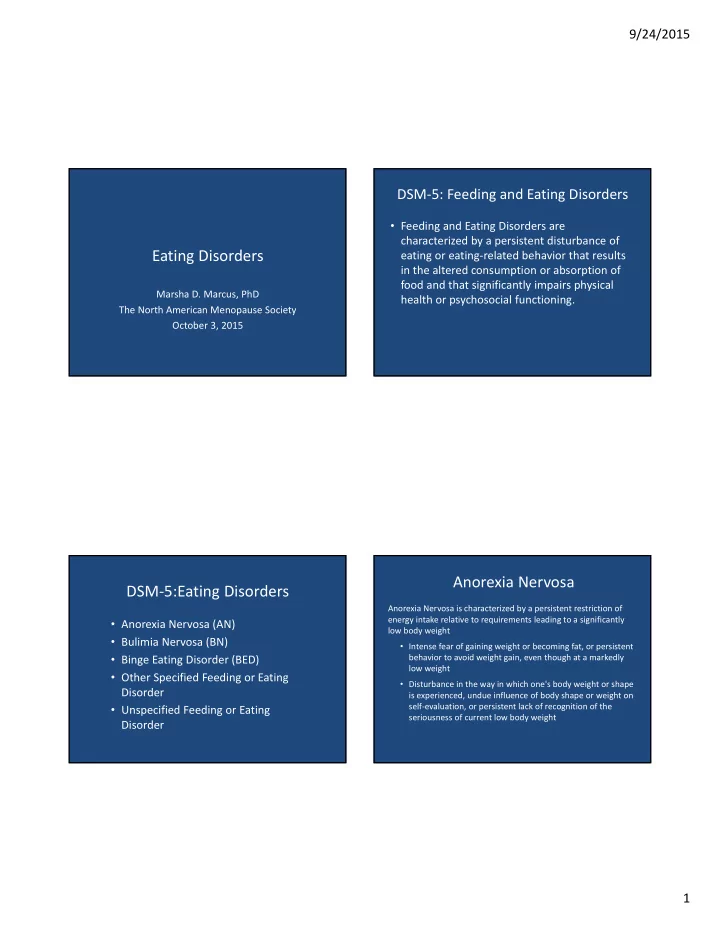
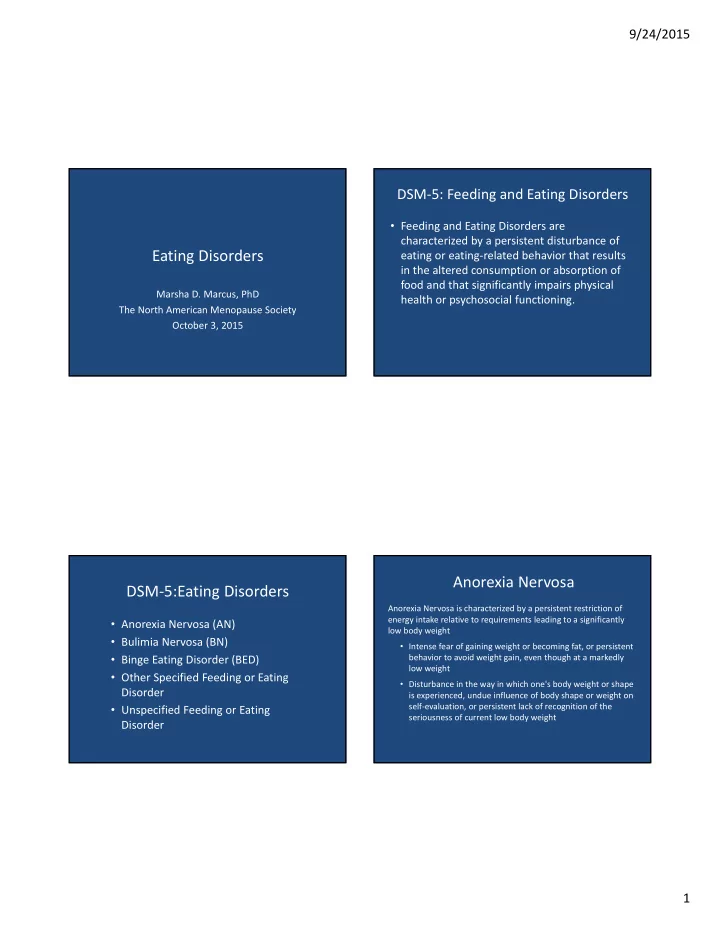
9/24/2015 DSM ‐ 5: Feeding and Eating Disorders • Feeding and Eating Disorders are characterized by a persistent disturbance of Eating Disorders eating or eating ‐ related behavior that results in the altered consumption or absorption of food and that significantly impairs physical Marsha D. Marcus, PhD health or psychosocial functioning. The North American Menopause Society October 3, 2015 Anorexia Nervosa DSM ‐ 5:Eating Disorders Anorexia Nervosa is characterized by a persistent restriction of energy intake relative to requirements leading to a significantly • Anorexia Nervosa (AN) low body weight • Bulimia Nervosa (BN) • Intense fear of gaining weight or becoming fat, or persistent behavior to avoid weight gain, even though at a markedly • Binge Eating Disorder (BED) low weight • Other Specified Feeding or Eating • Disturbance in the way in which one's body weight or shape Disorder is experienced, undue influence of body shape or weight on self ‐ evaluation, or persistent lack of recognition of the • Unspecified Feeding or Eating seriousness of current low body weight Disorder 1
9/24/2015 Binge ‐ Eating Disorder Bulimia Nervosa Binge eating disorder (BED), like BN, is characterized by recurrent episodes of Bulimia Nervosa (BN) is characterized by recurrent, persistent episodes of binge eating, but without regular the compensatory behaviors in BN binge eating, which have two critical features: • Eating, in a discrete period of time (e.g., within any 2 ‐ hour period), The binge ‐ eating episodes are associated with three (or more) of the an amount of food that is definitely larger than what most following clinical correlates : individuals would eat in a similar period of time under similar circumstances • Eating much more rapidly than normal • A sense of lack of control over eating during the episode (e.g., a • Eating until feeling uncomfortably full feeling that one cannot stop eating or control what or how much one • Eating large amounts of food when not feeling physically hungry is eating) • Eating alone because of being embarrassed by how much one is eating • Feeling disgusted with oneself, depressed, or very guilty after There are recurrent inappropriate compensatory behaviors to prevent overeating weight gain, such as self ‐ induced vomiting; misuse of laxatives, diuretics, or other medications, fasting; or excessive exercise Marked distress regarding binge eating is present Self evaluation is unduly influenced by body shape and weight Subjective Binge Eating Eating Disorders Symptomatology • Symptoms of eating disorders are common in • The amount eating in binge episodes is highly the general population and also are associated variable with distress and dysfunction – Many episodes consist of a small or moderate Restrictive dieting • number of calories Driven exercise • • Subjective binge episodes (SBEs): Purging behaviors • – Eating an amount of food that is perceived by the Binge eating • individual to be large, but is not definitely larger Over ‐ concern with shape and weight • than most others would eat Body dissatisfaction • – An associated sense of loss of control 2
9/24/2015 Psychiatric Co ‐ morbidity Associated with “Any Lifetime Prevalence of DSM ‐ IV Eating Disorders* Binge Eating”* Males (%) Females Total (%) % Odds Ratio (%) Any anxiety disorder 59.5 3.7 Anorexia nervosa .3 .9 .6 Any mood disorder 44 3.0 Bulimia nervosa .5 1.5 1.0 Any impulse control 40.2 2.2 Binge eating disorder 2.0 3.5 2.8 disorder Sub ‐ threshold binge 1.9 .6 1.2 Any substance use 28.7 2.8 eating disorder disorder Any binge eating 4.0 4.9 4.5 Any disorder 76.5 3.7 *Hudson, Hiripi, Pope, Kessler, 2007 * Hudson, Hiripi, Pope, Kessler 2007 BMI Distribution for BN and BED Eating Disorders and Mid ‐ Life Women BMI Distribution 12 ‐ Month BN (%) 12 ‐ Month BED (%) No Disorder (%) • Disordered eating in mid ‐ life may represent: < 18.5 (underweight) ‐ ‐ 2.0 – Persistent or chronic disorder 18.5 ‐ 24.9 (normal) 15.3 19.0 36.7 – Recurrence or exacerbation 25 ‐ 29.9 (overweight 42.2 35.7 36.2 30 ‐ 34.9 (class I) 3.5 25.6 15.1 – New onset disorder 35 ‐ 39.9 (Class II) 20.3 3.6 6.2 40+ (class III) 18.7 16.2 3.8 30+ (total obese) 42.4 45.4 25.1 3
9/24/2015 Increased Admissions among Mid ‐ Life Women Percent of women 40 years or older admitted for inpatient eating disorders treatment by year of admission (Ackard et al., J Psychosomatic Res, 2013) Eating Disorder Diagnoses Vary by Age Disordered Eating in Mid ‐ Life Group (18 ‐ 24 years vs. 40+ years)* • The estimated point prevalence for eating disorders in mid ‐ life is 4.6%* • More than 10% of women older than 50 years endorse symptoms of eating disorders • Older and younger women report high levels of body dissatisfaction (40 ‐ 80%) *Elran ‐ Barak et al., J Nervous Mental Dis, 2015. *Mangweth ‐ Matzek et al., IJED, 2014; 4
9/24/2015 Is the Menopausal Transition a Reasons for Body Dissatisfaction in “Window of Vulnerability”? Mid ‐ Life – Biological – Menopausal status, Body Mass Index • Investigators examined the relation between menopausal status and eating disorders and – Psychological – Negative affect, importance of appearance, aging anxiety associated pathology in 436 community – Sociocultural – Role transition, history of adversity women – Peri ‐ menopausal women had a markedly higher prevalence of eating disorders than pre ‐ menopausal women – Peri ‐ menopausal women also reported higher levels of body image concerns *Mangweth ‐ Matzek et al., Int J Eat Disorders, 2013 Disordered Eating as a Function of Implications for Clinicians Menopausal Status Pre – MP (N=192) Peri – MP (N=110) Post – MP (N=134) • Screening N (%) • Referral Eating Disorders 4 (2)* 10 (9)* 7 (5) AN 0 0 0 • Treatment BN 2 2 3 BED 1 4 2 Unspecified ED 1 4 2 Sub ‐ Threshold EDs 7 (4) 7 (6) 7 (5) Binge Eating 5 5 3 Purging Ov/Ob 2 2 4 5
9/24/2015 Eating Disorder Screen for Primary Care* • Are you satisfied with your eating patterns? • Do you ever eat in secret? • Does your weight affect the way you feel about yourself? • Have any members of your family suffered with an eating disorder? • Do you currently suffer or have you ever suffered in the past from an eating disorder? Cotton M et al., J Gen Intern Med, 2003 Pharmacotherapy of BN & BED Psychotherapy for Eating Disorders • Pharmacotherapy • Weight restoration is the cornerstone of – There is no clearly efficacious medication for AN treatment of AN – Antidepressant treatment moderately effective in the – Specialty ‐ care referral is indicated treatment of BN and BED • Strongest evidence for SSRIs • Psychosocial treatment is effective in treatment of BN and BED • FDA ‐ Approved treatment – Cognitive behavior therapy – BN ‐ Fluoxetine (60 mg/day) – BED ‐ Lisdexamfetamine dimesylate (50 ‐ 70 mg/day) – Interpersonal therapy – Dialectical behavior therapy • Dearth of long ‐ term outcome data 6
9/24/2015 Summary • Eating disorders and associated symptoms are common in mid ‐ life women – Query patients about weight ‐ related and eating behavior concerns – Consider depressive symptoms and other psychiatric co ‐ morbidity – Discuss referral to mental health provider 7
Recommend
More recommend