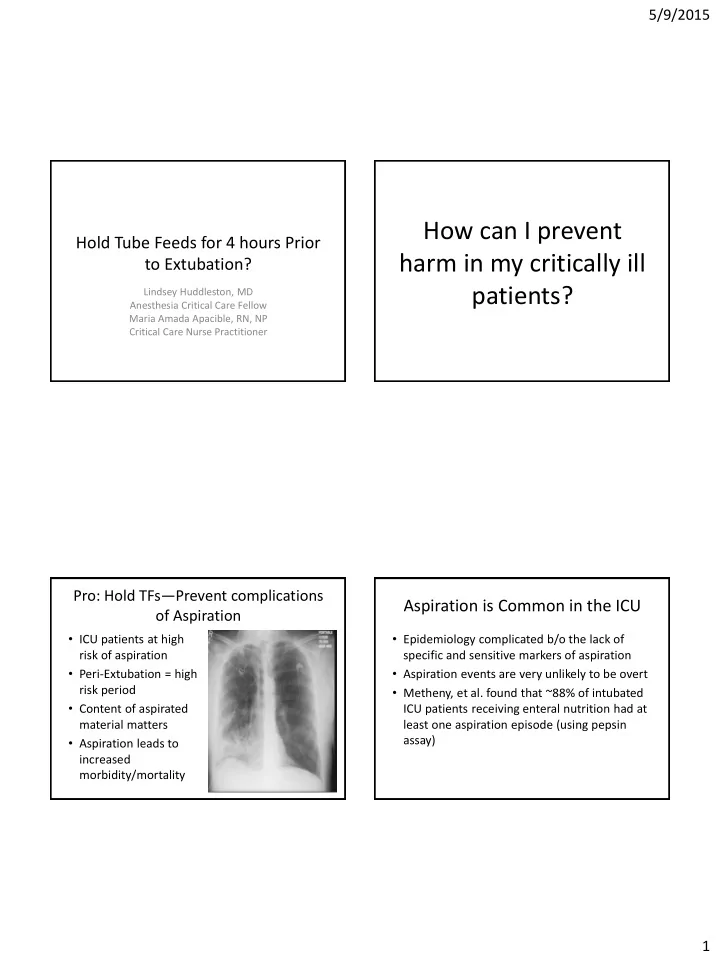
5/9/2015 How can I prevent Hold Tube Feeds for 4 hours Prior harm in my critically ill to Extubation? patients? Lindsey Huddleston, MD Anesthesia Critical Care Fellow Maria Amada Apacible, RN, NP Critical Care Nurse Practitioner Pro: Hold TFs — Prevent complications Aspiration is Common in the ICU of Aspiration • ICU patients at high • Epidemiology complicated b/o the lack of risk of aspiration specific and sensitive markers of aspiration • Peri-Extubation = high • Aspiration events are very unlikely to be overt risk period • Metheny, et al. found that ~88% of intubated • Content of aspirated ICU patients receiving enteral nutrition had at material matters least one aspiration episode (using pepsin assay) • Aspiration leads to increased morbidity/mortality 1
5/9/2015 Impaired Swallowing After Mechanical ICU Patients = High Aspiration Risk Ventilation • Altered Level of Consciousness • Swallowing dysfunction has been demonstrated in – Medications (sedatives, narcotics) patients who have been intubated for as short as 48h – Encephalopathy • Possible etiologies for swallowing dysfunction: – Primary CNS problem (eg., stroke, TBI) – Residual sedation – Delirium – Decreased Cough reflex • Impaired gastric emptying – Decreased airway reflexes and upper airway sensitivity – Ileus – Mechanical problems (Laryngeal muscular dysfunction, – Recent surgery glottic injury) – SBO • Post-extubation dysphagia is common in ICU (up to – narcotics 60% of pts w/o and 90% of patients with neurologic • GERD disorders) • Impaired swallowing – Especially within first 24h of extubation Decreased Cough Reflex High risk of Aspiration Peri-Extubation Postextubation • Leder, et al. Fiberoptic endoscopic documentation of • 86 pts undergoing CABG the high incidence of aspiration following extubation in • Baseline cough reflex critically ill trauma patients. – Trauma patients intubated > 48h measured, then within – Identified aspiration in 45% of pts w/in first 24h of 2hrs post-extubation and extubation mult. subsequent time • Barquist, et al. Postextubation fiberoptic endoscopic points until reflex evaluation of swallowing after prolonged endotracheal returned intubation: a randomized, prospective trial. – Trauma patients intubated for > 48h • 60% of pts with NO reflex – ~15% rate of aspiration in first 24h post-extubation at first measurement – All patients who developed PNA had aspiration event 2
5/9/2015 Aspiration Increase Risk of PNA and What/How much is Aspirated Matters ALI/ARDS • Aspiration is recognized • Lower pH = higher risk of as a major cause of chemical pneumonitis ALI/ARDS • Higher – Studies show volume/particulate approximately 1/3 of matter = higher risk of patients with aspiration pneumonitis go on to PNA develop ALI/ARDS • Metheny, et al.-- • Possible need for re- Recurrent aspiration of intubation (mortality acidic material increases increase demonstrated in r/o PNA numerous studies) Risk of Aspiration Too High, Hold TFs! • Aspiration is common in the ICU • How can I prevent harm • Peri-extubation, ICU patients carry numerous in my critically ill risk factors for aspiration • Aspirated material content matters: oral patients? secretions ≠ gastric contents or particulate matter • Aspiration increased r/o ALI/ARDS, re- intubation increased health care costs, morbidity and mortality 3
5/9/2015 Con: Continue tube feedings prevent Importance of enteral tube feeding in Malnutrition/Underfeeding critically ill patients • Emerging data that nutritional support is • Malnutrition from underfeeding is common in essential for recovery of critically ill patients. the ICU and increases morbidity and mortality. • Optimal provision of calories and protein is • No data that continuing TF increases risk for demonstrated to aspiration. – Reduce Morbidity and Mortality • There are preliminary data that continuing TF – Reduce Length of hospital and ICU stay – Improve function of the immune system in the peri-extubation period is safe and – Mitigate weakness and deconditioning improves nutrition. – Improve wound healing – Reduce Health care costs A typical timeline for holding tube Data supporting continuation of TFs feedings for extubation • While data is limited, there are some clinical trials in • NPO and hold TF at midnight (possibly 4 am) for morning extubation. pediatric population that continuing TFs peri-extubation is • safe and results in more optimal nutrition Patient placed on SBT & sedation weaned at 6 am. ABG sent. • • Lyons et, al: RCT comparing continuous TFs to interrupted ICU team rounds start at 9 am. • ICU team sees patient on rounds, but needs to confer with the feeds at time of extubation in pediatric patients primary team prior to extubation. – No increase in adverse events in continuous TF group • ICU finished rounds between 11 am and 12 pm. – Significant increase in calorie percentage in continuous TF group • Patient may be extubated following ICU rounds provided the team (55% greater) is not distracted by admissions, a procedure, a code blue, etc. • Multiple studies have shown that it is safe to continue TFs • Tube feeds are held for 2 to 4 hours following extubation to ensure in the perioperative period that the patient will not need reintubation. – Patients with continuous TFs have fewer wound infections • Result: Tube feedings are held for 8 to 16 hours which is too much – Patients require less albumin supplementation time to be made up with increased tube feeding rates and patient is – Overall better outcomes malnourished that day. 4
5/9/2015 Continuing TF not necessarily Incidence of Aspiration for Planned increasing risk verses Unplanned Extubation • Unplanned extubations may result in aspiration • While the concern for aspiration exists, there and possible reintubation, leading to increased are no data that continuing TFs increases risk. morbidity and mortality. – The factors contributing to the higher reintubation risk in unplanned extubation are continuing sedation, decreased GCS, increased secretions, impaired ability to protect airway, severity of illness – not ready. • However, patients who undergo planned extubation do not carry the same risk, thus risk of aspiration and reintubation is likely small. Continuing TF is right for most ICU Continuing TF is right for most ICU patients patients • The reintubation rate for planned extubations is • Patients who receive continuous TF meet 90% ~17% while the reintubation rate for unplanned of nutritional requirements while those with extubation is ~50%. interrupted TF only meet 50%. • The risks for aspiration and reintubation simply are not present for most ICU patients who have planned extubations. – Sedation has been weaned. – Awake and demonstrate neurological readiness for extubation. – Minimal secretions. – Able to protect airway – strong cough and gag. 5
Recommend
More recommend