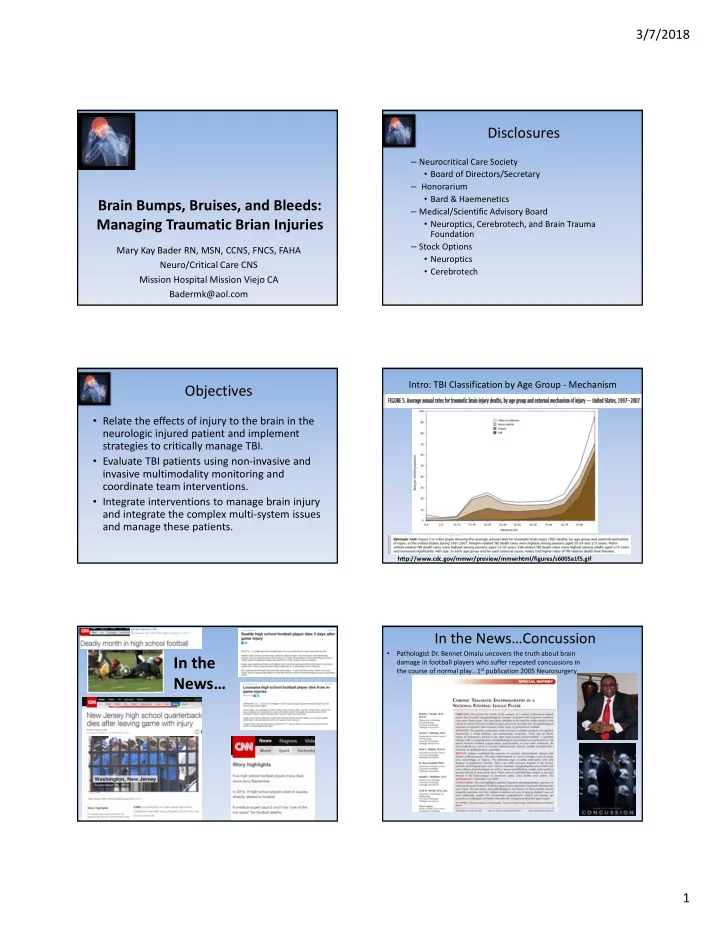
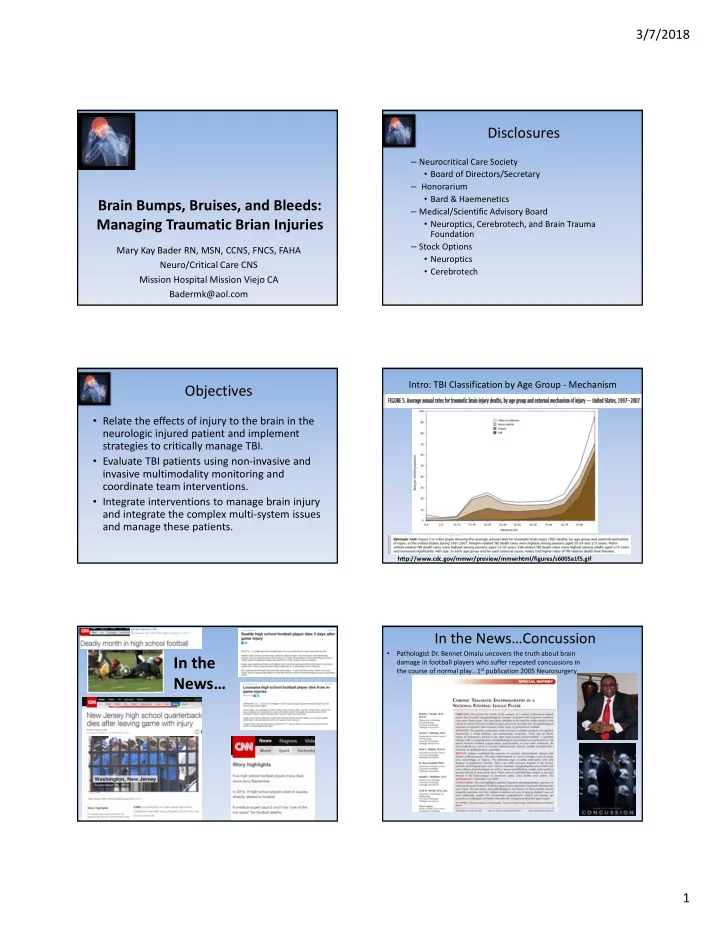
3/7/2018 Disclosures – Neurocritical Care Society • Board of Directors/Secretary – Honorarium • Bard & Haemenetics Brain Bumps, Bruises, and Bleeds: – Medical/Scientific Advisory Board Managing Traumatic Brian Injuries • Neuroptics, Cerebrotech, and Brain Trauma Foundation – Stock Options Mary Kay Bader RN, MSN, CCNS, FNCS, FAHA • Neuroptics Neuro/Critical Care CNS • Cerebrotech Mission Hospital Mission Viejo CA Badermk@aol.com Intro: TBI Classification by Age Group ‐ Mechanism Objectives • Relate the effects of injury to the brain in the neurologic injured patient and implement strategies to critically manage TBI. • Evaluate TBI patients using non ‐ invasive and invasive multimodality monitoring and coordinate team interventions. • Integrate interventions to manage brain injury and integrate the complex multi ‐ system issues and manage these patients. http://www.cdc.gov/mmwr/preview/mmwrhtml/figures/s6005a1f5.gif In the News…Concussion • Pathologist Dr. Bennet Omalu uncovers the truth about brain In the damage in football players who suffer repeated concussions in the course of normal play…1 st publication 2005 Neurosurgery News… 1
3/7/2018 Chronic Traumatic Encephalopathy Chronic Traumatic Encephalopathy (CTE) is a CDC Definition of TBI progressive degenerative disease of the brain found in athletes (and others) with a history of repetitive brain trauma. This trauma, which includes multiple concussions, triggers progressive degeneration of the brain tissue, including the build ‐ up of an abnormal protein called tau. These changes in the brain can begin months, years, or even decades after the last concussion or end of active athletic involvement. The brain degeneration is associated with memory loss, confusion, Junior Seau impaired judgment, paranoia, impulse IMPACT OF control problems, aggression, depression, and, eventually, progressive dementia. MULTIPLE MINOR CTE can only be definitively diagnosed through post ‐ mortem examination of the BUMPS ON THE brain, although efforts are underway to learn how to diagnose CTE in living people, a BRAIN? key step to developing a treatment for the disease. Dave Duerson. who committed suicide in February, had evidence of chronic traumatic encephalopathy Classification of Head Injury: TBI Impact Presentation National TBI Estimates. *The number of people with TBI who are not seen in an emergency department or who receive no care is unknown. Source: CDC Case Study • Nurse K ‐ 39 year old female (Trauma Nurse) What types of Brain Injury are • Mechanism – Patient was driver, rear ended, + seatbelt, airbag deployment, you most concerned about? experienced brief LOC – Other vehicle driver who caused the MVA was texting, with her child in the backseat. 2
3/7/2018 Hospital Course • ER Phase ‐ 1st VS: 153/90, HR 126, RR 26, NRB, T 98.5, GCS= 14 • CT Brain, C Spine, MRI = Negative • Admit for observation • Failed Cognition Evaluation Mild TBI • D/c home with PT/ST • Injury Severity Score (ISS range 1 ‐ 75)= 5 an anatomically based consensus ‐ derived 80 ‐ 90 % of all TBI is Mild! global severity scoring system that classifies each injury in every body region according to its relative severity. (head & neck) • 0.996= Probability of Survival Score TRISS determines the probability of survival, of a trauma patient, from the ISS + a Revised Trauma Score. Facts and Stats Mild TBI: Concussion • Mild traumatic brain injury (mTBI) is defined as an acute • Estimates of mild traumatic brain injury (mTBI) impact 2.5 million brain injury resulting from mechanical energy to the head affected individuals annually in the United States, many of whom from external physical forces which result in a complex do not obtain immediate medical attention (CDC 2015) pathophysiologic process inducing biochemical changes in • Approximately 2 million emergency department (ED) visits occur in the brain the United States annually for TBI (CDC 2015) – only 56% of these are recognized at mTBI – The injury produced results in a functional disturbance in brain • The incidence of clinician ‐ confirmed TBI in U.S. soldiers returning function without typical structural findings indicative of injury (CT from Iraq and Afghanistan is reported to be approximately 23%, or MRI). where the majority are MTBI (Terrio et al., 2009). – mTBI is composed of physical, cognitive, emotional, and sleep ‐ • 2% of US population live with TBI caused disabilities related symptoms. • Economic impact: $77 billion per year (CDC 2015, Faul et al 2010) – The impact on the patient may last minutes to months. References: Christopher C. Giza, Jeffrey S. Kutcher, Stephen Ashwal, et al. Neurology 2013;80;2250 ‐ 2257; Mild TBI Guidelines AANN); & Faul M, Xu L, Wald MM, Coronado VG. Traumatic brain injury in the United States: emergency department visits, hospitalizations, and deaths 2002–2006. Atlanta (GA): US Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, 2010: 1–71 Anatomical Timeline of a Concussion Pathophysiology Defining the Key Factors • Primary injury: – Concussion is always a primary injury as is the initial neurological insult. While the primary event cannot be changed, steps can be taken to prevent secondary injury. 3
3/7/2018 Progressive Biomechanical Changes • Secondary injury ensues – hours to days – Complex neuro inflammatory changes • Abrupt, massive depolarization of neuronal, glial, and endothelial cells of the cerebral vessels • Release excitatory neuro transmitters, ionic shifts, altered glucose metabolism, and CBF and impaired axonal function • Excessive Ca influx ‐ damage axonal exoskeleton creating axonal disconnection • Neuronal apoptosis and programmed cell death occur – Danger: Second impact syndrome can occur if another CLINICAL GUIDELINES PUBLISHED impact to the brain occurs in the immediate period (hours to few weeks) following the initial injury (primarily reported in children and young adults). • Blow results in neuro inflammatory response—massive cerebral edema and rapid rise in ICP Eastern Association for the Surgery of Eastern Association for the Surgery of Trauma Practice Guidelines: Mild TBI Trauma Practice Guidelines: Mild TBI • Mild TBI defined • Recommendations Radiographic Study – Acute alteration in brain function caused by a – Clinicians should perform brain CT scan on blunt external force and is characterized by patients with suspected brain injury (II) • GCS 13 ‐ 15 – If CT resources limited, use set of criteria to • Loss of consciousness for 30 minutes or less determine which patients get a CT (II) • Duration of post traumatic amnesia < 24 hours. – Clinicians should not routinely use MRI, PEAT or – CT brain normal NMR in management of patients at present (III) Eastern Association for the Surgery of Eastern Association for the Surgery of Trauma Practice Guidelines: Mild TBI Trauma Practice Guidelines: Mild TBI • Recommendations • Recommendations – Patients with isolated TBI and negative CT brain – Ability to operate motor vehicles safely may be • d/c from ED if no other injuries requiring admit (III) impaired for a variable length of time in patients – Patients taking warfarin presenting with mild TBI should with MTBI. Individualize resumption of driving (III) have their INR evaluated (III) – Timing return to work individualized with formal – Anti ‐ coagulated pa � ents with ↑ INR and normal CT neuropsychologic testing considered (III) remain a significant risk for interval development of ICH and should be admitted for observations (III) – Biochemical markers such as S100B, neuron specific enolase, and serum tau should not be – Patients may be advised that measurable deficits in cognition/memory usually resolve at 1 month but 20 ‐ 40% routinely used in clinical management except in of cases, post ‐ concussive symptoms may present for 3 context of research protocol (III) months or longer (III) 4
3/7/2018 TQIP Guidelines Focus Severe TBI • Section on Elderly Patients with TBI – Often present with GCS 13 ‐ 15 and appear mild in nature due to brain atrophy – Neuro evaluation more complicated due to dementia, cognitive decline, and hearing/visual deficits • Determine baseline from family – Anti ‐ coagulants/Anti ‐ platelet medications exacerbate TQIP GUIDELINES sequalae of TBI • Reversal is important to remember ACS – Older age carries higher mortality and worse functional outcome How do we detect mild TBI? Scene Evidence Based Literature: Assessment Significant Variables associated with Mild TBI • Sports Related – Pre ‐ season: IMPACT Testing – AT event: • LOC: – Assess ABCs & Maintain Spine Precautions – Assess GCS and Pupils – Transport to ED • Absolute prevalence of symptoms (50%) • NO LOC – Athlete is removed from game and not allowed to return to play that day associated with concussion: – Sideline Assessment » SCAT 2 or similar – Headache, dizziness, blurred vision and nausea » Balance Error Scoring System (BESS) • Follow ‐ up – Post Game: • Medical Clearance » Parent Education • Retesting IMPACT » Cognitive Rest until symptom free • Teacher alert » Tylenol – no Advil » Sleep and Quick Checks 5
Recommend
More recommend