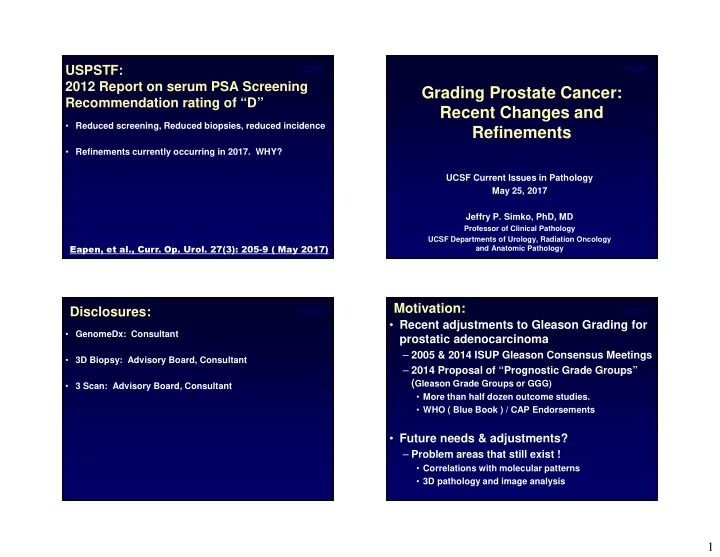
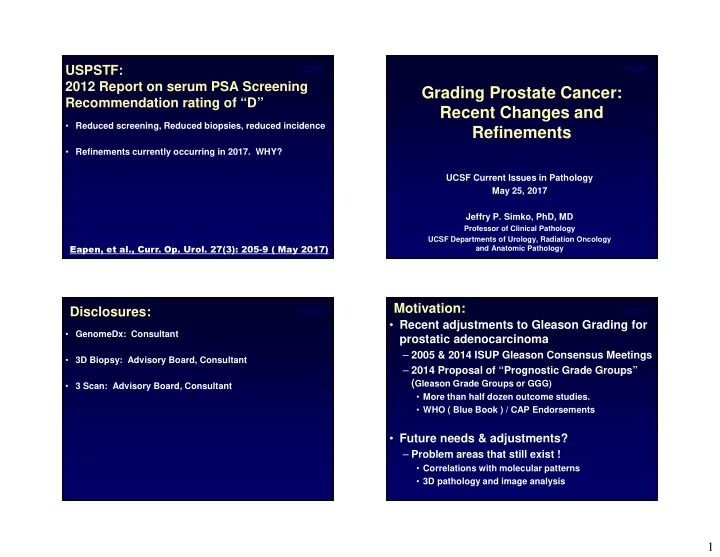
UCSF UCSF USPSTF: 2012 Report on serum PSA Screening Grading Prostate Cancer: Recommendation rating of “D” Recent Changes and • Reduced screening, Reduced biopsies, reduced incidence Refinements • Refinements currently occurring in 2017. WHY? UCSF Current Issues in Pathology May 25, 2017 Jeffry P. Simko, PhD, MD Professor of Clinical Pathology UCSF Departments of Urology, Radiation Oncology and Anatomic Pathology Eapen, et al., Curr. Op. Urol. 27(3): 205-9 ( May 2017) Motivation: UCSF UCSF Disclosures: • Recent adjustments to Gleason Grading for • GenomeDx: Consultant prostatic adenocarcinoma – 2005 & 2014 ISUP Gleason Consensus Meetings • 3D Biopsy: Advisory Board, Consultant – 2014 Proposal of “Prognostic Grade Groups” ( Gleason Grade Groups or GGG) • 3 Scan: Advisory Board, Consultant • More than half dozen outcome studies. • WHO ( Blue Book ) / CAP Endorsements • Future needs & adjustments? – Problem areas that still exist ! • Correlations with molecular patterns • 3D pathology and image analysis 1
Grading Cancers of the Prostate: UCSF UCSF Grading Systems (more than 40): • Prostatic adenocarcinoma (> 99%) Architecture vs. Cytology vs. Combinations – Acinar type • atrophic, foamy, pseudohyperplastic, others – Ductal type – Mucinous type – Vacuolated type (signet ring cell-like) • Other carcinoma and malignant tumor types (essentially all are high grade. Many Treatment-Related?) – Urothelial carcinoma – Squamous cell carcinoma – Small cell carcinoma – Adenosquamous carcinoma Urol Surg Pathol 1 st Ed. (Elsevier, Bostwick & Eble: 1996) – Metaplastic carcinoma / carcinosarcoma and sarcomas Gleason Grading: UCSF UCSF Original Gleason System “The most important tissue-based prognostic and predictive factor” (WHO Blue Book, 2016) • Formulated 60’s, validated 70’s, continued valids. Not accepted by WHO until 2003! – Architecture alone (not cytology) – Tumor heterogeneity is taken into account • Predicts stage, treatment outcomes, recurrence, progression and death! • Grades: 1 - 5 based on gland growth patterns • Grade X + Grade Y = Score ( sum: 2-10 ) • Profound effects on Management – Active surveillance ( No pattern 4 ? ) X = Most common tumor growth pattern (primary grade) – Type of radiation? Y = Second most common pattern (Secondary grade) If Y < 5% (< 3%) of total tumor, then repeat X. • + / - Anti-androgens – Adjuvant therapy post prostatectomy ? For Primary tumor ( Not for treated tumor or METs. ) 2
UCSF UCSF DF Gleason, 1966 UCSF UCSF Gleason pattern 1: Gleason Pattern 2: • Circumscribed nodule of uniform glands • Regular or irregular glands in a less • Uniform glands with no fusion ( fusion is 4) circumscribed nodule. • Never call on Bx, only RP • No intervening benign glands (that is 3) • Extremely rare, usually other patterns too • Individual glands, no fusion (fusion is 4) Prostate Bx. Int. 3 rd ed. (Epstein & Yang, 2002) 3
UCSF UCSF UCSF UCSF Gleason pattern 3: • Individual glands infiltrating benign • Irregular distribution (not uniform) • Regular distribution OK if B9 incorporated Prostate Bx. Int. 3 rd ed. (Epstein & Yang, 2002) Prostate Bx. Int. 3 rd ed. (Epstein & Yang, 2002) 4
UCSF UCSF Prostate Bx. Int. 3 rd ed. (Epstein & Yang, 2002) UCSF UCSF DF Gleason, 1977 Prostate Bx. Int. 3 rd ed. (Epstein & Yang, 2002) 5
UCSF UCSF Prostate Bx. Int. 3 rd ed. (Epstein & Yang, 2002) UCSF UCSF Gleason Pattern 4: • Gland fusion – Cribriform (glomerulations) – Sinuating small glands in chains or cords – Poorly formed glands ? • High grade tumor (changes Rx options) Prostate Bx. Int. 3 rd ed. (Epstein & Yang, 2002) 6
UCSF UCSF UCSF UCSF Jesses comments. Prostate Bx. Int. 3 rd ed. (Epstein & Yang, 2002) 7
UCSF UCSF UCSF UCSF 8
UCSF UCSF Gleason Pattern 5: • Single cells, solid sheets or necrosis in 4 • Vacuoles are not pattern 4! Prostate Bx. Int. 3 rd ed. (Epstein & Yang, 2002) Prostate Bx. Int. 3 rd ed. (Epstein & Yang, 2002) UCSF UCSF McKenney, et al., Am J Surg Pathol 40: 1439 (2016) Prostate Bx. Int. 3 rd ed. (Epstein & Yang, 2002) 9
UCSF UCSF UCSF UCSF 10
UCSF UCSF More sclerotic. UCSF UCSF Dolphining McKenney, et al., Am J Surg Pathol 40: 1439 (2016) 11
UCSF UCSF Prostate Bx. Int. 3 rd ed. (Epstein & Yang, 2002) UCSF UCSF Treated Carcinoma: • Post radiation and/or anti-androgen Rx. • Atrophic, associated inflammation, changes in the benign. • ONLY grade if treatment changes not seen! – Sometimes both treated & untreated (report). 12
UCSF UCSF Grading Variants: Use the Gleason growth pattern • Variants and subtypes not well-defined. – Classic examples, OK, BUT borders, continuum • Acinar variants and subtypes. • Outcome data supports this. UCSF UCSF 13
UCSF UCSF UCSF UCSF 14
UCSF UCSF UCSF UCSF treated issues. 15
UCSF UCSF McKenney, et al., Am J Surg Pathol 40: 1439 (2016) UCSF UCSF Vacuoles all of them. 16
UCSF UCSF Gleason Modifications: ISUP • International Society of Urologic Pathologists Consensus Meetings: 2005, 2014 – Dozens of prostate pathologists at the meetings • Treating clinicians also attended the 2014 meeting Subtypes foamy, muycinous, – Identify common areas: Consensus statements pseudohyperplastic, atrophic. – Identify areas of confusion: Experiments to clarify • 2005 results criticized for no outcome data! • Outcome studies have now validated virtually all • Increased consistency in grading ( cribriform ) UCSF UCSF Problems with original Gleason (2005 & 2014 ISUP) • Some patterns are extremely rare / not cancer? RARE – Grade 1 likely adenosis (Basal Cell IHC) – Grade 2 Rare / Can’t Dx on small needle Bx • Not all possible growth patterns represented – Inter-observer variability; degraded prognostics • Some descriptions vague – Cribriform 3 vs. Cribriform 4 – Inter-observer variability; degraded prognostics • No rules for when more than two patterns 17
UCSF UCSF Problems with original Gleason (2005 & 2014 ISUP) • Some patterns are extremely rare / not cancer – Grade 1 likely adenosis – Grade 2 Rare / Can’t Dx on small needle Bx • Some descriptions vague – Cribriform 3 vs. Cribriform 4 – Inter-observer variability; degraded prognostics • Not all growth patterns represented ( glomerulations) – Inter-observer variability; degraded prognostics Prostate Bx. Int. 3 rd ed. (Epstein & Yang, 2002) • No rules for when more than two patterns UCSF UCSF RARE Jesses comments. 18
UCSF UCSF Gleason Modifications: ISUP Problems with original Gleason (2005 & 2014 ISUP) Scoring rules changed to better represent biology • Some patterns are extremely rare / not cancer – Grade 1 likely adenosis – Grade 2 Rare / Can’t Dx on small needle Bx • Bx, primary grade + worst = score, not secondary • Some descriptions vague • In Bx, if secondary lower grade and < 5%, ignore – Cribriform 3 vs. Cribriform 4? – Inter-observer variability; degraded prognostics • Prostatectomy, score discreet tumors of different grades separately. • Not all possible growth patterns represented – Inter-observer variability; degraded prognostics!!! • Recommend reporting percent > pattern 3. • No rules for when more than two patterns Modified Gleason -> UCSF UCSF Grade Groups: Problems in Clinic: • Developed by Hopkins Group (J. Epstein) • Grade Migration (perceived upgrading?) • No formal name yet. – ”BEST” score now 3+3 = 6 on scale 2-10. – Endorsed by WHO: WHO Grade Groups ? – Gleason Grade Groups (GGG). – Confusing to patients – Difficult to explain • Based on using modified Gleason grades. – Patient anxiety precluding conservative management – ISUP 2005 and ISUP 2014 consensus conferences • Patient and clinician frustration! • 3+4=7 and 4+3=7 same score, but very different outcome!!! • How does this system relate to Gleason grades and patient outcomes? • How to apply this reporting system to practice? 19
UCSF UCSF How to apply Grade Groups: Grade Groups (Epstein): • ISUP modified Gleason Grades works best • Grade Group 1 = Gleason score < 7 • Grade Group 2 = Gleason score 3+4 = 7 • Developed using Biopsy with highest score • Grade Group 3 = Gleason score 4+3 = 7 – Subsequent study showed that using overall Bx grade • Grade Group 4 = Gleason score 8 (4+4, 3+5, 5+3) group or highest Bx grade group gave similar prognosis • Grade Group 5 = Gleason score > 8 (4+5, 5+4, 5+5) (Berney et al., Br J Cancer Apr 21, 2016 epub) • Prostatectomy: If Grade 5 > 5%, then secondary • Validated in numerous f/u studies – Does not strictly follow ISUP! • Endorsed by WHO and CAP – Probably works either way. • UCSF Data: • Simple translation from Gleason score to GGG – 4+3=7 and 4+4=8 same – Clinicians can easily translate to grade groups – 4+5, 5+4 same, 5+5 worse (unpubl.) – Keeps report cleaner / less confusion PROSTATECTOMY UCSF UCSF Pierorazio, et al. Br J Urol Int 111: 753-60 (2013). Pierorazio, et al. Br J Urol Int 111: 753-60 (2013). 20
Recommend
More recommend