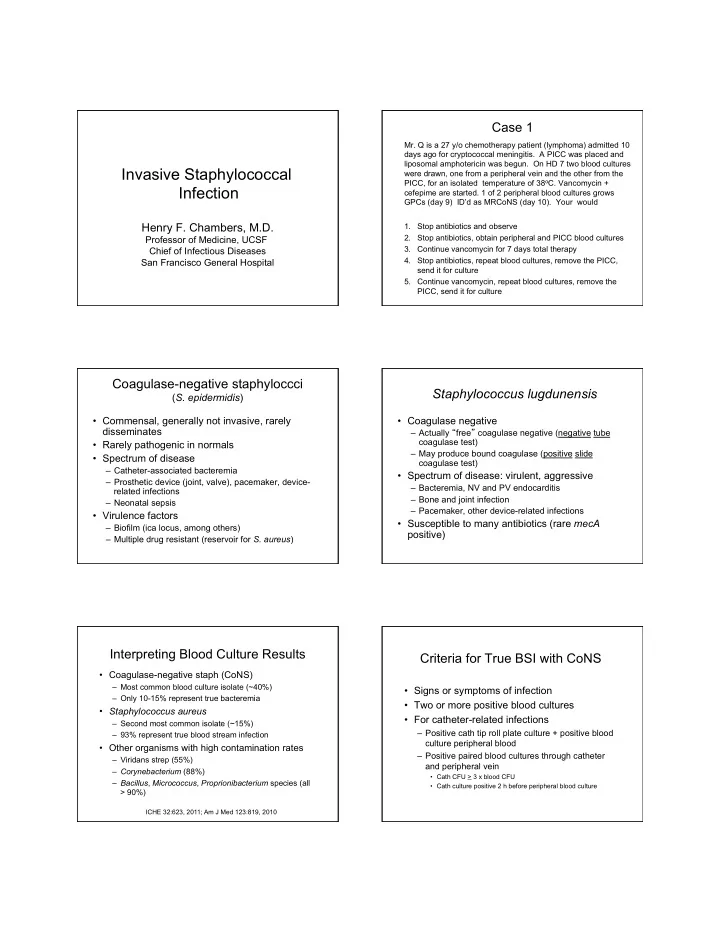
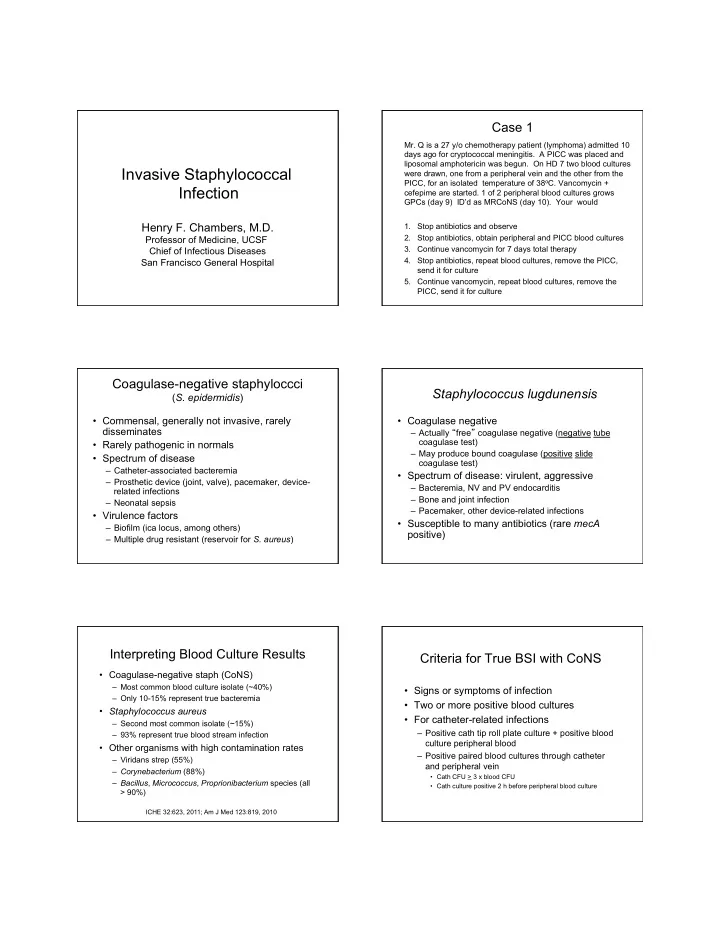
Case 1 Mr. Q is a 27 y/o chemotherapy patient (lymphoma) admitted 10 days ago for cryptococcal meningitis. A PICC was placed and liposomal amphotericin was begun. On HD 7 two blood cultures Invasive Staphylococcal were drawn, one from a peripheral vein and the other from the PICC, for an isolated temperature of 38 o C. Vancomycin + Infection cefepime are started. 1 of 2 peripheral blood cultures grows GPCs (day 9) ID’d as MRCoNS (day 10). Your would Henry F. Chambers, M.D. 1. Stop antibiotics and observe 2. Stop antibiotics, obtain peripheral and PICC blood cultures Professor of Medicine, UCSF 3. Continue vancomycin for 7 days total therapy Chief of Infectious Diseases 4. Stop antibiotics, repeat blood cultures, remove the PICC, San Francisco General Hospital send it for culture 5. Continue vancomycin, repeat blood cultures, remove the PICC, send it for culture Coagulase-negative staphyloccci Staphylococcus lugdunensis ( S. epidermidis ) • Commensal, generally not invasive, rarely • Coagulase negative disseminates – Actually “ free ” coagulase negative (negative tube coagulase test) • Rarely pathogenic in normals – May produce bound coagulase (positive slide • Spectrum of disease coagulase test) – Catheter-associated bacteremia • Spectrum of disease: virulent, aggressive – Prosthetic device (joint, valve), pacemaker, device- – Bacteremia, NV and PV endocarditis related infections – Bone and joint infection – Neonatal sepsis – Pacemaker, other device-related infections • Virulence factors • Susceptible to many antibiotics (rare mecA – Biofilm (ica locus, among others) positive) – Multiple drug resistant (reservoir for S. aureus ) Interpreting Blood Culture Results Criteria for True BSI with CoNS • Coagulase-negative staph (CoNS) – Most common blood culture isolate (~40%) • Signs or symptoms of infection – Only 10-15% represent true bacteremia • Two or more positive blood cultures • Staphylococcus aureus • For catheter-related infections – Second most common isolate (~15%) – Positive cath tip roll plate culture + positive blood – 93% represent true blood stream infection culture peripheral blood • Other organisms with high contamination rates – Positive paired blood cultures through catheter – Viridans strep (55%) and peripheral vein – Corynebacterium (88%) • Cath CFU > 3 x blood CFU – Bacillus , Micrococcus , Proprionibacterium species (all • Cath culture positive 2 h before peripheral blood culture > 90%) ICHE 32:623, 2011; Am J Med 123:819, 2010
Case 1 Therapy of CoNS BSI Mr. Q is a 27 y/o chemotherapy patient (lymphoma) admitted 10 days ago for cryptococcal meningitis. A PICC was placed and liposomal amphotericin was begun. On HD 7 two blood cultures • Antibiotic were drawn, one from a peripheral vein and the other from the – Empirical therapy: vancomycon PICC, for an isolated temperature of 38 o C. Vancomycin + – MRCS: vancomycin cefepime are started. 1 of 2 peripheral blood cultures grows GPCs (day 9) ID’d as MRCoNS (day 10). Your would – MSCS: beta-lactam • Duration 1. Stop antibiotics and observe – No therapy: line out, no hardware, intravascular 2. Stop antibiotics, obtain peripheral and PICC blood cultures device, pre-treatment blood cultures negative 3. Continue vancomycin for 7 days total therapy – 3-5 days* or 5-7 days: line out 4. Stop antibiotics, repeat blood cultures, remove the PICC, – 10-14 days: line in and in combo with lock therapy send it for culture 5. Continue vancomycin, repeat blood cultures, remove the *Int J Antimicrob Agents 34S:S47, 2009; Clin Infect Dis 49:1, 2009 PICC, send it for culture Types of S. aureus Diseases • Carriage (not a disease, normal flora) – 30% rate – Transmission by direct contact – Prevented by good hand washing • Spectrum of disease Invasive Staph. aureus – Local infection: abscess, cellulitis, folliculitis, impetigo Infection – Toxin-mediated disease • Staphylococcal food poisoning (preformed toxin, not an (Bacteremia in 75%) infection) • Toxic shock syndrome • Bullous impetigo, scalded skin syndrome – Invasive infection, sepsis: bacteremia, endocarditis, osteomyelitis, septic arthritis, pneumonia, complicated skin/soft tissue infections Case 2 Case 2 You would 38 y/o man, new CHF, alcoholic cardiomyopathy, 1. Continue vancomycin pending blood culture Hct = 13. He is transfused and on hospital day 3 results, d/c if those are negative. an upper + lower endoscopy performed. Post- 2. Switch from vancomycin to cefazolin pending procedure T = 38 o C. The site of the previous IV, d/ blood culture results, d/c if those are negative. c’d post-procedure is tender and red. Two 3. Continue vancomycin pending blood culture peripheral blood cultures are drawn. The next day results, plan to treat for at least 14 days if those he is afebrile and 1 blood culture is growing GPC in clusters. Cultures are repeated, and vancomycin are negative. is administered. The following day the organism is 4. Switch from vancomycin to cefazolin pending identified as MSSA and repeat blood cultures show blood culture results, plan to treat for at least 14 no growth to date. days.
Vancomycin vs. Beta-Lactams Cefazolin vs. Nafcillin Study Regimens compared Key findings Fowler, et al Vanco vs beta-lactam **Lower cure rate (62% vs Outcome Cefazolin (n=41) Nafcillin (n=41) P value (Clin Infect Dis 84%) with vanco Days resolution of 27: 478, 1998) 4.1 + 3.8 5.4 + 9.5 NS fever (mean + sd) **Higher death rate (12% vs 6%) with vanco Death or clinical 4 4 NS failure @ 4 wk (n) Schweizer. et al 30 mortality with MSSA for **Lowest mortality for 1 vs Death or clinical (BMC Infect Dis 2 vs 3 (3% vs. 7% vs 6 6 NS failure @ 12 wk (n) 11:279, 2011) 1. Naf or cefazolin 20%) vs Relapse @ 12 wk 1 1 NS 2. Vanco + naf or cefazolin **Naf vs vanco: Death @ 12 wk 1 5 0.22 vs adjusted HR=0.21 Rx stopped for 3. Vanco 0 7 0.02 **Switch to naf after vanco adverse drug event vs stay on vanco: adjusted HR=0.31 Antimicrob Agents Chemother 55:5122, 2011 Duration of Therapy: Predictors of Complicated S. aureus Bacteremia Staphylococcus aureus Bacteremia Duration Indications • Community-onset 14 days • Fever resolves by day 3 • Septic shock • Sterile blood culture after 2-3 days • Easily removed focus of infection • Persistent or secondary focus of infection • No metastatic infection (e.g., osteo) • Prolonged bacteremia on therapy (>48-72h) • Negative echo, no evidence of endocarditis • No predisposing valvular abnormalities • Fever > 3 days on therapy • No implanted prosthetic devices • Elderly patient (age > 60 years) • (No DM, immunosuppression) • MRSA 4-6 weeks • Failure to meet one or more of above criteria • Osteomyelitis, endocarditis, epidural • Use of vancomycin instead of a β -lactam abscess, septic arthritis (3 wk), pneumonia • Duration of treatment < 10-14 days (3-4 wk), complicated UTI Clin Infect Dis 49:1, 2009; Clin Infect Dis 52:285, 2011 Case 2 Case 2 You would 1. Continue vancomycin pending blood culture And if those blood cultures turn positive… results, d/c if those are negative. 2. Switch from vancomycin to cefazolin pending blood culture results, d/c if those are negative. – Obtain an ECHO 3. Continue vancomycin pending blood culture – Search for secondary or metastatic focus results, plan to treat for at least 14 days if those – Treat for a minimum of 4-6 weeks are negative. 4. Switch from vancomycin to cefazolin pending blood culture results, plan to treat for at least 14 days.
Recommend
More recommend