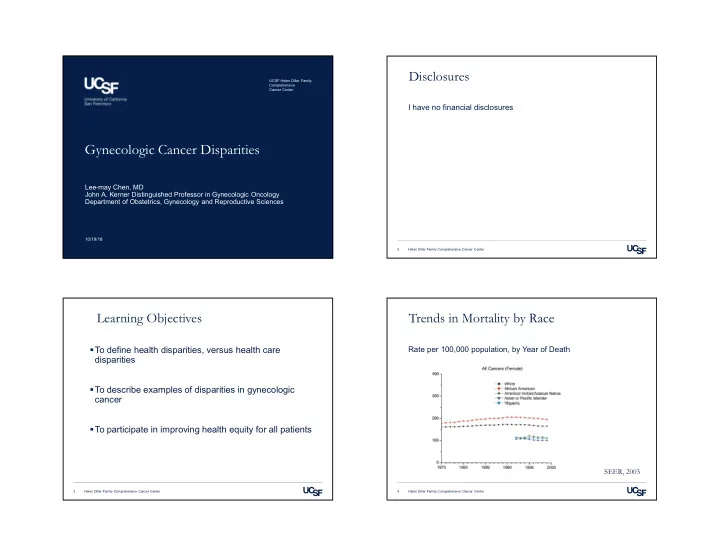
Disclosures UCSF Helen Diller Family Comprehensive Cancer Center I have no financial disclosures Gynecologic Cancer Disparities Lee-may Chen, MD John A. Kerner Distinguished Professor in Gynecologic Oncology Department of Obstetrics, Gynecology and Reproductive Sciences 10/19/18 2 Helen Diller Family Comprehensive Cancer Center Learning Objectives Trends in Mortality by Race To define health disparities, versus health care Rate per 100,000 population, by Year of Death disparities To describe examples of disparities in gynecologic cancer To participate in improving health equity for all patients SEER, 2003 3 Helen Diller Family Comprehensive Cancer Center 4 Helen Diller Family Comprehensive Cancer Center
Examples of Cancer Health Disparities Cancer Health Disparities Incidence (new cases) Prevalence (all existing cases) Mortality Morbidity Survivorship , QOL after Cancer Treatment Burden of cancer, related health conditions Screening rates Stage at diagnosis 5 Helen Diller Family Comprehensive Cancer Center 6 Helen Diller Family Comprehensive Cancer Center Disparities of Referrals Definitions Health Disparities: difference in health that is closely linked with social or economic, and/or environmental disadvantage Equal health may require different levels of resources. Source: UCSF Cancer Registry 7 Helen Diller Family Comprehensive Cancer Center 8 Helen Diller Family Comprehensive Cancer Center
Age-standardized Incidence and Death Rates Cervical Cancer Stage Rates per 100,000, 1996-2000 By Race and Ethnicity, SEER 1996-2000 By Poverty Rate, SEER 1995-1999 9 Helen Diller Family Comprehensive Cancer Center 10 Helen Diller Family Comprehensive Cancer Center Factors that Influence Social Disparities Cervical Cancer Difficulty in access • Poor follow-up of abnormal screenings • Lower literacy rates • Medical comorbidities • Public insurance • Low socioeconomic status Black women are more likely to be treated with primary radiation / chemotherapy, less likely to undergo full surgery, minimally invasive surgery Older women, low volume hospitals, Medicaid/MediCal less likely to receive guideline-based care Fleming et al, PLoS One, 2014 Ward et al, CA Cancer Clin J 2004 Uppal et al, Gynecol Oncol 2016 11 Helen Diller Family Comprehensive Cancer Center 12 Helen Diller Family Comprehensive Cancer Center
Delivery of Radiation Therapy Disparities in Primary RT/Chemo for Cervical Cancer • Brachytherapy • Chemosensitization National Cancer Database: 51% utilization of brachytherapy • Timing UCSF ACS CoC 2015 Benchmark Radiation therapy completed within 60 days of 100% initiation of radiation among women diagnosed with 81% (n=12/12) any stage of cervical cancer [CERRT] Chemo administered to cervical cancer patients who Cervix received raddiation for stages IB2-IV (Group 1) or 100% 90% with + pelvic LN, + surgical margin, &/or + (n=29/29) parametrium (Group 2) [CERCT] Use of brachytherapy in patients treated with 98% primary radiation with curative intent in any stage of 69% (n=46/47) cervical cancer [CBRRT] Korenaga et al, WAGO 2018 Source: UCSF Cancer Registry & ACS CoC 13 Helen Diller Family Comprehensive Cancer Center 14 Helen Diller Family Comprehensive Cancer Center Improving prevention & screening What’s New isn’t always better Promotion of HPV vaccination LACC Trial: Phase III trial of Open versus Minimally Invasive Radical Hysterectomy for Stage IA1-IB2 cervical CA • 41% completion by females at Kaiser • Methods: 740 patients for 90% power to declare noninferiority in • Asians: 1.29 OR, Hispanics: 0.82 OR, Black 0.53 OR DFS at 4.5 years with a margin of 7.2% ‒ Higher adherence in younger girls, less acculturated Latinas • Study closed at 631 patients, median follow-up of 2.5 years. Self sampling of HPV ‒ MIS: 16% robotic, 83% laparoscopic • 20% completed self -collected Pap smears, versus 6% • MIS was associated with worse overall survival (97% versus 86%, HR 6.0, 95% CI 1.48-20.3, p = 0.004) and disease free • 2.7% positive for HPV 16/18 survival (HR 3.74, 95% CI 1.63-8.58, p = 0.002) Freeman et al, Obstet Gynecol 2018 Sultana et al, Int J Cancer, 2016 Ramirez et al, SGO 2018 15 Helen Diller Family Comprehensive Cancer Center 16 Helen Diller Family Comprehensive Cancer Center
Endometrial Cancer Minimally Invasive Surgery & Adjuvant therapy UCSF ACS CoC Modifiable risk factors 2015 Benchmark • Obesity Endoscopic or Laparoscopic, robotic, or converted to ‒ Impacting minimally invasive surgery, efficacy of 96% open surgery performed for all endometrial cancer, for 75% chemotherapy & radiation (n=97/101) all stages [ENDLRC] Endometrium • Diabetes • Black women were less likely to receive surgery (OR 0.38) Chemotherapy and/or radiation administered to 90.5% ‒ Even after adjusting for age, stage, region, income, patients with Stage IIIC or IV endometrial cancer 85.5% (n=19/21) comorbidities [ENDCTRT] Black women have higher mortality (OR 1.6-2.9) and more high-risk disease Doll et al, Am J Obstet Gynecol, 2017 Source: UCSF Cancer Registry & ACS CoC Modesitt et al, Obstet Gynecol Surv, 2005 17 Helen Diller Family Comprehensive Cancer Center 18 Helen Diller Family Comprehensive Cancer Center Laparoscopy vs. Laparotomy Role of Gynecologic Oncologist GOG LAP2 SEER database, linked to Medicare • Randomized trial of laparoscopy vs. laparotomy for comprehensive surgical staging of uterine cancer •n=18,338 Endometrial cancer patients, Stage I-IV, • N=2616 (920 lap, 1696 L/S), 1996-2005 1991-2002 78% vs 86% complete staging 23% conversion to open, influenced by age, obesity Multivariate Analysis for Survival Median OR time: 3.3 vs. 2.2hrs Hazard Ratio Confidence Interval P-value Median LOS: 3 vs. 4 days Age at diagnosis 1.04 (1.04 - 1.05) <0.001 Laparoscopy with less pneumonia, ileus Stage 5.89 (5.16 - 6.72) <0.001 3 year recurrence: 11.3 vs. 10.2% Grade 2.87 (2.52 - 3.28) <0.001 5-year survival: 89.8% in both groups Gynecologic oncologist 0.71 (0.62 - 0.82) 0.001 Walker et al, J Clin Oncol 2009 Chan et al, J Clin Oncol 2011 Walker et al, J Clin Oncol 2012 Helen Diller Family Comprehensive Cancer Center Helen Diller Family Comprehensive Cancer Center
Endometrial CA: Role of Gyn Oncologist Calling a Gynecologic Oncologist • Surgical staging not readily available Disease specific survival, Stage II-IV disease • Preoperative high risk histology • Cervical or extra-uterine disease • (+) washings Survival • Unexpected endometrial CA on final path (percent) • Recurrent disease Yes GynOnc=79% • Non-operative therapy considered No GynOnc= 73% P=0.001 Time (years) Chan et al, J Clin Oncol 2011 Helen Diller Family Comprehensive Cancer Center Helen Diller Family Comprehensive Cancer Center Treatment Guidelines can also be Diverse Ovarian Cancer Access to high quality care, involving complex surgical & medical management • Non-adherence associated with Black race, low socio-economic status, low volume hospital, low volume surgeon • High volume surgeons are associated with urban settings Access to clinical trials • Low enrollment associated with non-White race, Medicaid/MediCal, low English proficiency Bristow et al, J Natl Cancer Inst, 2013 Mishkin et al, Gynecol Oncol 2016 23 Helen Diller Family Comprehensive Cancer Center 24 Helen Diller Family Comprehensive Cancer Center
Do the Right Ovarian Cancer Surgery Stick with the Guidelines Retrospective cohort study of Stage IIIC-IV ovarian cancer through SEER-Medicare database, 1992-2009. UCSF ACS CoC 2015 Benchmark Primary outcome of adherence to NCCN treatment guidelines for surgery, chemotherapy Salpingo-oophorectomy with N=10,296. Median follow-up: 57 mo. Median survival: 18 mo. omentectomy, debulking, Ovary 81% Overall, 30.2% received guideline adherent care. 69% cytoreductive surgery, or pelvic (n=30/37) exenteration in Stages I-IIIC ovarian 31% whites, 19% blacks, 32% Asians, 25% Hispanics, p < 0.001 cancer [OVSAL] Inverse association with non-adherent care and socioeconomic status Median survival for guideline adherent care: 36 mo. HR 1.69 for non-adherence (95% CI 1.60-1.79) Source: UCSF Cancer Registry & ACS CoC Bristow et al, Obstet Gynecol 2015 25 Helen Diller Family Comprehensive Cancer Center 26 Helen Diller Family Comprehensive Cancer Center Asians versus Caucasians Genetic Counseling & Testing SEER database review of epithelial ovarian cancer between 1988- 53% of ovarian cancer patients are currently offered genetic 2009 counseling and testing. 36% counseled, 33% tested N = 52,260. 3932 Asian, 48,328 white Mean time from diagnosis to counseling: 4.6mo. Median age of diagnosis: 56 vs. 64, p < 0.001 Barriers: race, language, insurance, referral process On multivariate analysis, age, race, surgery, stage, tumor grade were all independently predictive of 5 year disease specific survival Fuh et al, Gynecol Oncol 2015 Manrriquez et al, Gynecol Oncol 2018 27 Helen Diller Family Comprehensive Cancer Center 28 Helen Diller Family Comprehensive Cancer Center
Recommend
More recommend