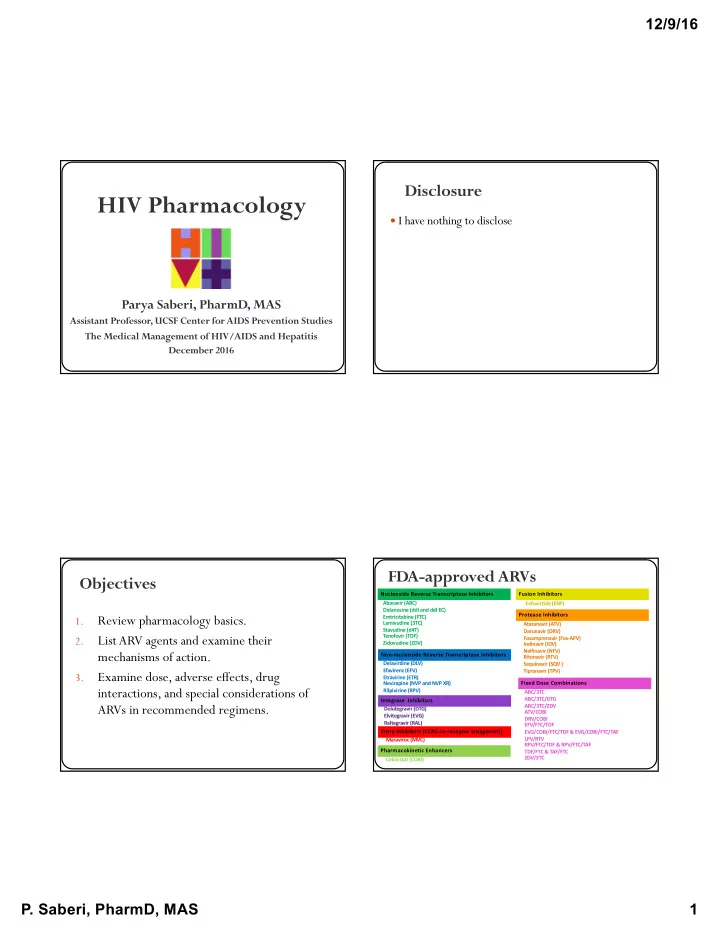
12/9/16 Disclosure HIV Pharmacology I have nothing to disclose Parya Saberi, PharmD, MAS Assistant Professor, UCSF Center for AIDS Prevention Studies The Medical Management of HIV/AIDS and Hepatitis December 2016 FDA-approved ARVs Objectives Nucleoside Reverse Transcriptase Inhibitors Fusion Inhibitors Abacavir (ABC) Enfuvirtide (ENF) Didanosine (ddI and ddI EC) Protease Inhibitors Review pharmacology basics. Emtricitabine (FTC) 1. Lamivudine (3TC) Atazanavir (ATV) Stavudine (d4T) Darunavir (DRV) List ARV agents and examine their Tenofovir (TDF) 2. Fosamprenavir (Fos-APV) Zidovudine (ZDV) Indinavir (IDV) Nelfinavir (NFV) mechanisms of action. Non-nucleoside Reverse Transcriptase Inhibitors Ritonavir (RTV) Delavirdine (DLV) Saquinavir (SQV ) Efavirenz (EFV) Tipranavir (TPV) Examine dose, adverse effects, drug 3. Etravirine (ETR) Nevirapine (NVP and NVP XR) Fixed Dose Combinations interactions, and special considerations of Rilpivirine (RPV) ABC/3TC ABC/3TC/DTG Integrase Inhibitors ARVs in recommended regimens. ABC/3TC/ZDV Dolutegravir (DTG) ATV/COBI Elvitegravir (EVG) DRV/COBI Raltegravir (RAL) EFV/FTC/TDF Entry Inhibitors (CCR5 co-receptor antagonists) EVG/COBI/FTC/TDF & EVG/COBI/FTC/TAF LPV/RTV Maraviroc (MVC) RPV/FTC/TDF & RPV/FTC/TAF Pharmacokinetic Enhancers TDF/FTC & TAF/FTC ZDV/3TC Cobicistat (COBI) P. Saberi, PharmD, MAS 1
12/9/16 HIV Life-cycle Recommended Regimens Fusion inhibitors RPV *** DRV/r DRV/c DRV/c EVG/c ATV/c ATV/r DRV/r DTG DTG RAL EFV CCR5 co- receptor Protease inhibitors inhibitors ABC/3TC ** TDF/FTC or TAF/FTC* Reverse transcriptase inhibitors Integrase inhibitors * TDF/FTC not recommended if CrCl <70 & TAF/FTC not recommended if CrCl <30 ** If HLA-B*5701 is negative *** If pre-treatment HIV RNA <100,000 copies/mL & CD4 >200 cells/mm3 http://aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf Alternative Regimens Lightening Fast RPV *** DRV/r DRV/c DRV/c EVG/c ATV/c ATV/r DRV/r DTG DTG RAL EFV Pharmacology Review ABC/3TC ** TDF/FTC or TAF/FTC* * TDF/FTC not recommended if CrCl <70 & TAF/FTC not recommended if CrCl <30 ** If HLA-B*5701 is negative *** If pre-treatment HIV RNA <100,000 copies/mL & CD4 >200 cells/mm3 http://aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf P. Saberi, PharmD, MAS 2
12/9/16 PK Parameters Pharmacology Review AUC (area under the curve): average drug concentration over a time period (e.g.,1 dosing interval or 1 day). Represents drug exposure. PK : What your body does to the drug. T ½ (half-life): time taken to reduce the concentration by 50% Study & characterization of time course of drug C max : Peak plasma concentrations; can be associated with a PD response Absorption, Distribution, Metabolism, & C min : Plasma concentrations at the end of the dosing interval (just before Excretion . next dose); lowest concentration within a dosing interval C 0h , C trough , C τ ( tau: the length of the dosing interval) PD : What the drug does to your body. Subjective (anxiety level) or objective (BP , pupil size) http://i-base.info/ttfa/learning-resources/what-happens-when-you-take-a-drug/ Transporters Excretion P-glycoprotein (P-gp): efflux enzyme that “pushes” drugs out of GI blood stream back into GI lumen P-gp inhibitor: RTV , COBI P-gp inducer: SJW , GFJ, rifampin Organic anion transporters (OAT): involved in secretion or reabsorption of drugs; in kidney, brain, & liver OAT inhibitor: COBI Organic cation transporters (OCT): involved in secretion or reabsorption of drugs; in liver, skeletal muscle, kidney, heart, small intestine, prostate OCT inhibitor: RTV , DTG P. Saberi, PharmD, MAS 3
12/9/16 Uridine Diphospho- Metabolism Glucuronosyltransferase (UGT) Responsible for glucuronidation, a major part of phase II metabolism (conjugation) UGT 1A1 Substrate: RAL, DTG UGT 1A1 Inhibitor: ATV UGT 1A1 Inducer: TPV , RTV , rifampin Cytochrome P450 Enzymes Question #1: How quickly does CYP450 induction occur? Essential for metabolism of two-thirds of meds cleared by metabolism >50 enzymes; however, 6 metabolize 90% of drugs: CYP1A2, 1. 1-2 hours CYP2C9, CYP2C19, CYP2D6, CYP3A4 , & CYP3A5 Primary cause of the majority of drug-drug & drug-food interactions 2. 1-2 days CYP450 Inducers : ↑ CYP450 enzyme activity by ↑ enzyme synthesis (e.g., efavirenz, rifampin) 3. 1-2 weeks CYP450 Inhibitors : Block metabolic 4. 1-2 months activity of CYP450 enzymes (e.g., protease inhibitors) P. Saberi, PharmD, MAS 4
12/9/16 Question #2: How quickly does CYP450 Inducers CYP450 inhibition occur? Onset gradual ( 1-2 weeks ) 1. 1-2 hours Onset depends on half-life (t 1/2 ) of the 2. 1-2 days inducer & synthesis of new enzymes 3. 1-2 weeks Offset depends on inducer elimination & decay of enzyme stores 4. 1-2 months Boosting CYP450 Inhibitors Onset is rapid (after 1-2 doses) Taking advantage of a drug-drug interaction Low-dose CYP450 inhibitors (e.g., RTV or COBI) lead to: Extent of inhibition depends on dose & binding ↑ AUC, ↑ Cmin & ↑ Cmax ability of inhibitor ↓ risk of drug resistance Offset depends on elimination of the inhibitor & Can use lower doses of PI half-life of the inhibitor at enzyme site May eliminate food restriction ↑ plasma half-life ( t 1/2 ) All PIs are net inhibitors of CYP3A4 ↓ dosing frequency Boosting: use of low-dose CYP450 inhibitor to ↑ ARV exposure Zeldin RK, et al. Journal of Antimicrobial Chemotherapy.53.2004. P. Saberi, PharmD, MAS 5
12/9/16 Question #3: Which of the following Drawbacks of Boosting is (are) true re: RTV & COBI ↑ potential of drug-drug interactions 1. Both inhibit P-gp & BCRP transporters ↑ pill-burden 2. Both inhibit MATE1 & OATP except fixed-dose combos LPV/r, EVG/c, DRV/c, ATV/c transporters ↑ risk of metabolic AEs 3. Both result in increased Scr & TG However, 4. Both inhibit or induce CYP450 enzymes Boosting with RTV or COBI is recommended for PI- & 5. Options 1, 2, & 3 EVG-based regimens 6. All of the above RTV vs COBI RTV vs COBI: PK RTV COBI RTV COBI Absorption Both inhibit intestinal transporters P-gp & BCRP: (Structural analogue of RTV) ↑ absorption of ATV , DRV , TAF Boosting w/ 100mg QD-BID Boosting w/ 150mg QD Excretion Both inhibit OATP & MATE1 (transporter involved in tubular Antiviral activity at higher doses Without antiviral activity secretion of Cr) Inhibits or induces drug-metabolizing Inhibits drug-metabolizing enzymes • ↑ Scr due to inhibition of Cr secretion vs. impairment of enzymes → DDIs → DDIs renal function • COBI results in higher Scr vs. RTV; may be due to COBI accumulating in tubular cells & having higher concentrations to inhibit MATE1 Marzolini C, et al. J Antimicrob Chemother. 2016 Marzolini C, et al. J Antimicrob Chemother. 2016 Sherman E, et al. Clinical Therapeutics. 2015;37,9. P. Saberi, PharmD, MAS 6
12/9/16 RTV vs COBI: PK RTV vs COBI: DDIs interchangeable as CYP3A inhibitors Summary of differences in predicted interaction profiles: Meds that are… RTV COBI Examples Metabolism RTV COBI ↓ Glucuronidated &/or metabolized by not affected bupropion or inducible CYPs & w/o CYP3A methadone Inhibition • CYP3A inhibitor • More specific CYP3A inhibitor involvement (CYP2B6) • CYP2D6 inhibitor • Weaker CYP2D6 inhibitor ↓ Glucuronidated &/or metabolized by moderately Sertraline Induction • CYP1A2, CYP2B6, • Unlikely to induce drug ↑ inducible CYPs to a larger extent than (2B6>2C9, 2C19, CYP2C9, & CYP2C19 & metabolism CYP3A 2D6, 3A4) glucuronidation inducer ↓ or only ↑ Subject to CYP induction or inhibition Duloxetine ↑ (2D6, 1A2) Inducible CYPs: CYP1A2, CYP2B6, CYP2C9, & CYP2C19 ELV: inducer of CYP2C9 (ELV/c overall effect: ↓ warfarin) Marzolini C, et al. J Antimicrob Chemother. 2016 Marzolini C, et al. J Antimicrob Chemother. 2016 RTV vs COBI: AEs RTV COBI Case #1 D, HA, N, nasopharyngitis N, D, HA, nasopharyngitis Median ↑ TG: 32, TC: 9 mg/dL Median ↑ TG: 19, TC: 5 mg/dL Median ↑ SCr: 0.09 mg/dL; Median ↑ SCr: 0.13 mg/dL; ↓ CrCl: 9 mL/min ↓ CrCl: 13 mL/min D/C due to renal AEs: 1.4% D/C due to renal AEs: 1.7% Sherman E, et al. Clinical Therapeutics. 2015;37,9. P. Saberi, PharmD, MAS 7
Recommend
More recommend