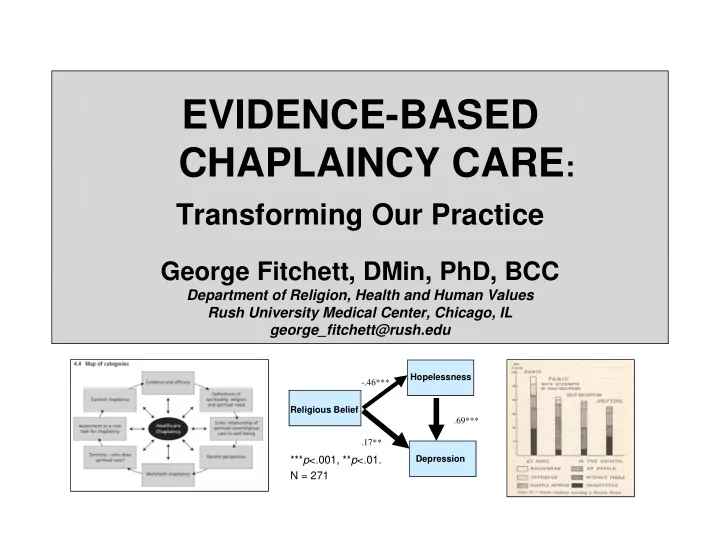
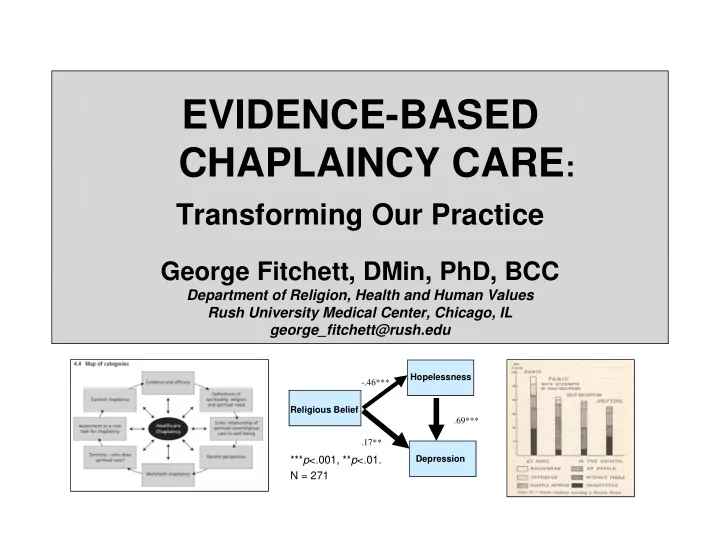
EVIDENCE-BASED CHAPLAINCY CARE : Transforming Our Practice George Fitchett, DMin, PhD, BCC Department of Religion, Health and Human Values Rush University Medical Center, Chicago, IL george_fitchett@rush.edu Hopelessness -.46*** Religious Belief .69*** .17** *** p <.001, ** p <.01. Depression N = 271
How Do We Know Good Spiritual Care? Tradition – We have always done it this way. Policy – This is the way we are supposed to do it. Education – I was taught to do it this way. Personal Experience/Trial and Error – I tried several ways and this this one works best. Intuition – Doing it this way feels right to me. Research – There is evidence this is the best way to do it. From Hundley, 1999
Chaplaincy: A Research-Informed Profession Standard 12: Research The chaplain practices evidence-based care including ongoing evaluation of new practices and when appropriate, contributes to or conducts research. (http://www.professionalchaplains.org)
Outline 1. Evidence-Based Care: What is it? 2. Evidence-Based Care: Against it & for it Hopelessness 3. Ways of Knowing: Religion and -.46*** Science Religious Belief .69*** 4. Types of Research Evidence .17** 5. Overview of Chaplaincy-Related *** p <.001, ** p <.01. Depression N = 271 Research 6. Next Steps for Research-informed Chaplaincy
What is Evidence-Based Spiritual Care? “Evidence-based spiritual care is the use of scientific evidence on spirituality to inform the decisions and interventions in the spiritual care of persons” Tom O’Connor (2002). Journal of Religion and Health
What is Evidence-Based Practice? Evidence-based practice in psychology is the integration of • the best available research with • clinical expertise • in the context of patient characteristics, culture, and preferences. APA Policy Statement on Evidence-Based Practice in Psychology, 2006
AGAINST Evidence-Based Spiritual Care It can’t be done God, the Spirit, presence, prayer, etc. are much too big and always will be mysteriously beyond our attempts to measure and quantify. (Stiger, 2002) It shouldn’t be done Once pastoral care services succumb to the need to prove they can decrease the length of stay or improve patient satisfaction all will be lost. (Sulmasy, 2006)
FOR Evidence-Based Spiritual Care “Evidence from research needs to inform our pastoral care. To remove the evidence from pastoral care can create a ministry that is ineffective or possibly even harmful” (O’Connor TSJ and Meakes E. 1998. The first article to use the term “evidence- based” pastoral care.) Good stewardship of creation requires our best, evidence-based, care (Grossoehme in Fitchett & Grossoehme, 2011)
Health Care Chaplaincy Improving our Care and Making our Case Through Research Hopelessness -.46*** Religious Belief .69*** .17** *** p <.001, ** p <.01. Depression N = 271
Source: Anton T. Boisen Explorations of the Inner World: A Study of Mental Disorder and Religious Experience ( Willett, Clark & Company, 1936)
Can Religion and Science Co-Exist? Conflict: opposite and antagonistic, conflict Mutual independence: separate and different Ian Barbour, Nature, Dialogue: meeting on Human Nature and God, 2002 boundaries Integration
Chaplaincy: A Research-Informed Profession Standard 12: Research The chaplain practices evidence-based care including ongoing evaluation of new practices and when appropriate, contributes to or conducts research. (http://www.professionalchaplains.org)
Chaplaincy: A Research-Informed Profession • Research Literacy All health care chaplains should be research literate • Research Collaboration Some health care chaplains will be qualified to collaborate in research conducted by health care colleagues (co-investigators) • Research Leadership Some health care chaplains will be qualified to lead research projects (principal investigators)
Chaplaincy: A Research-Informed Profession A research-literate chaplain has the ability to read, understand, and Hopelessness -.46*** summarize a Religious Belief .69*** research study and .17** *** p <.001, ** p <.01. Depression to explain its N = 271 relevance for his/her spiritual care.
Overview of Chaplaincy Research 1. Importance of R/S for patients 2. Patient/family R/S coping and R/S needs 3. Patient/family preferences for spiritual care 4. Describe what chaplains do 5. Effect of spiritual care on important outcomes
Reviews of Chaplaincy Research Mowat, Harriet (2008). The potential for efficacy of healthcare chaplaincy and spiritual care provision in the NHS (UK): A scoping review of recent research.
My faith or spirituality has helped me through my cancer experience Black (n=914) Hispanic (n=664) White (n=6827) 100% 88% 80% 80% 65% 60% 40% 20% 20% 15% 11% 9% 7% 5% 0% very much/quite a bit somewhat not at all/a little bit N=8,405, ACS SCS II; Canada et al. 2013
Religious Coping among Persons with Persistent Mental Illness (N=406) Religion helped to cope with symptom 65% severity (to a large or moderate extent) Religion became more important when 48% symptoms worsened Religious beliefs and activities were “the 30% most important things that kept [them] going” Tepper et al. (2001) Psychiatric Services, p. 662
Religious/Spiritual Perspectives of Adolescents & Young Adults Receiving BMT Believing God has a “He chose me ’cause I’m strong. I understand what reason I have to go through.” “And just when I’m in pain and I pray for peace. . . Using faith practices that side effects won’t be too bad.” Benefitting from spiritual “My pastor’s wife is one of the biggest helps support people because. . . she talks to me like I’m normal.” “We learned that AYA patients were utilizing R/S far more than we suspected. Our data. . . suggest that chaplains should be proactive in asking AYA patients about their understanding and use of faith.” Themes for 12 AYAs (age 15-28, 7 female, interviewed 2 weeks pre to 3 months post- transplant; 6 re-interviewed 1 yr post-transplant); Ragsdale et al., 2014
"I want to know more about this" 21 Pargament et al 2000
Percent with Item distress Not able to carry out important roles 37.5 Feeling no longer who I was 36.4 Feeling of not having control 29.2 Feeling uncertain 26.9 Distress in 253 Feeling a burden to others 24.1 Palliative Care Patients Feeling depressed 22.5 (90% Canadian, Worried about future 20.9 10% Australian) Feeling of unfinished business 19.4 Feeling life no longer has meaning or 17.4 Chochinov et al., 2009 purpose Not feeling worthwhile or valued 17.0 Feeling have not made meaningful 11.9 contribution Not being able to accept things as they 11.5 are Concerns regarding spiritual life 6.3
Spiritual Distress 50% with no or little distress 23% with distress in 3+ Chaplain ratings of spiritual distress for 113 palliative care in-patients at MD Anderson. Hui et al., 2011
Spiritual Distress in Older Medical Rehab Patients 65% some distress 27% some distress in all 5 dimensions 22% severe distress in at least one dimension 60% of severe unmet needs were for Life Balance From Monod et al., 2012; n=203 geriatric patients in medical rehabilitation, Switzerland
Screening for R/S Struggle BRIGHTEN Participants (n=188) Is R/S important to you as you cope with your illness? YES NO (82%) (18%) How much strength or Has there ever been a time comfort do you get from when R/S was important to your R/S right now? you? NO (9%) YES (9%) Less than I need or none All that I at all (41%) need (41%) R/S Struggle Path 1 R/S Struggle Path 2
Screening for Religious Struggle Delgado Guay et al., Study Mako et al, 2006 2011 Center Calvary Hospice, NYC MD Anderson Inpatients w advanced Palliative care outpt Patients cancer clinic Sample size 57 91 Yes % 61% 44% Median (IQR) 3 (1, 6) Mean 4.7 Are you experiencing spiritual pain right now? Spiritual pain is a pain deep in your soul (being) that is not physical How would you rate your overall spiritual pain 0 (none) – 10 (worst)?
Implications of Screening for Spiritual Pain IMPLICATION FOR QUESTION SPIRITUAL CARE How did you decide which patients to Good stewards of scarce see this week? resources How did staff you work with determine Protocol for screening and who to refer and who not to refer? referral What evidence did you generate this week that your spiritual care made a Accountability and difference in measurable patient documentation outcomes? Can estimate level of How many chaplains does your spiritual acuity and institution/service need? staffing needs
Interest in Spiritual Care (n= 364 oncology Predictors of Interest in outpatients, Israel) Spiritual Care OR Spirituality (ref = Not spiritual) Somewhat spiritual 4.17 Very spiritual 8.35 Religiousness (ref = Secular) Traditional 1.79 Religious 2.41 Prior experience with spiritual care (ref = No) Yes 3.9 Understand spiritual care (ref = No) Schultz et al., 2014 Yes 2.9
Preferences about Chaplain Visits* Want at least 1 visit 70% Daily visits 18% Visit every few days 38% Weekly visit 13% Not at all 17% Expect visit without requesting 39% *14% missing Piderman et al, 2010, N=1591
Recommend
More recommend