In-depth cholera epidemiological study of Cholera in Zimbabwe Epidemiological study of cholera hotspots and epidemiological basins in East and Southern Africa
Prospective Cooperation Cholera Team Cholera specialist Bio-statistic specialist Epidemiologist & Project coordination biologist Senior infectious Infectious disease Senior epidemiologist Field epidemiologist & disease specialist & specialist & epidemiologist WaSH engineer microbiologist 2
Background Cholera burden • Cholera epidemics remain a public health concern in East and Southern Africa - Approx. 634,000 cases/14,303 deaths (CFR of 2.3%) between 2007-2016 • The brunt of the cholera burden affects a small number of specific zones and communities: “cholera hotspots” targeted approach (Cf. Ending Cholera Roadmap) Control and Prevention • Cholera can be eliminated where access to WASH services are ensured • Oral cholera vaccine can help provide protection for a population while sustainable WASH interventions are being implemented Challenges for sustainable intervention in cholera high-risk areas • Communities in cholera hotspots are often neglected by WASH development programs, as WASH sector objectives are coverage (and not health) driven • Lack of common understanding and knowledge about priority areas • Lack of donor investment in cholera hotspots 3
UNICEF Strategic Framework in Eastern and Southern Africa Implementation of the framework hinges on epidemiological studies focused on identifying areas regularly affected by cholera outbreaks 1 Development of national and subnational plans 2 Well-targeted capacity development Local-scale social and behaviour change communication 3 4 Information management for improved monitoring and action 5 Regional coordination and greater cross-border collaboration 6 Knowledge management and operational research 7 Partnerships, public advocacy, social movements and influencers 4
Study region and timeline • Greater Horn of Africa : Study results by Oct 2018 • Zambesi Basin: Study results by Oct 2018 5
Study objectives • To better understand the local dynamics of cholera at a national and regional level – Apply an approach combining field research, epidemiology and genetic analysis of clinical isolates of Vibrio cholerae • To identify cholera hotspots as well as high-risk populations and practices for targeted emergency and prevention programs • To establish effective strategies to combat cholera in Zimbabwe and neighboring countries
Methods (1/2) • Cholera case definition (Ministry of Health) Suspected case: – In a patient age five years or more, severe dehydration or death from acute watery diarrhea in an area where there is no cholera. – In the context of a cholera epidemic, a suspected case is any person age two years or more with acute watery diarrhea, with or without vomiting . Confirmed case: – A suspected case in which Vibrio cholerae serogroups O1 or O139 has been isolated from stool samples. • Cholera cases and deaths (Ministry of Health, WHO) – Total number of cases/deaths per district for 1998-2002 and 2004-2006 – Weekly time series of cholera cases and deaths per district for 2003 and 2007- 2018 (missing weekly data for 2015). • GIS shape files, background layers (UNOCHA) • Population data from ZIMSTAT 2012 census with a population growth factor derived from the National Health Profile 2014 • Rainfall data estimated from daily TRMM Multi-Satellite Precipitation Analysis remote sensing products 7
Methods (2/2) • Data Analysis Process – Data cleaning and quality assessment, including missing data and outlier detection – Smoothing and interpolation procedure – Patterns of sporadic cases were removed (e.g., a single case or two to three cases without reported cases during the two weeks before and after). – Two successive outbreaks separated by an inter-epidemic period equal to or greater than six weeks were considered as two separate events. – Outbreak: extraction of the key epidemiological features per outbreak event (onset, peak, duration, incidence, case fatality rate, inter-epidemic period) – Hotspot classification according to recurrence, duration and intensity of cholera outbreaks – Interpretation of the results according to local contexts (literature and national expertise) 8
Dynamics of recent cholera outbreaks 9
Dynamics of recent cholera outbreaks 10
Overview of cholera outbreaks between 1998-2018 • Since 1998, cholera cases have been reported in Zimbabwe almost every year, with the exception of 2014 and 2017 • Cholera is often reported along the Mozambican and Zambian border • Major outbreaks in 2008-2009 affected the capital city and almost all provinces due to a concomitant severe economic crisis, which led to widespread disruption of environmental and health services • Pattern changed over time with very little cholera notification after 2012 – only sporadic cases reported until a resurgence in 2018 • High AR and CFR registered in rural areas 11
Cholera Seasonality Median outbreak start week Week W45 – W51 (November – mid December) week� onset� [min-max] STATE� /� COUNTY Median� MASHONALAND� WEST 47� [37-11] HARARE 48� [33-13] MANICALAND 50� [28-27] MASHONALAND� CENTRAL 51� [43-20] MASVINGO � 51� [32-23] MASHONALAND� EAST � 51� [40-20] MIDLANDS � 48� [40-05] MATABELELAND� SOUTH 47� [44-05] MATABELELAND� NORTH 47� [41-01] BULAWAYO 45� [45-45] 12
Risk factors Lack of adequate access to safe water & sanitation and access to healthcare Unreliable water services (quantity; service interruptions, quality) Contaminated environment (open defecation; Sewer bursts & blockages in urban/periurban areas) Rainy season High population density / population density per borehole Low elevation in high-density neighborhoods Presence / number of markets / bus stations in the neighborhood Individual risk factors: low cholera immunity, weakened immune systems due to HIV and AIDS, and poor nutritional status
High-risk population Children under five and women of childbearing age Rural populations (AR in rural areas > in urban areas in 2008) Mobile working population (age 15-44) in urban areas Refugees / displaced people in camps High-risk practices & aggravating factors Open defecation (44% in rural areas – MICS 2014) Use of unprotected water sources Body transportation & preparation during burials, consumption of food at funeral feasts Belonging to a religious sect that discourages seeking medical attention Low cholera awareness Limited access to oral rehydration solutions at community level increase the severity of dehydration – and risk of mortality Inadequate surveillance / access to healthcare (61.4% of all reported deaths took place in the community in 2008-2009)
Hotspot classification Cholera hotspot Definition A geographically limited area (e.g. city, administrative level 2 or health district catchment area) where environmental, cultural and/or socioeconomic conditions facilitate the transmission of the disease and where cholera persists or re-appears regularly. Hotspots play a central role in the spread of the disease to other areas. Source: Interim Guidance Document on Cholera Surveillance Global Task Force on Cholera Control (GTFCC) Surveillance Working Group June 2017 http://www.who.int/cholera/task_force/GTFCC-Guidance-cholera-surveillance.pdf
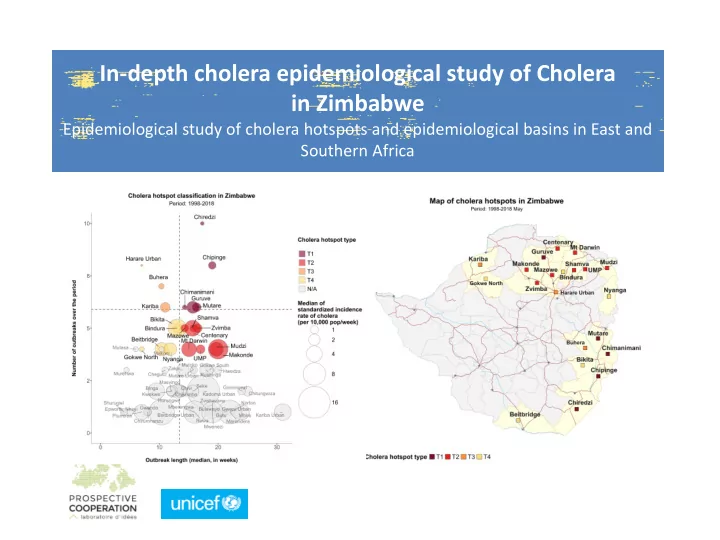
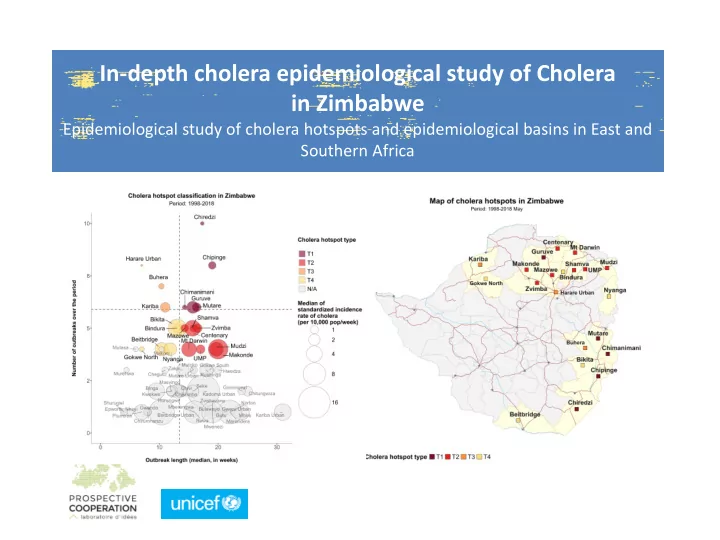
Hotspot classification Type� Interpretatio Frequency� Frequency� Duration� Duration� Intensity� Intensity� n� (Percentile� of� outbreaks� (Percentile� (number� (Percentile� Median� distribution)� of� of� weeks)� of� Indicende� distribution distribution over� time� )� )� T1� Highest� >90� >6� � ≥ 40� ≥ 13.5� � � � Priority� � T2� High� >70� and� >4� and<6� � ≥ 40� ≥ 13.5� � � � Priority� � <90� T3� Med.� >90� >6� � <40� <13,5� � ≥ 40� >0,9� Priority� � T4� Low� >70� and� >4� and� <6� � <40� <13,5� � ≥ 40� >0,9� Priority� � <90� Table� 1:� Frequency� and� duration� of� cholera� outbreak� thresholds� per� hotspot� type� �
Hotspot classification To be classified as Hotspot, a district must have Frequency of outbreaks > 4 To be classified as Hotspot T1, Frequency > 6 & Duration > 13.5 weeks To be classified as Hotspot T3, Frequency > 6 & Duration < 13.5 weeks but Intensity >0.9 To be classified as Hotspot T2, Frequency > 4 & Duration > 13.5 weeks To be classified as Hotspot T4, Frequency > 4 & Duration < 13.5 weeks but Intensity >0.9 NB: Other Potential Areas of Interest: Buhera – Harare Urban – Makoni, Gwokwe North, Mutasa
Recommend
More recommend