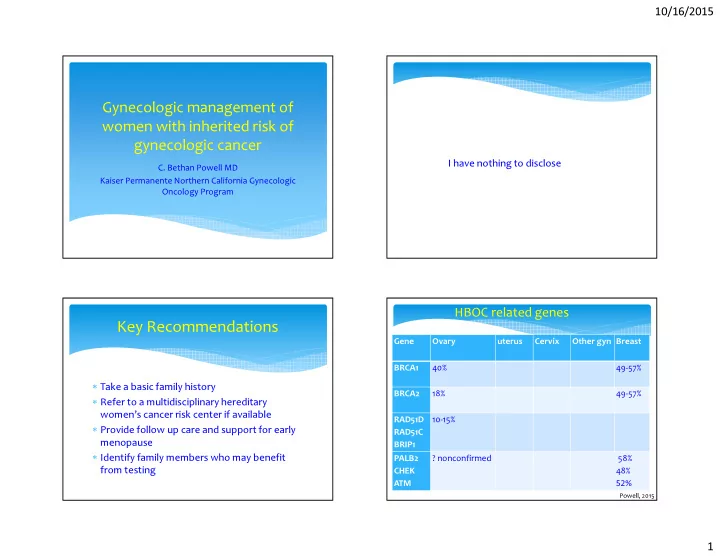
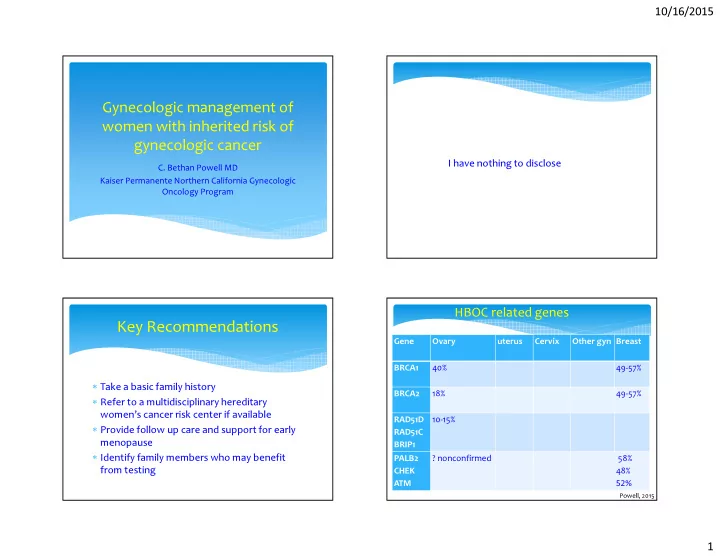
10/16/2015 Gynecologic management of women with inherited risk of gynecologic cancer I have nothing to disclose C. Bethan Powell MD Kaiser Permanente Northern California Gynecologic Oncology Program HBOC related genes Key Recommendations Gene Ovary uterus Cervix Other gyn Breast BRCA1 40% 49-57% ∗ Take a basic family history BRCA2 18% 49-57% ∗ Refer to a multidisciplinary hereditary women’s cancer risk center if available RAD51D 10-15% ∗ Provide follow up care and support for early RAD51C menopause BRIP1 ∗ Identify family members who may benefit PALB2 ? nonconfirmed 58% from testing CHEK 48% ATM 52% Powell, 2015 1
10/16/2015 Other genes associated with ovarian Ovarian and Breast Cancer risk by cancer gene and decade of life Gene Ovary uterus Cervix colon Breast MLH1 1 Lynch 20-54% 41% 4-20% Ovarian Cancer Risk Breast Cancer Risk MLH2 7.5-24% 21-49% 48% MSH6 0-13.5% 16-71% 12-31% At age 30 BRCA1 BRCA2 BRCA1 BRCA2 PMS 1 small 15% 15% Cowden PTEN 19-28% 50% By age 40 2.2% <1% 10% 6.6% Peutz- STK11/LKB1 21% 10% Jeghers Sex cord Adenoma By age 50 8.7% 2.4% 28% 20% stromal malignum tumors Other DICER1 Sertoli- By age 60 22% 7.4% 44% 35% leydig SMARCA4 By age 70 39% 16% 54% 45% Small cell carcinoma Powell, 2015 Chen, JCO 2007 Who Should be Considered for Hereditary Don’t be fooled Cancer Risk Assessment: HBOC Syndrome? ∗ Young age ∗ Families with few females ∗ Multigenerational cancers ∗ Families with females with early hysterectomy ∗ Personal history of non-mucinous ovarian cancer or breast cancer under age 50 ∗ Adoption ∗ Multiple cancers, bilateral breast ∗ Paternal as well as maternal history ∗ Male breast cancer ∗ Need to test an affected relative ∗ Ashkenazi Jewish 2
10/16/2015 Likelihood of being a BRCA carrier by American Women with Breast Cancer personal cancer history Non-Ashkenazi 2% ∗ Hispanic: 3.5% BRCA1 Breast cancer <10% ∗ US Ashkenazi Jews: 8.3% BRCA1 Breast cancer ∗ African American: 1.3% BRCA1 <40yrs ∗ African American, Ovarian cancer 10-15% with breast cancer age <35: Ashkenazi 10% 16.7% BRCA1 Breast cancer 30-35% ∗ Asian: 0.5% BRCA1 Breast cancer <40yrs 41% Ovarian cancer John, E JAMA: 2007, 2869 King et al 2003 Moslehi et al 2000 Malone et al 2006 and Papelard et al 2000 Strategies for ovarian cancer risk Pathologic Features of BRCA1 cancer reduction Woman with BRCA mutation ∗ Triple negative breast cancer: Surveillance Surgery < age 50, with any family history: 29% BRCA1 Chemopr evention < age 40: 23% BRCA1 ∗ Tubal cancer: 28% BRCA CA125, RRSO, OCPs Ultrasound salpingectomy, BTL ∗ Non-mucinous ovarian cancer: 16-21% BRCA Cass, I GynOnc, in press Lakhani, S Cl Can Res: 2005 3
10/16/2015 Lifestyle modification for ovarian Oral contraceptive pills cancer ∗ OR =0.58 (95% CL 0.46 to 0.73) Ovarian cancer risk reduction ∗ Risk reduction for BRCA1 and BRCA2 Parity > 4 ∗ Greater reduction of risk with years of use (3-6) breastfeeding ∗ No clear increased risk of breast cancer ?age< 25, BRCA1 No association ?prolonged use BMI, alcohol, age at menarche, ?increase in early breast cancer, in BRCA1 first birth under age 30 Moorman,JCO 2012 Iodice, Euro Jl of Cancer, 2010 Kostsopoulos, Breast Can Research 2014 Surveillance Tubal ligation ∗ UK Familial ovarian cancer screening study RR 0.43 in BRCA1 3563 women at 10% risk: annual CA 125 and ultrasound OR 0.39 in BRCA1 26% stage IIIC as compared with 86.7% in Risk reduction not confirmed in BRCA2 unscreened PPV 25.5% overall survival: 72 vs 48.4mo 60% of those with stage 1 had Lynch syndrome Antoniou, 2009 Narod, 2003 All screen negative cancers, were BRCA related Rosenthal, JCO 2013 4
10/16/2015 Surveillance: ROCA testing Symptom Diary ∗ Symptoms if occurring greater than 12 times in a ∗ Post-menopausal women, ave risk month were associated significantly with ∗ 4051 women, 11 year follow up ovarian cancer were ∗ CA 125 q 4mths, with ultrasound for abnormals. ∗ pelvic/abdominal pain, ∗ urinary urgency/frequency, ∗ PPV 40% ∗ increased abdominal size/bloating, ∗ difficulty eating/feeling full Goff, B Cancer 2007 Lu K, Cancer, 2013 Risk Reducing surgery: BSO RRSO: Breast cancer risk reduction ∗ 5783 women with BRCA1 or BRCA2 ∗ RRSO under age 40 ∗ 69% reduction all cause mortality OR = 0.44 BRCA1 ∗ 77% reduction in mortality, if no prior breast OR = 0.57 BRCA2 cancer ∗ Risk per year .9% brca1 peak 50-59 ∗ Risk per year .3% BRCA2 peak 60-69 Finch A, JCO 2014 Eisen A, JCO 2005 5
10/16/2015 Technique for risk reducing salpingo- Oophorectomy in women with BRCA1 and Risk of cancer at RRSO and after BRCA2 mutations: ∗ ∗ Laparoscopic ∗ Inspection of all peritoneal surfaces, diaphragm, liver and pelvic peritoneum ∗ 2035 cases ∗ Collection of peritoneal cytology ∗ 3.0% STIC ∗ resection of the entire ovary with a retroperitoneal approach, removing all adhesions with the adnexa, ∗ 2.7% invasive cancers resection of the tube as close to the uterus as possible and gentle handling of the specimen with removal in a endoscopic bag. Risk of peritoneal primary ∗ The entire tube and ovary should be submitted with micro-sectioning of the entire specimen in 2-3mm 3.9% BRCA1 cuts. 1.9% BRCA2 ∗ Attention in particular should be paid to the fimbria Finch A, and immunohistochemistry staining with Ki67 and P53 Powell, GO 2014 for confirmation of precursor lesions. 6
10/16/2015 SEE-FIM Protocol Sectioning of RRSO Specimens . Medeiros et al, Am J Surg Path, 2006 Should Hysterectomy be performed Salpingectomy in women with BRCA with RRSO? mutations ∗ CONS If a young woman is not ∗ PROS Increased risk, cost, ready for men0pause or Ensures removal of all tube hospitalization may even want the Simplifies hormonal No reports of cancer in possibility of a child management cornual portion of fallopian What about removing Increased risk of uterine tube the tube first and cancer with BRCA? and Endometrial cancer can be removing the ovaries at Tamoxifen detected in early stage with a later time? vaginal bleeding Other gyn pathology 7
10/16/2015 Salpingectomy Salpingectomy Technique Cons Pros ∗ Inspect entire abdomen • Two stages to surgery ∗ Avoid a portion of pelvic • Result in a delay of removing serous cancers ∗ Peritoneal cytology ∗ Avoid premature menopause the ovaries ∗ Remove adjacent ovarian capsule • May not be as effective as ∗ Option when patient will not agree to RRSO removing both tubes and ∗ Remove all the fimbria ovaries ∗ Maintain option for IVF ∗ Place in an endoscopic bag for removal • Removal of ovaries in young pregnancy BRCA carriers reduces breast ∗ Pathology processing with SEE-FIM protocol cancer by 50% HRT in women with BRCA mutations Long term health outcomes � Early menopause PROSE study: no impact on Breast cancer risk � Increase in osteopenia/osteoporosis –70% may reduce the protective effect of RRSO reduction still significant: HR 0.37 (CI 0.14-0.96) � Cardiovascular disease, hyperlipidemia – 30% 427 women with BRCA1 had no increased risk of breast � Sexual symptom, decreased pleasure and cancer on HRT, decreased risk on estrogen only satisfaction and increased dyspareunia. Rebbeck JCO 2005 Eisen JNCI 2008 8
10/16/2015 Recommendations after RRSO Recommendations after RRSO � Primary peritoneal cancer: ?annual pelvic exam Menopausal symptoms CA 125 q 6mths � Bone Health Hormone replacement therapy after BSO in women DXA scan at 2-3 years, then q 5 years without breast cancer, stopping by age 45-50. Weight bearing exercise Vitamin D 1000 IU and Calcium 1500mg � Cardiovascular disease Lipids q 1-3 years if no HRT and family history Fertility and reproduction New directions: Cascade Testing ∗ Premature ovarian failure ∗ Menopause at 48 vs 50 Challenges: how to identify and test ∗ Increased rate of premature menopause (under age 40) family members at risk ∗ Breast cancer ∗ Prenatal diagnosis: PGD for those undergoing IVF PND at 12-16 weeks gestation Finch, Fert Steril 2013 9
Recommend
More recommend