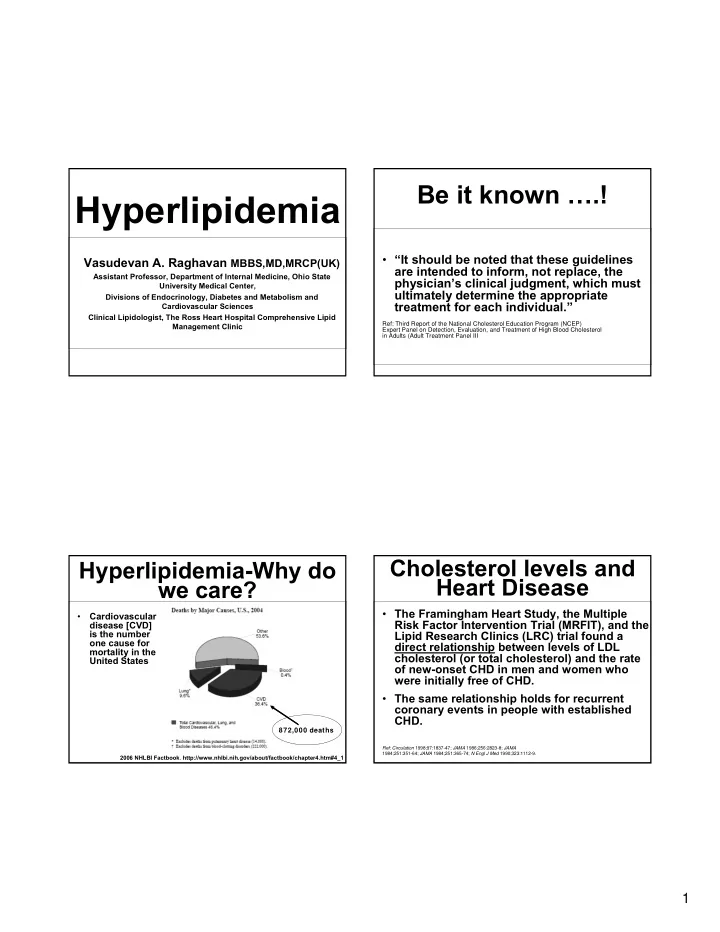
Be it known ….! Hyperlipidemia • “It should be noted that these guidelines Vasudevan A. Raghavan MBBS,MD,MRCP(UK) are intended to inform, not replace, the Assistant Professor, Department of Internal Medicine, Ohio State physician’s clinical judgment, which must University Medical Center, ultimately determine the appropriate Divisions of Endocrinology, Diabetes and Metabolism and treatment for each individual.” Cardiovascular Sciences Clinical Lipidologist, The Ross Heart Hospital Comprehensive Lipid Management Clinic Ref: Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III Cholesterol levels and Hyperlipidemia-Why do Heart Disease we care? • The Framingham Heart Study, the Multiple Cardiovascular • Risk Factor Intervention Trial (MRFIT), and the disease [CVD] is the number Lipid Research Clinics (LRC) trial found a one cause for direct relationship between levels of LDL mortality in the cholesterol (or total cholesterol) and the rate United States of new-onset CHD in men and women who were initially free of CHD. • The same relationship holds for recurrent coronary events in people with established CHD. 872,000 deaths Ref: Circulation 1998;97:1837-47; JAMA 1986;256:2823-8; JAMA 1984;251:351-64; JAMA 1984;251:365-74; N Engl J Med 1990;323:1112-9. 2006 NHLBI Factbook . http://www.nhlbi.nih.gov/about/factbook/chapter4.htm#4_1 1
Atherogenic Particles – Lipoprotein Subclasses What are They? 2
Frederickson Classification P C of Hyperlipoproteinemias 100% P P 80% C P Composition 60% T C 40% T C 20% T T 0% Chylo- VLDL LDL HDL microns Lipoprotein Type The major classes of lipoproteins and their relative content of triacylglycerol ( T ), cholesterol ( C ) and protein (P) LDL-C Lowering With Statins: LDL Cholesterol Reduced CHD Events • Typically makes up 60–70 % of the total serum cholesterol Secondary Prevention 4 S-PL Primary Prevention 2 5 • It has a single apo-B molecule in its structure. LI PI D-PL 2 0 4 S-Rx Events ( % ) • It is the major atherogenic lipoprotein 1 5 CARE-PL CARE-Rx • It is the primary target for therapy in most W OSCOPS-PL 1 0 LI PI D-Rx W OSCOPS-Rx individuals, with few exceptions. [This 5 focus on LDL has been strongly validated AFCAPS- Rx by recent clinical trials, which show the AFCAPS- PL 0 efficacy of LDL-lowering therapy for 5 0 7 0 9 0 1 1 0 1 3 0 1 5 0 1 7 0 1 9 0 2 1 0 reducing risk for CHD.] LDL Cholesterol ( m g/ dL) Adapted from Illingworth DR. Med Clin North Am . 2000;84:23-42. 3
Hypercholesterolemia- HDL Cholesterol Manifestations: Corneal Arcus and Tendon Xanthomata • Normally makes up 20–30 % of the total serum cholesterol • The major apolipoproteins of HDL are apo A-I and apo A-II. • HDL-c levels are inversely correlated with risk for CHD. • Some evidence indicates that HDL is anti- atherogenic, although a low HDL-c often reflects the presence of other atherogenic factors. Palmar Crease Xanthoma- VLDL Pathognomonic of Dysbetalipo- [ not part of a lipid panel ] Proteinemia or Type III Hyperlipidemia • Are triglyceride-rich lipoproteins, but contain 10–15 percent of the total serum cholesterol. • The major apolipoproteins of VLDL are apo B- 100, apo Cs (C-I, C-II, and C-III), and apo E. • VLDL are produced by the liver and are precursors of LDL • VLDL remnants consist of partially degraded VLDL and are relatively enriched in cholesterol ester. • VLDL remnants appear to promote athero- sclerosis, similar to LDL 4
Lipemia-Excess Eruptive Xanthoma-Seen in Patients with Very High Triglycerides Triglycerides [VLDL / Chylomicrons] Creamy supernatent=high chylomicron Lipemic fasting serum usually means the excess presence of either VLDL or chylomicron [types I, V and rarely IV] Uniformly lipemic serum= high VLDL Evanescent pin-head or larger yellow papules with an erythematous base occurring most commonly on the buttocks, shoulders and extensor surfaces of the extremities . Lipid Profile Lipid Profile The The Basic Test Basic Test The first step is to obtain a fasting lipid • • Calculated serum triglycerides are not profile usual components are reliable when tg levels are elevated 1. Triglycerides [ measured ] above 350-400 mg/dl 2. HDL cholesterol [ measured ] = [HDL-c] • ‘Direct ldl-c’ measurement is possible 3. Total Cholesterol [ measured ] = [T.Chol] and can be requested in those with hypertriglyceridemia [icd-9 code for 4. LDL cholesterol [ calculated ] = [LDL-c] pure hypertriglyceridemia 272.1 ] calculation usually based on the Friedewald’s formula (T. Chol ― HDL-c ― TG/5) 5
Lipid Profile The Basic Test • Serum triglycerides are affected by Who Should Get a food intake. Hence the need for a fasting blood sample. Lipid Panel? • Non-HDL-c [ T.Chol ― HDL-c] is a measure of all apolipoprotein-B [apo- B] containing particles [LDL-c, IDL-c and VLDL-c] and does not need a patient to fast. Screening Guidelines Lipid Screening Physician Initiated Patient Request Screening group Begin screening Frequency Test • “ I want you to check my blood cholesterol levels” CHD, CHD risk Age 20 years or at 1-2 years Fasting lipid equivalent, or > 2 onset panel • Pre-test counseling risk factors • Icd-9 codes and billing Familial Age 20 years 2 years Fasting lipid issues:reimbursement issues must be dyslipidemia or panel discussed beforehand family history of premature CHD • Relevant in those with a family h/o None of the above Age 20 years 5 years Fasting lipid panel or non- premature chd, hyper-lipidemia, sudden fasting total cardiac death etc. cholesterol and HDL-C 6
National Cholesterol ATP III Classification Education Program [NCEP] of T. Chol Adult treatment Panel [ATP] • < 200 desirable • ATP I: published 1988 • ATP II: published 1993 • 200-239 borderline high • ATP III: published 2002 • ATP III Update: 2004 • > 240 high ATP III Classificaton ATP III Classification of LDL-c [mg/dl] of HDL-c • < 100 optimal • < 40 Low • 100-129 near optimal / above optimal • > 60 High • 130-159 borderline high • 160-189 high • > 190 very high 7
Treatment Principles in Treatment Principles in Dyslipidemia Patients Dyslipidemia Patients • CV risk stratification • CV risk stratification • Define targets for therapy • Define targets for therapy • Determine intensity of treatment needed • Determine intensity of treatment needed • Lifestyle measures • Lifestyle measures • Pharmacotherapy • Pharmacotherapy • Screening for complications of disease and • Screening for complications of disease and therapy therapy • Comprehensive cardiometabolic approach • Comprehensive cardiometabolic approach Risk Factors that Modify Non-Lipid Risk Factors LDL- c Goals for CHD Positive risk factors: MODIFIABLE RISK NON-MODIFIABLE FACTORS RISK FACTORS 1. Age Hypertension* Age* 2. Male >45;Female >55 Cigarette smoking* Male sex* 3. Family h/o premature CHD [MI/SCD < 55 in father/male 1 st degree relatives; < 65 in mother/other 1 st degree Prothrombotic states† Family history of relatives] premature CHD Diabetes mellitus* 4. Current smoker Obesity 5. Hypertension [> 140/90 or on medications] Physical inactivity 6. Low HDL-c [ < 40 mg/dl both genders] Atherogenic diet Negative risk factor: *included in ATP III risk assessment † inferential [anti-platelet drugs / 1. HDL-c > 60 mg/dl in both genders anticoagulants seem to reduce CHD events 8
NCEP ATP 3 Risk Very High Risk Patients Categories 1. Recent acute coronary syndromes • Very-high risk 2. Established cardiovascular disease and • High risk � Multiple major risk factors (especially Type 2 DM) • Moderately-high risk � Severe and poorly controlled risk factors (especially cigarette smoking) • Moderate risk � Multiple risk factors of the metabolic • Low risk syndrome (abdominal obesity, increased Tg, decreased HDL, blood pressure ≥ 130/85, glucose > 100 Coronary Risk Categorization in High Risk Patients Patients without Established CHD • High risk 1. History of CHD � >20% 10 year CHD risk 2. Type 2 diabetes • Moderately-high risk 3. Symptomatic carotid disease � 2 or more risk factors and 10-20% 10 year risk 4. Peripheral vascular occlusive disease • Moderate risk � 2 or more risk factors and < 10% 10 year risk 5. Abdominal aortic aneurysm • Lower risk � 0-1 risk factors and < 10% 10 year risk 9
CHD/CHD Risk Equivalents For Those without CHD 10-year CAD risk exceeds 20% • Determine presence of major risk factors aside from LDL-C • Established cad � Current cigarette smoking • Stroke and stroke variants � BP ≥ 140/90 or on anti-hypertensive medication • Peripheral arterial disease � HDL-C < 40 mg/dl (if ≥ 60 count as negative RF) • Atherosclerotic aortic aneurysms � CHD in ♂ 1st degree relatives < 55, or ♀ first • Post-op cabg / carotid endarterectomy / degree relatives < 65 peripheral arterial revascularization � Age ♂ ≥ 45 or ♀ ≥ 55 • Diabetes mellitus • Calculate Framingham Risk Score in those with 2 or more risk factors NCEP/Framingham risk scores: Estimate of 10-yr Hard CHD risk in men without CHD Available online at: http://hp2010.nhlbihin.net/atpiii/calculator.asp?usertype=prof 10
Recommend
More recommend