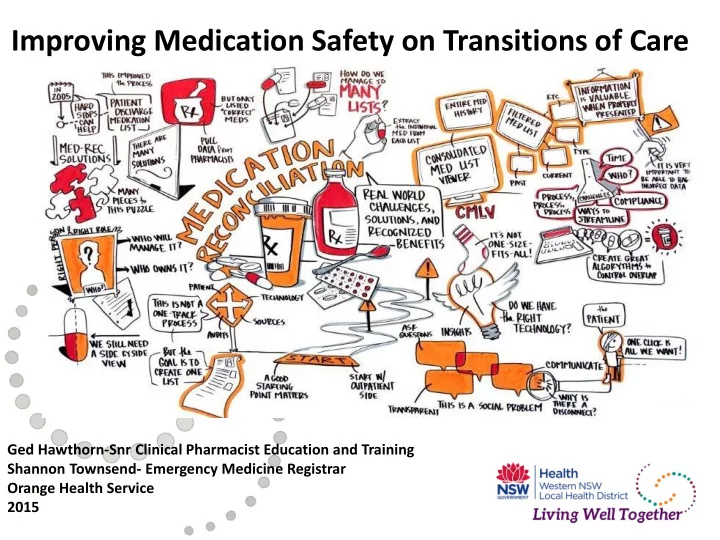
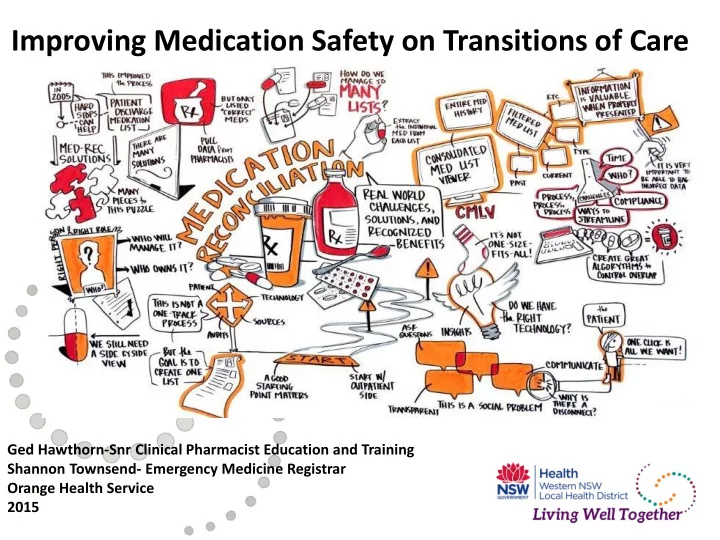
Improving Medication Safety on Transitions of Care Ged Hawthorn-Snr Clinical Pharmacist Education and Training Shannon Townsend- Emergency Medicine Registrar Orange Health Service 2015
Orange Health Service
Med Rec- How do we compare? • Using adapted QLD health MAP since 2008 • Adopted NSW Health MMP 2011 • 2012- Project Med Rec on admission • Since then around 75% pts have MMP • Discharge process
CEC Continuity of Medication Management Audit Percentage of patients with at least one medication omission or discrepancy at discharge – OBH 2013 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% Omission Discrepancy Either Omission or Discrepancy
A Series of Audits 96% Patients taking medications with a discharge summary 88% 100% 58% Patients with more than 5 mediciens on discharge 69% 72% 46% Patients on medicines, that had one or more medications omitted 48% 50% 1/01/2013 OHS 13% Patients with a discharge summary that had additional 13% unexplained medicines 20.00% 1/06/2013 OHS 61% Patients with at least one omission or discrepancy on their 67% discharge summary 73% 1/06/2014 CCU 79% Patients on medicnes which were ceased, new or changed during 82% admission 85% 0% Patients with discharge summary that had a rationale for all 13% changes to medicines 18% Patients who received a patient friendly medication list 22% percentage of identical med lists and discharge summaries 0%
Time for Action • Engaging Staff: Feedback, Highlighting risk, engaging, empowering, pts story, solution focused • The Team: Pharmacists, JMOs, Regs, NUM, CNC, CNE, IT, Pt Safety • Combined Aim: Improve the accuracy of medication documentation and increase patient education by 20% within 6 months
Planning & implementing solutions Communication No clear plan from team re meds IT D/C summary written in Latin No template for Pt verbally counselled but not meds in EMR documented No eMMP and discharge checklist Need pharmacist on round for direct and effective communication Transcription errors No Multi-d communication tool Incorrect Systems don’t documentation and integrate lack of patient JMO writing d/c Bed pressure, high turnover, not education regarding unfamiliar with pt enough time to prepare d/c. medicines on discharge JMO hands documents to ward clerk Underfunded pharmacist FTE/ no redundancy rather than to engage in conversation with pt. Pt not seen by Weekend Discharges no pharmacist on d/c reconciliation process Pharmacist not available on ward at time of Busy staff conflicting tasks to discharge do No formal multi-d discharge process. Nursing not taking Staffing ownership of medication counselling. Processes
Possible solutions High Impact Low Effort Increase communication Remove latin abbreviations Develop medicine list template Nursing flagging high risk patients Create a Multi-D eMMP Medication safety discharge checklist Rostering pharmacist time Discharge flow sheet for staff to follow
Possible solutions High Impact High Effort • Customise eMR for useful discharge templates Costs $ • Education for nurses to do medication reconciliation Time • Employ more pharmacists Attempting to • Having one integrated eHealth system I’ll keep dreaming! • Pharmacist increase med rec on discharge • Streamline medical rounding • Clinical streams for pharmacists to provide redundancy
Enablers | Barriers Pharmacy not built into discharge process Smaller Hospital Staffing Motivated staff Multi-D engagement Med Rec Consultant buy in Union’s and position descriptions SIBR Model Med Rec not seen as everyone’s business Pharmacist med rec on ward Individuals Patient Focus Research demonstrating importance CEC toolkit MMP
SIBR In Action
Outcomes and evaluation 2015 Western NSW LHD Living Well Together Health Awards
Outcomes and evaluation
Sustaining change • Policies on medication reconciliation developed • MMP, BPMH and HETI med rec training during orientation • Cardiologists briefed to educate JMOs on discharge expectations • eMMP is now in use in ICU and is available for ICIP across district • Medication reconciliation is a large focus of all pharmacists work • Engagement and results shown to new team on ward 2015 Western NSW LHD Living Well Together Health Awards
How to gain support from the Exec • Financial Savings Number of discrepancies per patient (1.55- from baseline audit data) x Number of patients per year through cardiovascular ward (1654- from health round table report) x Percent of patients with discrepancies that would result in an adverse drug event (9.4% of errors on a cardiology ward that could result in harm [1] ) x Percent effectiveness of process (85% of discrepancies avoided through med rec process, global and local result) x Cost of an average adverse drug event ($2500 conservative) = Annual gross cost savings ($512 100) • Accreditation - helps to meet 15 standard 4 requirements. • Strategic Fit Financial model developed by Steven B. Meisel, Pharm D Minneapolis. [1] Magalha ˜es GF, Santos GBNdC, Rosa MB, Noblat LdACB (2014) Medication Reconciliation in Patients Hospitalized in aCardiology Unit. PLoS ONE 9(12): e11549doi:10.1371/journal.pone.0115491
Questions
Recommend
More recommend