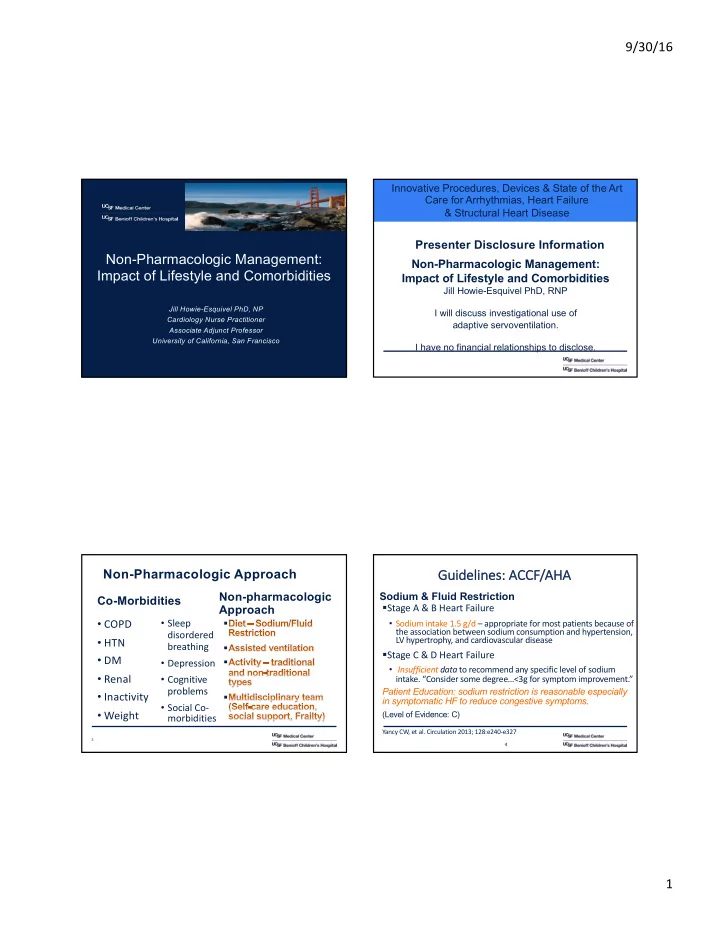
9/30/16 Innovative Procedures, Devices & State of the Art Care for Arrhythmias, Heart Failure & Structural Heart Disease Presenter Disclosure Information Non-Pharmacologic Management: Non-Pharmacologic Management: Impact of Lifestyle and Comorbidities Impact of Lifestyle and Comorbidities Jill Howie-Esquivel PhD, RNP Jill Howie-Esquivel PhD, NP I will discuss investigational use of Cardiology Nurse Practitioner adaptive servoventilation. Associate Adjunct Professor University of California, San Francisco I have no financial relationships to disclose. Guidelines: ACCF Gu CCF/AH AHA Non-Pharmacologic Approach Non-pharmacologic Sodium & Fluid Restriction Co-Morbidities § Stage A & B Heart Failure Approach • Sleep • COPD • Sodium intake 1.5 g/d – appropriate for most patients because of § the association between sodium consumption and hypertension, disordered LV hypertrophy, and cardiovascular disease • HTN breathing § § Stage C & D Heart Failure • DM • Depression § • Insufficient data to recommend any specific level of sodium • Renal • Cognitive intake. “Consider some degree…<3g for symptom improvement.” problems Patient Education: sodium restriction is reasonable especially • Inactivity § in symptomatic HF to reduce congestive symptoms . • Social Co- • Weight (Level of Evidence: C) morbidities Yancy CW, et al. Circulation 2013; 128:e240-e327 3 4 1
9/30/16 HF HFpEF Sod Sodium Restrict ction on in in St Stab able HF § 12 week prospective RCT, N=97, NYHA class II-IV § Medically optimized, previous signs of fluid retention § Fewer data on either > 40mg furosemide (NYHA III-IV) or >80mg (NYHA II-IV) § In clinical practice -assumption that excess sodium is associated with fluid retention and § Randomized to either Na 2-3g/d & fluid 1.5L/d hospitalization (individualized sodium restriction) or usual nurse-led HF information § Excess sodium restriction is associated with § Composite primary endpoint: NYHA functional class, worsening neuro-hormonal response hospitalization, weight, peripheral edema, quality of life, thirst, and diuretic use Volpe M. et al. Circulation. 1993;88:1620–7 . Philipson H, et al, Eur J Heart Failure 2013; 15 (11):1304-10 5 Compared Improved and Deteriorated Patients He Heart Failure Adherence and Retention Trial (HART) Re § N=902 (833 had Na data) 2001-04, NYHA class II-III, followed over median 36 months § Compared self-management counseling versus education alone § 18, 2 hour group meetings with 10 pts over 1 year using Tipsheets endorsed by AHA § Propensity scoring was used to match pts for disease severity, diuretic use, EF, co-morbids, medical therapy. 51% improvement in the composite endpoint in the § Sodium restricted group defined as <2500mg/d vs >2500mg/d intervention grp vs 16% in control mostly due to NYHA class, and LE edema; No negative effects: QOL, thirst, § Endpoint: death or HF hospitalization appetite- no sig diff between groups in rehosp Philipson H, et al, Eur J Heart Failure 2013; 15 (11):1304-10 Doukky et al, J Am Coll Cardiol HF 2016;4:24–35 2
9/30/16 Sodium & Fluid Restriction ADHF He Heart Failure Adherence and Re Retention Trial (HART) Examined: Weight loss, Clinical stability, Thirst perception, Readmissions § Sodium restriction associated with sig risk of death or HF hospitalization (42.3% vs. 26.2%; hazard ratio 1.85) § Non-significant increase in the rate of cardiac death Doukky et al, J Am Coll Cardiol HF 2016;4:24–35 Aliti et al. JAMA Intern Med. 2013;173(12):1058-1064. Aggressive Fluid and Sodium Restriction in Acute Decompensated Aggressive Fluid and Sodium Restriction in Acute Decompensated Heart Failure: A Randomized Clinical Trial Heart Failure: A Randomized Clinical Trial -No effect on wt, stability - Increased Thirst in intervention group Figure 2. Change in body weight from baseline to 3-day reassessment and from baseline to the end of the study period in the intervention and control groups. Alti et al. JAMA Intern Med. 2013;173(12):1058-1064. doi:10.1001/jamainternmed.2013.552 Alti et al. JAMA Intern Med. 2013;173(12):1058-1064. doi:10.1001/jamainternmed.2013.552 3
9/30/16 Positive Airway Pressure Therapy Features Sleep Disordered Breathing Guidelines : ACCF/AHA § Continuous positive airway pressure can be beneficial to increase LVEF and improve functional status in pts with HF and sleep apnea (Level of Evidence: B) Yancy CW, et al. Circulation 2013; 128:e263 Cowie M, et al. Cardiac Failure Review 2015;1(1):16–24 CPAP in Central Sleep Apnea Canadian Trial of CPAP Treatment in Patients With Chronic Heart Failure & Central Early hazard vs late benefit Sleep Apnea - CANPAP Improved LVEF on survival § 258 patients with HF + CSA, age=63, LVEF 25, NYHA II (67%) or III/IV (33%) § Randomly assigned to CPAP or no CPAP and followed for mean of 2 years § Endpoints: sleep, EF, exercise capacity, QOL, neurohormones, survival Cpap improved CSA, norepinephrine levels, oxygenation, EF, and increased 6MWT distance but did not affect QOL, no diff in survival btwn grps Bradley et al. NEJM 2005:353 (19): 2025-33 Bradley et al. NEJM 2005:353 (19): 2025-33 4
9/30/16 Adaptive Servo-Ventilation for Central Adaptive Servo-Ventilation Sleep Apnea in HFrEF- SERVE-HF Positive airway pressure ventilation that continuously § 1325 patients with HFrEF + Central Sleep monitors the patient's breathing Apnea, AHI 15 or more/hr pattern using an algorhythm § ASV vs guideline med tx (control) •Designed to detect episodes of • Age 69 yrs, NYHA II (30%), III or IV (70%), BMI sleep apnea and intervene to 28.5 maintain breathing at 90% of what had been normal for that § Any-cause death or life-saving cardiovascular individual just prior to episode intervention (txp, vad, shock, hosp) Inspiratory pressure on top of expiratory positive airway pressure American Sleep Association: Cowie MR et al. N Engl J Med 2015;373:1095-1105 https://www.sleepassociation.org/adaptive-servo-ventilation/ Adaptive Servo-Ventilation for Central CAT- HR Trial Sleep Apnea in HFrEF § Prospective, RCT, SDB (CSA or OSA) + ADHF § Used adaptive servo-ventilation § HFrEF OR HFpEF § N=215 expected enrollment § Endpoint death, CV hospitalization, 6MWD § All-cause and CV mort were ASV group § Stopped early (N=126) due to safety concerns for pts with HFrEF (LVEF<45%) Cowie MR et al. N Engl J Med 2015;373:1095-1105 Fiuzat et al. Contemp Clin Trials 2016;47:158-64 5
9/30/16 Ong Ongoing ng Tr Trial wi with AS ASV Obesity: Guidelines? • Results expected § ADVENT HF 2016 • CSA or OSA + CHF ACCF/AHA (2013) • AHA Stage B-D, LVEF < 45% No specific recommendation • 860 patients; Europe, N. America • Endpoint-driven with expected minimum 2 year f/u • All cause death or HF hospitalization • Still enrolling Yancy CW, et al. Circulation 2013; 128:e240-e327 The Obesity Paradox in Heart Failure Bariatric Surgery in HF Obese people with heart failure Obese people are more likely to live longer than normal or develop heart failure underweight people The presence of CHF increases the operative mortality risk from bariatric surgery 7-fold Kenchaiah S, et al. NEJM 2002;347:305-13 Benotti P, et al. Ann Surg 2014;259(1):123-30 Horwich TB, et al. JACC 2001;38:789-95 6
9/30/16 Efficacy and Safety of Exercise Training in Patients With Chronic Heart Failure: Exercise Training in Heart Failure HF-ACTION Randomized Controlled Trial Guidelines ACCF/AHA N=2331, mean EF 25%, 3 months of exercise vs usual care § Class I Exercise training (or regular physical activity) is recommended as safe and effective for patients with HF who are able to participate to improve functional status. (Level of Evidence: A) § Class IIa Cardiac rehabilitation can be useful in clinically stable patients with HF to improve functional capacity, exercise duration, HRQOL, and mortality. (Level of Evidence: B) Modest significant reductions for both all-cause mortality or hospitalization and cardiovascular mortality or heart failure hospitalization Yancy CW, et al. Circulation 2013; 128:e264 O ’ Connor CM, et al. JAMA. 2009;301(14):1439-1450. Yoga in Heart Failur e Efficacy and Safety of Exercise Training in Patients With Chronic Heart Failure: HF-ACTION Randomized Controlled Trial § Pullen (2010) – N=40 AA 12-weeks of yoga • Improved peak VO2, QoL, inflammatory markers, and flexibility § Howie-Esquivel (2010)– N=12 Modified Yoga in HF • Increased QOL, 6MWT, muscle strength § Selman (2015) – N=15 Tele-yoga in HF and COPD pts participated in yoga viewed at home • less social isolation and high enjoyment of the yoga § Gomes-Neto (2014)- “Meta-Analysis” 2 studies (N=59), effects of yoga on exercise capacity and QOL • Improved peak VO2 and QOL KCCQ - P = .001 for treatment effect for both ischemic and non-ischemic heart failure. . § Krishna (2014) – N=92 RCT over 12 weeks • Increased LVEF (36%), NT pro-BNP Flynn KE, et al. JAMA. 2009 Apr 8;301(14):1451-9 7
Recommend
More recommend