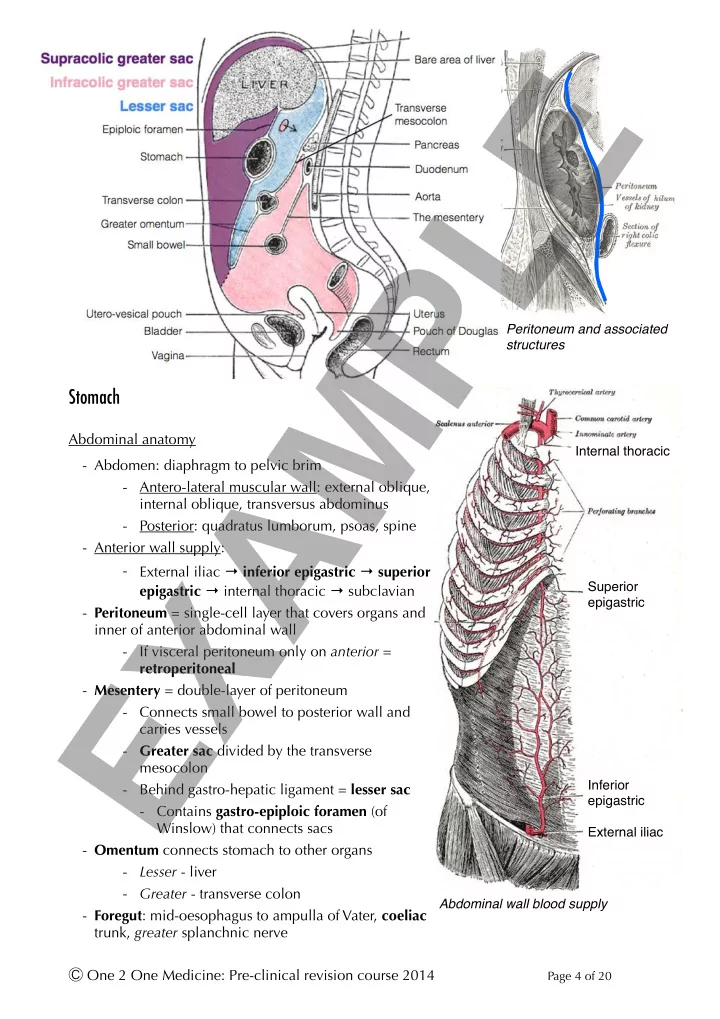
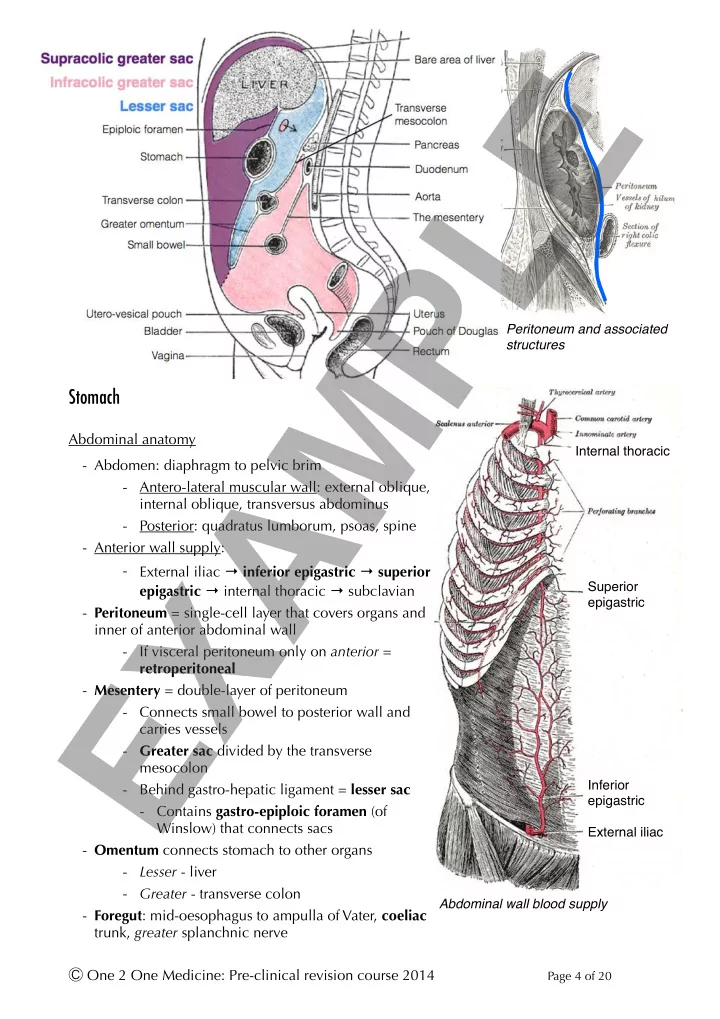
EXAMPLE Peritoneum and associated structures Stomach ! Abdominal anatomy Internal thoracic - Abdomen: diaphragm to pelvic brim - Antero-lateral muscular wall: external oblique, internal oblique, transversus abdominus - Posterior: quadratus lumborum, psoas, spine - Anterior wall supply: - External iliac → inferior epigastric → superior epigastric → internal thoracic → subclavian Superior epigastric - Peritoneum = single-cell layer that covers organs and inner of anterior abdominal wall - If visceral peritoneum only on anterior = retroperitoneal - Mesentery = double-layer of peritoneum - Connects small bowel to posterior wall and carries vessels - Greater sac divided by the transverse mesocolon Inferior - Behind gastro-hepatic ligament = lesser sac epigastric - Contains gastro-epiploic foramen (of Winslow) that connects sacs External iliac - Omentum connects stomach to other organs - Lesser - liver - Greater - transverse colon Abdominal wall blood supply - Foregut : mid-oesophagus to ampulla of Vater, coeliac trunk, greater splanchnic nerve Ⓒ One 2 One Medicine: Pre-clinical revision course 2014 Page ! of ! 4 20
- Midgut : to ⅔ rd transverse colon, superior mesenteric artery, lesser splanchnic nerve EXAMPLE - Hindgut : to dentate line (rectum), inferior mesenteric artery, least splanchnic nerve ! Stomach - Anterior : diaphragm, transverse colon, GIT embryology liver - Posterior : pancreas, spleen, kidney - Supply : right & left gastric, gastroepiploic, short gastric [splenic runs posterior] - Drain to splenic and superior mesenteric veins - Extra (external) oblique muscle layer - Functions: - Store & regulate release - Protein & vit B12 digestion - Immune defence - Cephalo-gastric and gastro-gastric Stomach anatomy reflexes inhibit vagal contraction to fill without pressure rise - Rugae also help filling without pressure increase Coeliac axis branches Ⓒ One 2 One Medicine: Pre-clinical revision course 2014 Page ! of ! 5 20
Lower oesophageal sphincter - Competent if sphincter pressure exceeds gastric pressure, contributing factors: EXAMPLE - Muscular (physiological) sphincter itself - Increase in intra-abdominal/-thoracic pressure with coughing, talking, exhalation - Acute angle between oesophagus & stomach with mucosal flaps - Gravity relatively minor role - Gastro-oesophageal reflux disease (GORD): pain, cough, regurgitation - Chronic oesophagitis may give Barrett's metaplasia (to gastric type) - Increased cancer risk Cell type Secretions Function Parietal cells Gastric acid and Denature protein, immune protection, pepsinogen intrinsic factor activation Chief cells Pepsinogen Protein digestion APUD (amine Somatostatin Inhibit acid and increase mucus production precursor uptake decarboxylase) cells G-cells Gastrin Increase acid production Mucus-secreting cells Alkaline mucus Protect epithelium from acid-damage ECL (entero- Histamine Increase acid production chromaffin-like) cells Gastric physiology - Parietal cells secrete H + via proton pump (H + - ATPase) made by carbonic anhydrase (on H 2 O) + CO 2 ) - Target for proton pump inhibitors (e.g. omeprazole) - Basolateral HCO 3- excretion (for Cl - ) makes alkaline tide - Control: - Vagal innervation of parietal cells increases directly - Indirectly: via gastrin from G-cells and Gastric acid secretion binds CCK B -receptor on parietal cells - Gastrin reduced by secretin (from duodenal S-cells in response to acid) - Histamine (ECL cells) increases acid production at H 2 -R on parietal cells - Target for histamine antagonists (e.g. ranitidine) - Somatostatin inhibits directly on parietal cells - Indirectly: via r educing histamine production from ECL cells - Mucus increased by ACh (therefore at same time as acid) using PGE 2 - Use of NSAIDs reduce PG production and predisposes to gastritis/ulcers Ⓒ One 2 One Medicine: Pre-clinical revision course 2014 Page ! of ! 6 20
Control of gastric acid EXAMPLE - Gastric motility Helicobacter pylori - Mixing in corpus - Propulsion moves towards - Bacterium specialised to living in stomach antrum - Associated with peptic ulcer disease - Retropulsion back from - Urease produces an alkaline coat antrum/pylorus to corpus - Flagella to bury into mucus - Pylorus relaxes in response - Inhibits somatostatin secretion → increases acid to: distention, small boluses, peptides ! Small bowel ! Anatomy - Duodenum: superior (coeliac) & inferior (SMA) pancreato-duodenal arteries - Posterior to 1 st : common bile duct, gastroduodenal artery and portal vein - Posterior to 2 nd : right kidney and ureter - 3 rd : around head of pancreas, crossed by root of the mesentery & SMA - 4 th : ligament of Trietz at duodeno-jejunal junction with IMV to left Duodenal anatomy - Histology: - Brunner's glands : deep, alkaline-secreting, only in duodenum Ⓒ One 2 One Medicine: Pre-clinical revision course 2014 Page ! of ! 7 20
- Simple columnar with microvilli - Jejunum (2/5 th ): thicker with smaller lumen - Plicae circulares (/valvulae conniventes) = folds in small bowel EXAMPLE - Villae (= mucosae) with crypts of Leiberkuhn at base (new cells produced at base) - Peyer's patches = lymphoid aggregates - B-cells make secretory IgA that prevent pathogen adhesion - Panneth cells secrete lysozyme - Peritoneal cavity has a greater and lesser sac, separated by the stomach and it’s attachments - Mesentery is double-layered peritoneum containing neurovascular supply - Gastric parietal cells produce acid using H + /K + -ATPase - Duodenum is retroperitoneal and is both fore - & mid - gut ! ! ! ! ! ! ! ! ! ! Absorption ! Sodium & water absorption in the small bowel Water & ions - Basolateral Na + /K + -ATPase gives concentration gradient for apical facilitated diffusion: co-transport with glucose, amino acids and chloride - Water via osmosis through leaky occluding junctions in upper GIT and small bowel - Large bowel through aquaporins and transcellular movement - More controlled - K + and Cl - move by paracellular transport ; plus H + /K + -ATPase absorbs K + in colon ! Ca 2+ - Facilitated uptake in duodenum - binds calbindin inside cells (keeps gradient) - Basolateral efflux by Ca 2+ -ATPase or Na + /Ca 2+ -antiporter - PTH increases channel activity and vitamin D increases calbindin synthesis ! Ⓒ One 2 One Medicine: Pre-clinical revision course 2014 Page ! of ! 8 20
Recommend
More recommend