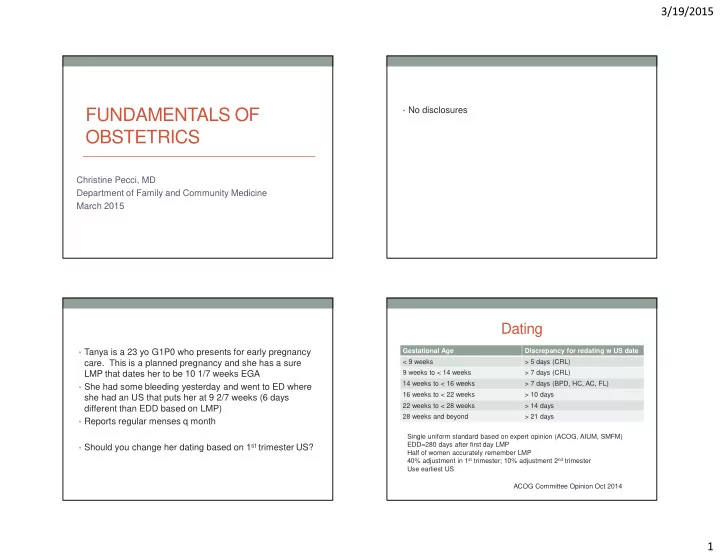
3/19/2015 • No disclosures FUNDAMENTALS OF OBSTETRICS Christine Pecci, MD Department of Family and Community Medicine March 2015 Dating Gestational Age Discrepancy for redating w US date • Tanya is a 23 yo G1P0 who presents for early pregnancy < 9 weeks > 5 days (CRL) care. This is a planned pregnancy and she has a sure 9 weeks to < 14 weeks > 7 days (CRL) LMP that dates her to be 10 1/7 weeks EGA 14 weeks to < 16 weeks > 7 days (BPD, HC, AC, FL) • She had some bleeding yesterday and went to ED where 16 weeks to < 22 weeks > 10 days she had an US that puts her at 9 2/7 weeks (6 days 22 weeks to < 28 weeks > 14 days different than EDD based on LMP) 28 weeks and beyond > 21 days • Reports regular menses q month Single uniform standard based on expert opinion (ACOG, AIUM, SMFM) • Should you change her dating based on 1 st trimester US? EDD=280 days after first day LMP Half of women accurately remember LMP 40% adjustment in 1 st trimester; 10% adjustment 2 nd trimester Use earliest US ACOG Committee Opinion Oct 2014 1
3/19/2015 Will my baby be normal? • We confirm that Tanya has a “sure” LMP • She has been reading about a new test for making sure the baby is normal. She wants to know if you can order • We will calculate her EDD based on her LMP this test. Will having a normal test guarantee that this • US discrepancy is 6 days but between 9-14 weeks we baby will be okay? would use the US based EDD only if it differs by >7 days Aneuploidy Screening Non-invasive Prenatal Testing (NIPT) • First trimester 10-15 weeks • Cell free fetal DNA • Serum testing (free bhg + PAPP-A) • Comes from placental cells and clears from maternal • Ultrasound (Nuchal transluncey) system in hours • Tests for Trisomy 18, 21, 13 • Second trimester screening 15-20 weeks • Can be checked 10 – 22 weeks gestation • Serum testing (AFP, inhibin, bhcg, estriol) • Only for high risk patients • Ultrasound (fetal survey) • Age >35, abn US, history of trisomy, parent with balanced translocation • Sequential vs integrated testing • If positive result, refer to genetic counseling and offer • NOT diagnostic (need CVS or Amniocentesis) invasive testing • False positive 0.5%, 98-99% Trisomy 21 detected 2
3/19/2015 Staying Healthy IOM weight gain guidelines Exercise in Pregnancy PrePreg BMI BMI Total Weight Gain • Goal: 30 minutes most days of the week Underweight <18.5 28-40 • If sedentary, start out slowly i.e. 5 min daily Normal 18.5-24.9 25-35 • Avoid contact sports or high risk of falling Overweight 25.0-29.9 15-25 • Avoid sports that involve balance changes Obese >30 11-20 • No scuba diving • Keep off back, drink lots of water • Listen to your body Institute of Medicine 2009 3
3/19/2015 I love my hot dogs! Nutrition in Pregnancy Folic Acid: 600 mcg folic acid • Pregnant women more likely to be affected Iron: 27 mg • Avoid refrigerated smoked seafood, pate, unpasteurized Calcium: 1000-1300 mg milk/cheese Vit D: 600 IU • Deli meats/hot dogs need to be steaming hot ACOG Sept 2013 I love my cat! I’m glad I don’t like fish! • Ingestion of raw/undercooked meat, unwashed • Fish is good for you and provides necessary nutrients for fruits/vegetables, soil or litter contaminated with cat feces growing fetus • Wash hands • Should eat on average two meals a week • Have someone else clean cat litter • Avoid swordfish, tilefish, king mackerel, shark • Use gloves • Change litter box daily • Do not feed raw meat to cats 4
3/19/2015 Preeclampsia: Diseases in Pregnancy You will see it! And it matters… • Incidence 2-8% • Has increased by 25% in last two decades • More likely in patients with hypertension • Unrecognized has serious health consequences for mom and baby • Risk factor for future CV and metabolic disease Task Force for Hypertension in Pregnancy, 2013 Task Force for Hypertension in Categories Pregnancy, 2013 • Preeclampsia-eclampsia • With or without severe features • 17 experts (OB, MFM, htn, nephrology, anesthesia, physiology, patient advocacy) • Chronic hypertension • Changes in terminology • Gestational hypertension- hypertension without proteinuria after 20 week • Changes in management • Chronic hypertension with superimposed preeclampsia Task Force for Hypertension in Pregnancy, 2013 5
3/19/2015 Diagnosis Proteinuria • >140/90 on two occasions 4 hours apart • >300 mg /24 hrs • Spot urine: creatinine ratio > 0.3 • SEVERE FEATURES • Dipstick 1+ • >160/110 • Plts <100K • Proteinuria is classically part of the syndrome • LFTs twice normal • But NOT required to make diagnosis of preeclampsia • Persistent RUQ pain or epigastric pain • Creatinine >1.1 or double • Pulmonary edema • New onset cerebral or visual disturbance Who should take ASA? Management • Initiate ASA 81 mg in late first trimester • Chronic hypertension • History of preeclampsia < 34 0/7 weeks • Deliver after 38 0/7 wks • Preeclampsia in more than one pregnancy • Gestational hypertension: • Patient with history of preeclampsia <34 wks. • Deliver at 37 0/7 weeks • Prevalence 40% • weekly dip for proteinuria + BP check (can be at home) • NNT 1:20 (moderate Q; qualified SOR) • NST q week • NNT 1:500 low risk (prev 2%) • NNT 1:50 high risk (prev 20%) 6
3/19/2015 Management Intrapartum Interventions • Preeclampsia without severe features: • Mg with severe preeclampsia only (low/qual) • Deliver at 37 0/7 weeks • Anti hypertensive meds only for > 160/110 (mod/strong) • 2x week BP, once a week labs • Administer steroids prior to delivery (high/ strong) • 2x week NST • Preeclampsia with severe features • Deliver at 34 0/7 weeks • Monitor in hospital • Severe uncontrolled htn, eclampsia, pulm edema, abruption, DIC, NRFHR, IUFD • Immediate delivery after initial stabilization Postpartum follow-up Diabetes in Pregnancy • Incidence unknown • Overall incidence of diabetes in pregnancy 6% • 90% of these are GDM • ALL patient should receive education on warning signs • Hyperglycemia and Adverse Pregnancy Outcome (HAPO) • Check BP 72 hours post delivery and 7-10 days trials show continuous relationship- neonatal postpartum hyperglycemia, macrosomia • Treat for >150/100 on two occasions 4-6 hrs apart • Increased hyperbilirubinemia, operative delivery, shoulder • Preconception- glycemic control, weight loss dystocia ACOG Practice Bulletin Aug 2013 7
3/19/2015 Diagnosis Gestational Diabetes • Screen at 24-28 wks • 2013 NICHD recommends 2 step test (50 gm then 100 gm) • Consider prevalence of diabetes • Early screening- if prior GDM, known impaired fasting glucose, BMI >30 • Consider resources • One hour glucola: range 135-140 • 2010 International Association of Diabetes and Pregnancy fasting 1 hr 2hr 3hr Study Group (endorsed by ADA) (92, 180, 153) NDDG* 105 190 165 155 • No data regarding therapeutic intervention CC** 95 185 165 140 *National Diabetes Data Group **Carpenter Coustan Treatment Mode of delivery • QID finger sticks • Prevention of a single permanent brachial plexus palsy • Cesarean delivery for 4500 gm NNT 588 • ADA and ACOG 140 on 3 hr and 120 2 hr • Cesarean delivery for 4000 gm NNT 962 • Carbs 33-40% of diet • Protein 20%; fat 40% • Mod exercise • If fasting consistently >95, consider insulin • Insulin does not cross the placenta • Glyburide and metformin not approved but being used • Glyburide crosses placenta but no measurable levels in cord blood • ? Long term effects? No short term effects 8
3/19/2015 Postpartum follow-up Infections in Pregnancy • 15-50% with GDM develop DM 20+ years later • Varies by ethnicity (60% Latina within 5 years) • Fasting or 2 hr GTT 6-12 wk postpartum • IGT picked up by 2 hr • Repeat testing q 3 years if normal HSV HSV-Give prophylaxis at term • Genital herpes affects 20% women in US? • Primary infection transmission to neonate 30-60% at delivery • Recurrent infection transmission 3% at delivery; no lesions • Incidence of new infection in pregnancy 2% 2/10,000 • Women with recurrent HSV-75% can expect episode • Acyclovir, famcyclovir, valcyclovir all class B, most data on during pregnancy, 14% at delivery acyclovir • 80% of infected infants born to women with no reported • Routine screening not recommended history • Genital Sx or lesions- c/s decreases transmission from 7.2% to • 20% neonatal survivors have long-term neurosequalae 1.2% even after ROM • Acyclovir 400 mg TID @ 36 weeks til delivery 9
Recommend
More recommend