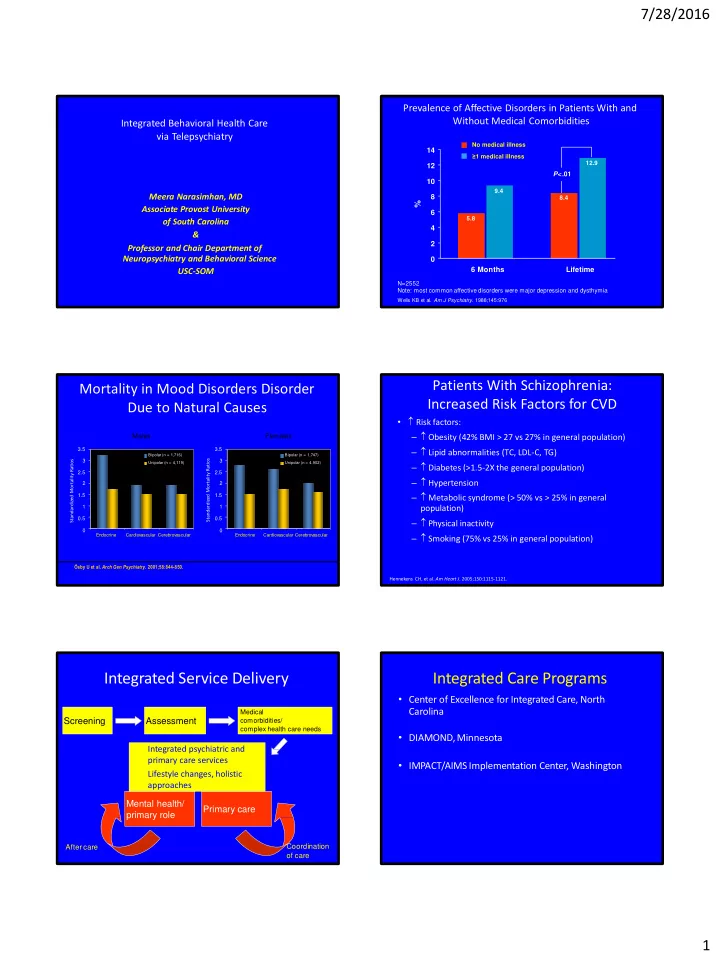
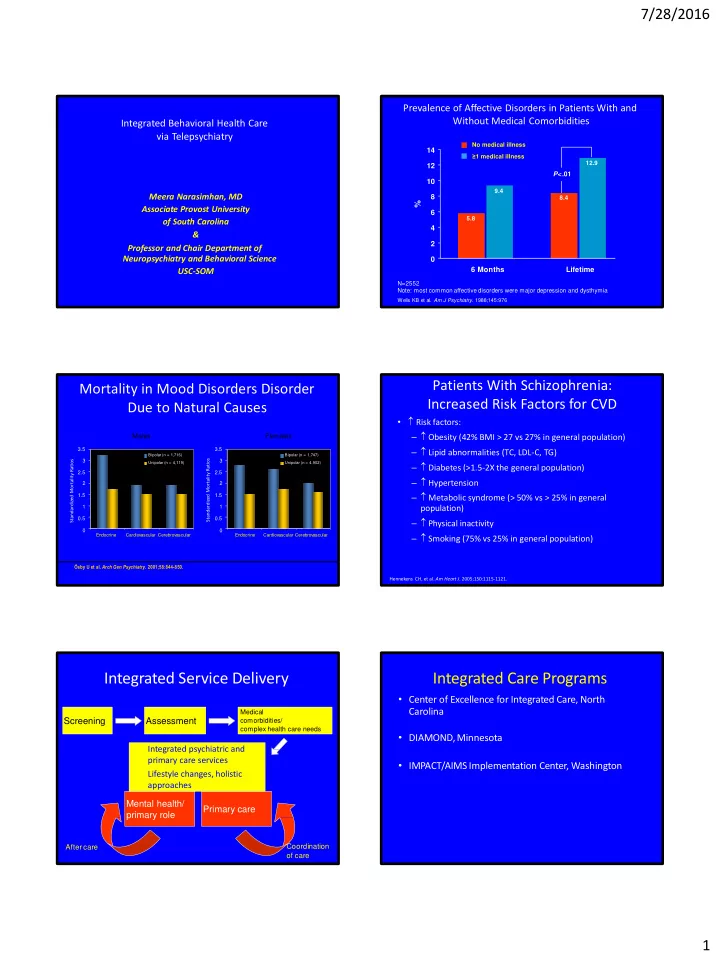
7/28/2016 Prevalence of Affective Disorders in Patients With and Without Medical Comorbidities Integrated Behavioral Health Care via Telepsychiatry No medical illness 14 ≥ 1 medical illness 12.9 12 P <.01 10 9.4 Meera Narasimhan, MD 8 8.4 % Associate Provost University 6 5.8 of South Carolina 4 & 2 Professor and Chair Department of Neuropsychiatry and Behavioral Science 0 6 Months Lifetime USC-SOM N=2552 Note: most common affective disorders were major depression and dysthymia Wells KB et al. Am J Psychiatry . 1988;145:976 Patients With Schizophrenia: Mortality in Mood Disorders Disorder Increased Risk Factors for CVD Due to Natural Causes • Risk factors: – Obesity (42% BMI > 27 vs 27% in general population) Males Females – Lipid abnormalities (TC, LDL-C, TG) 3.5 3.5 Bipolar (n = 1,716) Bipolar (n = 1,747) Standardized Mortality Ratios Standardized Mortality Ratios 3 3 Unipolar (n = 4,119) Unipolar (n = 4,902) – Diabetes (>1.5-2X the general population) 2.5 2.5 – Hypertension 2 2 – Metabolic syndrome (> 50% vs > 25% in general 1.5 1.5 1 1 population) 0.5 0.5 – Physical inactivity 0 0 Endocrine Cardiovascular Cerebrovascular Endocrine Cardiovascular Cerebrovascular – Smoking (75% vs 25% in general population) Ő sby U et al. Arch Gen Psychiatry . 2001;58:844-850. Hennekens CH, et al. Am Heart J . 2005;150:1115-1121. Integrated Service Delivery Integrated Care Programs • Center of Excellence for Integrated Care, North Carolina Medical Screening Assessment comorbidities/ complex health care needs • DIAMOND, Minnesota Integrated psychiatric and primary care services • IMPACT/AIMS Implementation Center, Washington Lifestyle changes, holistic approaches Mental health/ Primary care primary role After care Coordination of care 1
7/28/2016 T elepsychiatry – Overview Barrier to Care • Shortage of Mental Health Providers • Access to optimal mental health care 1,2 • Rural Counties: transportation, costs • Reduce health disparities 3 • Social determinants, minority, rural counties • Time constraints • Offers a host of benefits • Several challenges: licensure, state regulations • Attitude and stigma Thomas KC, et al. Psychiatr Serv . 2009;60:1323‐ 1328. Mohr DC, et al . Ann Behav Med . 2006;32:254-258. Grady B, et al. Telemed J E Health. 2011;17:131-148 Psychiatry Tele mental health or Telepsychiatry • Telemedicine refers communications technologies and electronic information to Psychoanalysis provide and support health care when Implementation Psychopharma Improvement distance separates the participants Science cology Science Digital • It has applications in clinical care, education and research Personalized Medicine • Reduce health disparities in patient & Population Health Benefits of T elepsychiatry Various Clinical Settings • Inpatient • Telepsychiatry may be a feasible means to deliver psychotherapy and pharmacotherapy. • Outpatient • Veterans Administration • Improves access to care in rural, underserved areas, reduce cost over time, decreased costs for patients and systems. • Correctional Facilities Lower attrition rate and similar levels of patient satisfaction as • Nursing Homes compared to person • Primary Care Clinics • Home Based Jenkins-Guarnieri MA, et al. Telemed J E Health . 2015;21:652-660. Mohr DC, et al. JAMA . 2012;307:2278-2285. Leigh H, et al . J Telemed Telecare . 2009;15:286-289. • Rural Settings 2
7/28/2016 Considerations for Telepsychiatry Reimbursement Policy for Telehealth Implementation • Technological competence • • Licensure and other liability issues • HIPAA compliance, and disclaimer language • Confidentiality and security measures • Reimbursement • Data storage and technical issues • Management of emergent situations and safety protocols • Therapeutic alliance • State policies for telemental health vary in specificity and scope • Acceptance by providers – Map represents state rankings for Medicaid coverage of mental and behavioral health services provided via telemedicine, based on scope and conditions of payment Thomas L, et al. http://www.americantelemed.org/policy/state-policy- resource-center. Accessed February 11, 2016. PRIMARY STROKE CENTER T elehealth • Tele Stroke Network • TeleID • Telepsychiatry The REACH Virtual & Collaborative Healthcare Model – Clinical Workload Balance TelePSYCHIATRY Hub A New Frontier in Tertiary Medical or Referral Hospital Improving Access, Affordability, Efficiency, Costs and Clinical Outcomes Spoke Cart* CT scanner Physician Internet access Laptop/PC Standard Web cam Internet access * Recommended/provided by REACH 3
7/28/2016 All Maine & South Carolina ER Visits per Thousand Members in Group per Year (ME/SC Study 5000 4000 3910 3000 3011 2000 1730 1680 1000 1394 1123 880 615 0 MH Dx SA Dx MH & SA Dx No MH/SA Dx Maine SC NRI Presentation 20 20 April 13-16, 2009 A Deeper Look at Medical The Uniqueness of the Telepsychiatry Co-morbidities – South Carolina Project • Largest ED telepsychiatry project in the nation!!! Cardiometabolic Risk • 30,000 patients in 22 ED, 3 more coming on board 20% 18.6% • Public, private and academic partnership. 15% 17.0% 13.5% 13.6% 12.1% 13.6% 10% • Policy Practice and Research 7.8% 8.7% 8.6% 7.7% 5% 5.7% 4.7% • Data warehouse all-payer state database in healthcare. 0% Diabetes Lipidosis Other Nutritional Hypertention • Opportunity to rigorously study the impact of this novel (includes obesity) intervention on outcomes None Non DMH-MH DMH-MH • Contextual factors that may allow the program to be disseminated to other states. Narasimhan et al, NASMHPD Research Institute, 2009 Outcomes • Lower rates of inpatient admission from the ED in the 30 days after telepsychiatry compared to the ED encounters with no Quality, Utilization, tEconomic Impact telepsychiatry (8% vs 19%; p< 0.01) • Shorter lengths of stay than those in the control group (4.1 and Sustainbility of Telepsychiatry, Aim 2: To examine the individual, ED, and community-level days vs. 6.2; p < 0.01 days for any hospitalization) and • 30 day outpatient follow-up than patients who received no moderators of the telehealth program. telepsychiatry (38% vs. 13%; P < 0.01) and (National Institute of Mental Health • 90 day follow-up than those who received no telepsychiatry funded R01) (46% vs. 17%; P < 0.01). Aim 3: To conduct a budget imanalysis Aim 1: To examine the impact of telehealth on access and quality of mental health care at both an individual and Emergency Department levels ( LOS, hospitalization and 30 day follow-up). 4
7/28/2016 Staff and Physician Perceptions of Telepsychiatry Patient Perceptions of Telepsychiatry Program Program 1 0 0 % 100% 8 9 .5% 9 0 % 90% 81.8% 80.4% 84.3% 84.1% 8 0 % 80% 77.1% 7 0 % 70% 6 0 % 60% 5 0 % 50% 4 0 % 40% S atisfaction w ith E fficie n t U se o f C o m fort w ith Im proved P atie n t Satisfaction with Satisfaction with Te c h no logy Tim e Tele p s ychiatry C are a n d Services Process S ervices Successful Integrated Models Summary • Telepsychiatry may improve access to mental Telehealth health care 1 and offer multiple benefits Primary Provider • Telepsychiatry may be acceptable for use among Health Coach patients within several psychiatric settings. Patient • Telepsychiatry is a feasible for use among various Centerednesss iPad underserved patient populations Integration Other Digital technologies • Telepsychiatry may offer advantages to all stakeholders in the service and delivery of mental health care, ie, patients, providers, and payors Health apps Specialty Care 27 5
Recommend
More recommend