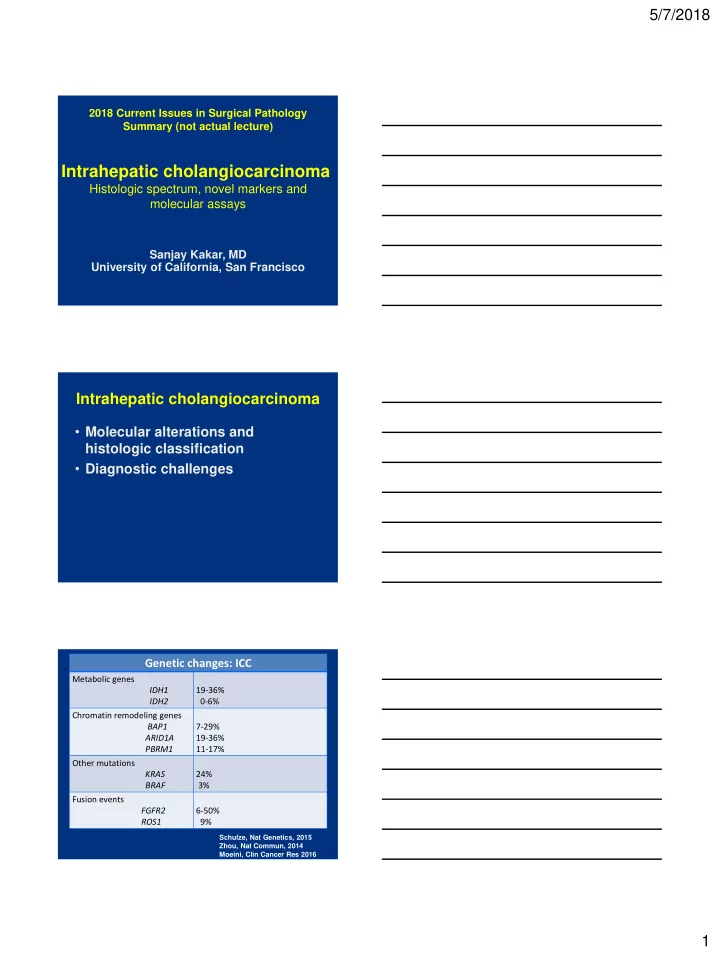
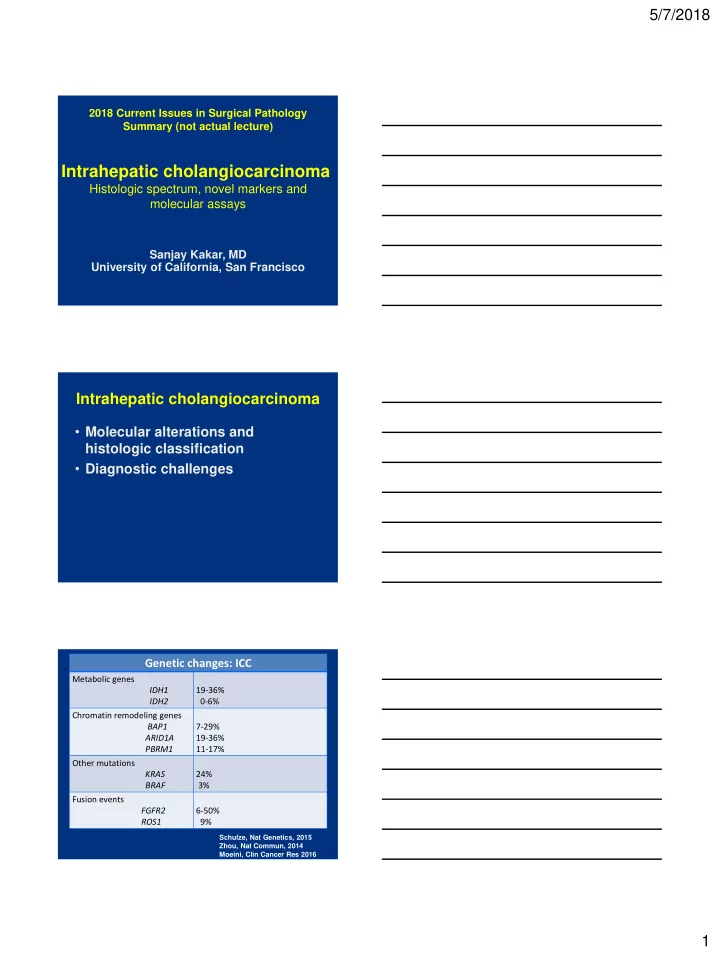
5/7/2018 2018 Current Issues in Surgical Pathology Summary (not actual lecture) Intrahepatic cholangiocarcinoma Histologic spectrum, novel markers and molecular assays Sanjay Kakar, MD University of California, San Francisco Intrahepatic cholangiocarcinoma • Molecular alterations and histologic classification • Diagnostic challenges Genetic changes: ICC Metabolic genes IDH1 19-36% IDH2 0-6% Chromatin remodeling genes BAP1 7-29% ARID1A 19-36% PBRM1 11-17% Other mutations KRAS 24% BRAF 3% Fusion events FGFR2 6-50% ROS1 9% Schulze, Nat Genetics, 2015 Zhou, Nat Commun, 2014 Moeini, Clin Cancer Res 2016 1
5/7/2018 ICC vs. HCC Genetic change Hepatocellular Intrahepatic carcinoma cholangiocarcinoma β -catenin mutation 20-30% Uncommon TERT promoter 30-50% Rare mutation IDH mutations Rare 19-36% PBRM1 mutation Absent FGFR2 fusion Absent 6-50% ICC vs. metastatic adenocarcinoma Genetic ICC Biliary GB PDAC Eso/Gastric change AC IDH 19-36% 0-7% 0 0 0 mutations BAP1 7-29% 0-10% 0 <1% 3% mutation PBRM1 11-17% 5% 20% 4-6% 0 mutation SMAD4 0-4% 10-25% 0 35-60% 8% mutation FGFR2 6-50% 0-5% 20% 0 2-9% fusion Intrahepatic cholangiocarcinoma Histologic classification Adenocarcinoma Well-differentiated Moderately-differentiated Poorly-differentiated Histologic subtypes Mucinous Signet ring Clear cell Lymphoepithelioma-like Sarcomatoid Adenosquamous Squamous 2
5/7/2018 Intrahepatic cholangiocarcinoma Proposed classification #1 Classification based on size of glands Large duct type Located close to hilum (Mucin-ICC) Glands typically large Mucin-positive Small duct-type Located at periphery (Mixed-ICC) Glands typically small Mucin-negative Cholangiolocellular Ductular reaction-like pattern Komuta, Hepatol 2012 Intrahepatic cholangiocarcinoma Proposed classification #2 Classification #2 Conventional ICC With biliary features Unconventional ICC Trabecular subtype Hilar subtype With predominant ductal plate malformation Cholangiolocellular Intraductal neoplasia Intraductal papillary neoplasm Intraductal tubulopapillary neoplasm Sempoux, Sem Liv Dis 2011 Intrahepatic cholangiocarcinoma • Molecular alterations and histologic classification • Diagnostic challenges 3
5/7/2018 Intrahepatic cholangiocarcinoma Diagnostic challenges Well-differentiated • BDA vs adenocarcinoma Adenocarcinoma: any differentiation • ICC vs metastatic adenocarcinoma Poorly differentiated • Hepatocellular carcinoma Well-differentiated Frozen section diagnosis • Metastatic adenocarcinoma • Benign biliary proliferation: Bile duct adenoma or hamartoma Benign biliary lesions Biliary hamartoma (von Meyenburg complex) • Dilated ducts with curvilinear outlines • Inspissated bile Bile duct adenoma • Compact small to medium sized glands • Round to oval contours, not dilated • Scant stroma if small, larger lesions can have prominent stroma 4
5/7/2018 Biliary Bile duct hamartoma adenoma Glands Dilated ducts with Compact small to medium curvilinear outlines sized glands Stroma Can be prominent Scant in small lesions, can be prominent in large lesions Bile or Often present Absent eosinophilic material Bile duct adenoma Adenocarcinoma Growth -Well-demarcated at -Destructive growth pattern interface -Grow around portal -Portal invasion tracts Stroma Typically collagenized in Desmoplastic center, can be cellular Cytologic Mild Mild to marked atypia Architecture Tubular glands, can be Can be complex angulated Mitoses Absent Can be present Bile duct adenoma Challenging features • Atypia enhanced by frozen artifact • Angulated infiltrative glands • Mucin can be present • Stroma may simulate desmoplasia • Variant histologic features 5
5/7/2018 Bile duct adenoma Variant features • Clear cell change • Oncocytic change • Alpha-1-antitrypsin globules • Granulomas Bile duct adenoma Benign neoplasm or reactive process • Reactive proliferation related to prior injury • Peribiliary gland hamartoma • Benign neoplasm Bile duct adenoma Study Result Pujals, Hepatology 53% had BRAF V600E mutation 2015 Pujals, Histopathol 53% positive for VE1 antibody by 2015 immunohistochemistry Angkathunyakul, 87.5% had BRAF V600E mutation Histopathol 2017 6
5/7/2018 BRAF mutation in ICC Study Result Goeppert, Mod ICC: 5/159 (3%) Pathol 2014 Extrahepatic biliary, GB: negative Zhu, Ann Surg ICC: 4.9% Oncol 2014 Lee, JCP 2016 Extrahepatic biliary: 1% BDA vs adenocarcinoma Immunohistochemistry: p53, Ki-67 IHC Result p53 35% ICC Strong diffuse 60% metastatic PDAC staining None: bile duct adenoma (patchy weak to moderate staining) Ki-67 index ICC: 88.5% (mean >20%) >10% BDA: none (mean 2%) Tan, AIMM 2004 Hornick, AJSP 2005 Tsokos/Gill, Histopathol 2016 BDA vs adenocarcinoma Immunohistochemistry: Other assays IHC Result DPC4 loss ICC: 5-10%; metastatic PDAC 50-60% BDA: none Mesothelin Metastatic PDAC: 64% BDA: none mCEA Metastatic PDAC: 92% BDA: none BAP1 loss ICC: 20-30% BDA: none (limited experience) Albumin ISH Metastatic PDAC: none BDA: Positive Hornick, AJSP 2005 Arora, Histopathol 2016 Misumi, Histopathol 2017 7
5/7/2018 Cholangiolocellular carcinoma Histologic criteria for diagnosis Study Microscopic Description Inconsistencies • small tubular or acinar or Kozaka, 2007 Some studies : • Small tubular glands enough cord-like structures, resembling reactive bile for diagnosis, did not require ductules branching configuration Some studies : Komuta, 2008 • small monotonous glands • CCC divided into well, • antler-like anastomosing moderate and poorly patterns differentiated categories • abundant hyalinized and/or edematous fibrous stroma • glands strongly embedded Moeini, 2017 in fibrous stroma • cuboidal to low columnar Rhee, 2018 cells with scanty eosinophilic or amphophilic cytoplasm • small monotonous glands CCC: ‘stem cell’ features? Study Stem Cell Markers • NCAM (CD56): 75% Kozaka, 2007 • NCAM in 87% Komuta, 2008 • CD133, c-kit, OCT4 • SALL4: 75% Moeini, 2017 • NCAM:100% • No difference in stem cell marker staining Rhee, 2018 compared to intrahepatic cholangioCA Cholangiolocellular carcinoma 8
5/7/2018 Cholangiolocellular carcinoma Well-differentiated ICC CD56 in CCC positive and negative case EMA in CCC Luminal and cytoplasmic EMA per literature • Luminal staining in CCC • Cytoplasmic staining in ICC Komuta, Hepatol 2012 Kondo, Int Med 2015 9
5/7/2018 Adenocarcinoma Any differentiation ICC vs metastatic adenocarcinoma • Pancreas, biliary tree • Upper GI ICC vs PDAC Immunohistochemistry: not widely studied Diagnosis IHC results ICC S100P- pVHL+ MUC5AC- CK17- PDAC S100P+ pVHL- MUC5AC+ CK17+ Lok, Hum Pathol 2014 ICC vs PDAC Other assays Diagnosis IHC results ICC BAP1 loss Albumin ISH positive PDAC BAP1 intact Albumin ISH negative 10
5/7/2018 BAP1: loss in tumor cells BAP1 loss Poorly differentiated ICC vs HCC • ICC with solid/trabecular growth pattern • Scirrhous HCC • Combined HCC-cholangiocarcinoma 11
5/7/2018 Cholangiocarcinoma HCC-like area HCC-like area CK19+ (Arg neg) Scirrhous HCC 12
5/7/2018 Hep Par, pCEA MOC31 Scirrhous HCC: Atypical features • Atypical radiologic features • Abundant stroma • Immunophenotypic features Negative: Hep Par 1, pCEA Positive: MOC31, CK19 GPC-3 CK19 13
5/7/2018 Stain Scirrhous HCC Conventional HCC Hep Par 1 17-20% 80-90% pCEA 33% 60-80% CK7 58-65% 0-20% CK19 50% 0-10% MOC31 64% 5-11% Arginase-1 95% 95% Glypican-3 95% 70-80% Matsuura, Histopath, 2005 Krings/Kakar, Mod Pathol 2013 Combined HCC-CC HCC • Morphology, arginase-1 • CK19: can be positive CC • Discrete glands, mucin + • Negative arginase-1 • CK7, CK19 and/or MOC31 HCC-like area Well-formed glands 14
5/7/2018 Arginase-1 CK19 Arginase-1 CK19 Intrahepatic cholangiocarcinoma AJCC 8 th edition T category Definition T1 T1a: Solitary tumor <5 cm without vascular invasion T1b: Solitary tumor >5 cm without vascular invasion T2 Solitary tumor with intrahepatic vascular invasion, or multiple tumors, with or without vascular invasion T3 Tumor perforates visceral peritoneum T4 Tumor involving local extrahepatic structures by direct invasion 15
5/7/2018 Intrahepatic cholangiocarcinoma AJCC 7 th edition T category Definition T1 Solitary tumor without vascular invasion T2 T2a: Solitary with vascular invasion T2b: Multiple tumors T3 Involving visceral peritoneum or direct invasion into extrahepatic structures T4 Tumor with periductal invasion Periductal invasion • Intrahepatic CC, macroscopic types Mass forming, periductal, intraductal, mixed • Periductal: worse prognosis Extensive intraductal growth: T4 • Problems How extensive is 'extensive' Recent studies do not confirm worse outcome Hirohashi, Hepatogastroeterol 2002 Uno, Surg Today, 2012 Periductal growth pattern 16
Recommend
More recommend