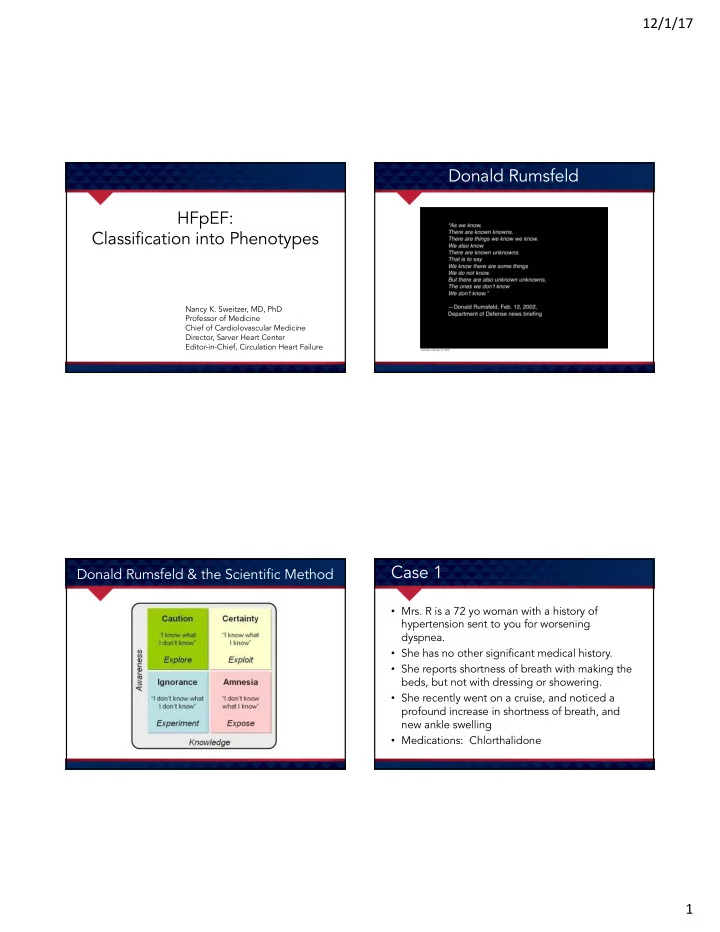
12/1/17 Donald Rumsfeld HFpEF: Classification into Phenotypes Nancy K. Sweitzer, MD, PhD Professor of Medicine Chief of Cardiolovascular Medicine Director, Sarver Heart Center Editor-in-Chief, Circulation Heart Failure Case 1 Donald Rumsfeld & the Scientific Method • Mrs. R is a 72 yo woman with a history of hypertension sent to you for worsening dyspnea. • She has no other significant medical history. • She reports shortness of breath with making the beds, but not with dressing or showering. • She recently went on a cruise, and noticed a profound increase in shortness of breath, and new ankle swelling • Medications: Chlorthalidone 1
12/1/17 Mrs. R Mrs. R • Weight: 115 pounds • Echo: • HR 72 bpm, BP 152/78 – EF 72%, no RWMA • JVP 14 cm H2O – LV thickness 13 mm • Chest clear – LA size: moderately enlarged – PA pressures estimated at 50 mmHg • Nl PMI, regular, nl S1, physiologic splitting – Mild MR, mild TR of S2, no audible murmur, +S4 – RV size and function normal • Enlarged liver, + HJR • Cath: No CAD • 1+ edema bilaterally to mid-shin, nl cap refill, warm Case 2 Mr. B • Weight 225 (height 5’7”) • Mr. B is a 62 yo man with exertional dyspnea • HR 96, BP 122/78 • Oxygen-dependent COPD • JVP 6 • Obesity hypoventilation syndrome • Chest clear without rales • Sleep apnea treated with CPAP • PMI not palpable, distant heart tones, but no • Referred by his pulmonologist obvious murmur or gallop • Liver span normal, no HJR, no edema • Echo with normal LV, E/A 0.8, e’ 8, E/e’ 8, RVH 2
12/1/17 Mr. B, RHC Overview • Definitions, Epidemiology • RA 4, PA 55/20, CWP 12 • Diastolic Dysfunction and HFpEF • Bicycle exercise on the cath lab table • Mechanistic Insights – RA 6, PA 98/45, CWP 32 • Improving Diagnostic Precision Epidemiology HFpEF: Definition • Clinical Definition: – A patient with the clinical syndrome of heart failure, normal left ventricular ejection fraction, and no other etiology of the symptoms, is said to have “heart failure with preserved ejection fraction” or HFpEF. – Historically called diastolic heart failure based on the supposition that if contraction is normal, then relaxation must be abnormal. • Pathophysiological Definition: Filling of the LV to normal end diastolic volume to produce normal cardiac output occurs only at higher than normal pressures under some conditions. Owan et al, NEJM 2006; 355:251-9. 3
12/1/17 Mechanisms of HFpEF Ca Causes of HF HFpEF •Diastolic dysfunction •Impaired left ventricular relaxation •Myocardial ischemia •Hypertrophy, including aortic stenosis, hypertension, hypertrophic cardiomyopathy •Systolic dysfunction •Diabetes mellitus •Aging •Increased myocardial stiffness •Infiltrative disorders (amyloidosis, sarcoidosis, hemochromatosis) •Endomyocardial fibrosis •Ventricular interaction or pericardial restraint •Right Ventricular pressure or volume overload •Acute pulmonary embolism •Acute mitral regurgitation or tricuspid regurgitation •Pericardial disease •Abbreviated left ventricular filling time •Atrial tachyarrhythmias, especially atrial fibrillation •Moderate sinus tachycardia with LBBB •Multifactorial •High output heart failure (thyrotoxicosis, arteriovenous fistula, pheochromocytoma) •Renal dysfunction •Volume overload states •Obesity Diastolic Dysfunction Diastolic Dysfunction R ELAXATION Left ventricle E LASTIC R ECOIL P ASSIVE E LASTICITY Left ventricle Impaired relaxation Increased stiffness Left atrium Left atrium Left atrium Left atrium Rapi Ra pid d At Atrial al IVRT IV Diastasis Di Fi Filling ng Fi Filling ng Rapi Ra pid d At Atrial al Diastasis Di IV IVRT Diastole is divided into 4 phases Filling Fi ng Fi Filling ng 4
12/1/17 Diastolic Function Assessment Diastolic Dysfunction is not HFpEF Redfield et al, JAMA. 2003;289:194-202 Redfield, et al. JAMA. 2003;289:194-202 HFpEF is not Diastolic Dysfunction HFpEF is not Diastolic Dysfunction 100 100 Severe DD 80 80 Moderate DD Mild DD 60 60 Severe DD Normal Moderate DD Indeterminate 40 Mild DD 40 Normal 20 Indeterminate 20 0 0 Control Hypertensive HFpEF Enrolled Patients: CHARM - Preserved LVH Melenovsky et al, 2007; 49:198-207 Persson et al JACC 2007; 49:687-94 5
12/1/17 Cardiovascular Stressors Produce Symptoms Diastolic Filling: Effects of Heart Rate in Patients with HFpEF • Exercise • Hypertension • Atrial Arrhythmias • Ischemia • Tachycardia (pneumonia, pain, acute illness) 75 bpm 92 bpm Filling Pressures in HFpEF Exercise Responses in HFpEF Failure of the Frank-Starling Relationship 70 35 Control 60 HFpEF 30 Pulmonary Capillary Wedge Peak 50 25 exercise Pressure (mmHg) 40 20 RV systolic pressure 30 15 Estimated PAD 20 10 Peak Rest exercise 5 10 0 0 120 140 160 60 80 100 DHF-Rest DHF-24 hour Left Ventricular End-Diastolic Volume (ml) Kitzman et al, JACC 1991 Zile et al., 2008, Journal Card Failure. 14: 816-23. 6
12/1/17 Mechanisms of HFpEF: HFpEF Physiology Abnormal Ventricular Stiffness • Traditionally attributed to changes in extracellular matrix, including: – Increased collagen deposition – Interstitial fibrosis • Recent studies suggest much of this is attributable to altered phosphorylation and increased stiffness of titin Pressure Volume Kawaguchi et al, Circ 2003;107:714-20. Mechanisms of HFpEF: Mechanisms of HFpEF: RAAS System Activation Abnormal Contractility • Angiotensin and aldosterone are pro- fibrotic in both the heart and blood vessels, increasing stiffness. • Hypertrophied hearts have increased ACE in the myocardium, leading to locally high angiotensin II levels. • Trials of angiotensin system blockade in diastolic HF have been disappointing. • CHARM, PEP-CHF, I-PRESERVE 7
12/1/17 Systolic Function in HFpEF Systolic Function in HFpEF 100 90 80 70 Ejection Fraction 60 50 Dobutamine Baseline 40 30 20 10 0 Control HFpEF Norman et al, JCardFail 2011; 17:301-8 Norman et al, JCardFail 2011; 17:301-8 Mechanisms of HFpEF: Systolic Dysfunction in HFpEF Abnormal Contractility • During times of increased demand, such as exercise, the ventricles of these patients seem unable to increase output. “Impaired contractile reserve” Shah AM et al, Circ 2015; 32:402-414. 8
12/1/17 Mechanisms of HFpEF: Physiology of Arteries Arterial Stiffening and Altered Ventricular-Vascular Interaction • Compliance or cushioning function – To transform pulsatile into continuous flow • Conduit function – Deliver an adequate supply of blood to body tissues – Maintain adequate mean arterial pressure • Minimize energy losses Mechanisms of HFpEF: Arterial Hemodynamics in Humans Arterial Stiffening and Altered Ventricular-Vascular Interaction • Unique Nature of Humans: • Altered wave travel in the arteries leads to – We are upright animals altered load on the ventricle. – Proximal aorta interacts directly with heart • Wave travel in the aorta is altered by – Short arteriolar beds exist between aorta and arterial stiffening. organs without much autoregulation (brain • This impacts ventricular systolic and and kidney) diastolic function. • Wave reflection is extremely important (after age 17) • Non-invasive assessment is useful 9
12/1/17 Wave Travel in Arteries Reflected Pressure Waves Reflected Pressure Waves Reflected Pressure Waves With aging, and nearly all identified cardiovascular risk factors, pulse wave velocity and amplification increase 10
12/1/17 Coupling of the LV to the Circulation Ventricular Performance Ventricular Vascular Coupling • If we reduce reflected waves, can we increase stroke volume • If we reduce reflected waves, can we improve ventricular relaxation Ø During a normal contraction, at peak force, there is little calcium left in the myocyte. Ø New crossbridges cannot be formed. 11
12/1/17 What Happened? Reduction of Augmentation 160 Va Variable Baseline Ba BN BNP p p value ue 140 Augmentation Index, % 11.4 ± 8.9 -0.2 ± 14.7 0.02 ∆ P Pressure (mmHg) es 120 E’ velocity 10.0 ± 2.5 8.8 ± 2.0 0.06 100 Stroke volume, mL 68.5 ± 18.3 60.9 ± 8.1 0.02 80 Ees 60 40 20 ∆ P ed 0 10 30 50 70 90 110 130 150 Volume (mL) 1. Theoretical pressure volume loops generated using mean data from the study population for central arterial pressure, Sweitzer NK et al, Am J Hypertens 2013; 26:866-71 Sweitzer NK et al, Am J Hypertens 2013; 26:866-71 HFpEF: Treatment NEAT Trial A Average Daily Accelerometer Units B Hours of Activity per Day C Average Daily Accelerometer Units in 120-mg Dose Phase in 120-mg Dose Phase in Three Dose Phases Combined 10,000 10.0 10,000 9,000 9.0 9,000 8,000 8.0 8,000 No. of Hours No. of Units No. of Units 7,000 7.0 7,000 6,000 6.0 6,000 5,000 5.0 5,000 0 0 0 − 500 − 0.5 − 500 P=0.06 P=0.02 P=0.02 − 1000 − 1.0 − 1000 Isosorbide Treatment Isosorbide Treatment Isosorbide Treatment Placebo Mononitrate Difference Placebo Mononitrate Difference Placebo Mononitrate Difference Figure 1. Primary and Secondary End Points for Activity Levels. Redfield MM et al, NEJM 2015; 373:2314-24 12
Recommend
More recommend