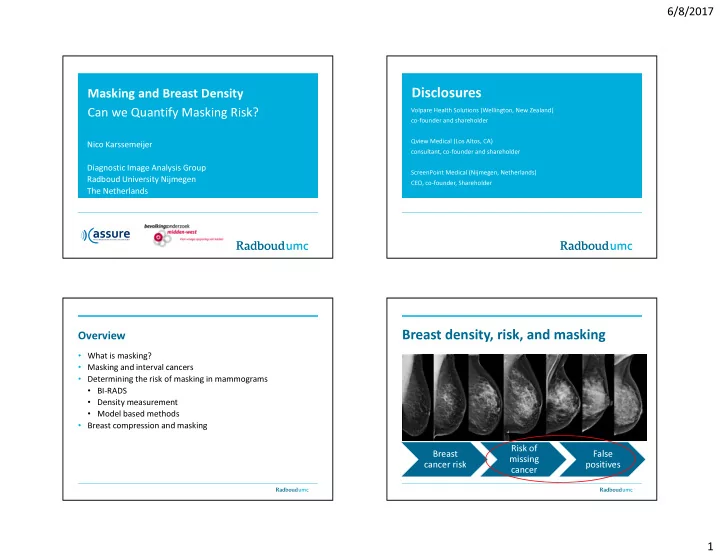
6/8/2017 Disclosures Masking and Breast Density Volpare Health Solutions (Wellington, New Zealand) Can we Quantify Masking Risk? co-founder and shareholder Qview Medical (Los Altos, CA) Nico Karssemeijer consultant, co-founder and shareholder Diagnostic Image Analysis Group ScreenPoint Medical (Nijmegen, Netherlands) Radboud University Nijmegen CEO, co-founder, Shareholder The Netherlands Breast density, risk, and masking Overview • What is masking? • Masking and interval cancers • Determining the risk of masking in mammograms • BI-RADS • Density measurement • Model based methods • Breast compression and masking Risk of Breast False missing cancer risk positives cancer 1
6/8/2017 Breast density and screening sensitivity in the Netherlands Population based screening program – Age group 50-74 – Two year interval - Digital Mammography Total VDG 1 % VDG2 % VDG3 % VDG 4 % N 111898 24,210 21.6 46,426 41.5 32,330 28.9 8932 8.0 Screen- detected 667 96 298 212 61 Interval 234 16 86 93 39 FP 1774 271 700 590 213 TN 109,223 23,827 45,324 32,279 8912 Breast density and screening sensitivity in Breast density and screening sensitivity in the Netherlands the Netherlands – Only invasive cancers Total VDG 1 VDG2 VDG3 VDG 4 Total VDG 1 VDG2 VDG3 VDG 4 Recall/1000 20.6 14.3 20.5 23.3 28.5 Recall / 1000 21.8 15.2 21.7 24.8 30.7 FP/1000 15.9 11.2 15.1 18.3 23.9 FP / 1000 15.9 11.4 15.1 18.2 23.8 Screen-detected / Screen-det /1000 4.7 3.1 5.4 5.0 4.6 1000 5.9 4.0 6.4 6.6 6.8 Interval/1000 2.1 0.6 1.8 2.8 4.4 Interval / 1000 2.1 0.7 1.9 2.9 4.4 BC/1000 6.9 3.7 7.2 7.9 9.0 BC / 1000 8.1 4.6 8.3 9.4 11.2 Sensitivity 83.3% 74.5% 62.9% 50.6% 69.1% Sensitivity 85.7% 77.6% 69.5% 61.0% 74,0% Specificity 98,4% 98.9% 98.5% 98.2% 97.6% Specificity 98.4% 98.9% 98.5% 98.2% 97.6% PPV 27,3% 26.2% 29.9% 26.4% 22.3% PPV 23.0% 21.7% 26.9% 21.6% 16.1% 2
6/8/2017 Sensitivity for invasive cancer in age groups 831,455 exams Comparison Wanders et. al. (top) and Kerlikowske et. al. (bottom) Volpara VDG 1 VDG2 VDG3 VDG 4 Distribution % 21.6 41.5 28.9 8.0 Sensitivity % (invasive) 83.3 74.5 62.9 50.6 Specificity % 98.9 98.5 98.2 97.6 BI-RADS 1 2 3 4 Distribution % 11.7 40.8 39.4 8.1 Sensitivity % 81.2 84.3 68.9 63.3 (invasive) 94.4 90.2 88.0 90.8 Specificity % 3
6/8/2017 4
6/8/2017 5
6/8/2017 6
6/8/2017 Cancers may be hidden in dense tissue. Can we quantify masking risk ? X-ray attenuation of cancers and dense tissue is about • BI-RADS the same. • Automated density assessment • Volumetric • 2D Compression paddle • Use a model to predict masking • Analytic • Machine learning • Observer models • Evaluate methods by measuring how well they can determine Detector / Imager interval cancer risk Also if not ‘inside’ dense tissue a cancer may be masked. It that case the other view (CC or MLO) may In this case the cancer will not be masked in any view help. Compression paddle Compression paddle Detector / Imager Detector / Imager 7
6/8/2017 Texture plays a role. If a cancer looks like other patches If an overlapping layer of dense tissue it thin the of dense tissue it will be hard to detect (priors may cancer may well be visible help) Compression paddle Compression paddle Detector / Imager Detector / Imager Masking risk quantification Calcifications are not masked. Their X-ray attenuation (Katharina Holland, Radboud Nijmegen) is much larger. • PDA : Percentage dense area • VGT : Volume of glandular tissue • PDV : Percentage dense volume Compression paddle • PA1 : Percent area with dense tissue thickness > 1cm • DTMM: Detectability model based on volumetric density maps Detector / Imager 8
6/8/2017 Volumetric Density Maps The simplest model • VGT : Volume of glandular tissue ( , ) d x y dxdy ∫ breast area • PDV : Percentage dense volume = VGT / breast volume 1 1 P. R. Snoeren and N. Karssemeijer (2004) IEEE Trans Med Replace dense tissue thickness with PA1: Aassume that a lesion is detectable when dense ‘masking’ measure tissue layer is less than 1 cm thick. • M(x,y) = 0 : no risk of a masked cancer at that location • M(x,y) = 1 : Cancers always masked Compression paddle ( , ) m x y dxdy ∫ breast area Detectable Not detectable Detector / Imager 9
6/8/2017 Use tumor size distribution Masking measure m(x,y) depends on dense tissue thickness and lesion size H 1.2 1.2 1 1 50 0.8 0.8 m 0.6 m 40 0.6 0.4 0.4 30 0.2 0.2 20 0 0 0 10 20 30 40 10 0 0.5 1 d (mm) d/H 0 step function sigmoid at 1 cm 0.25 H 0.5 H 0 5 10 15 20 25 30 35 40 45 50 sigmoid at 2 cm Effective diameter distribution screen detected cancers (mm) Normalization Lesion location distribution Avoid that large breasts have a higher masking risk than small breasts • Normalization with the breast area • Normalization with a cancer location probability distribution (CLPD) p(x,y) ( , ) ( , ) p x y m x y dxdy ∫ × 10
6/8/2017 Evaluation Effect of normalization Images for the Dutch breast cancer screening program • 2003-2011 complete cancer status • > 200.000 exams of > 60.000 women • 93 interval cancers diagnosed within 12 months from screening • 930 randomly selected controls • average results of the left and right MLO image Comparison of the methods • Study Material: Last negative screening mammogram of 111 interval cancers (within 12 months) and 1110 normal mammograms • Masking measures: • VDG - Volumetric Density (Volpara) • PDA - Percent Area with dense tissue thickness > 1 cm • DTMM - Mathematical Masking Model • BI-RADS 11
6/8/2017 Evaluation of Masking Measures Can we do better? Potential reduction of interval cancers by supplemental screening • Context (texture) should be included • More complex models that take into account MLO and CC views • Observer models may be used • Detectability can also be quantified with machine learning Computing lesion detectability • Local noise estimation • Volumetric density map • Assume lesion has Gaussian profile, width 5 mm. • Using model observer to compute detectability 12
6/8/2017 Machine Learning • Use deep learning to recognize patterns that are more likely to hide cancers • Train with patterns extracted from interval cancers and screen- detected cancers Deep learning architecture Experiments - Deep learning architecture: - Dataset: • patches at multiple scales • 109 interval cancers • supervised and unsupervised part • 285 screen detected cancers • output: risk score (for each image) • Raw data • Interval cancers: last screening mammogram before interval cancer occurred (contralateral breast) • Screen detected cancers: contralateral breast - Five fold cross validation - Volpara density grades - Compute odds ratios Michiel Kallenberg et al, University of Copenhagen 13
6/8/2017 Results: Results: VDG 1+2 VDG 3+4 (cancer/control) (cancer/control) Q 3+4 21/38 54/105 VDG 1+2 VDG 3+4 (cancer/control) (cancer/control) Q 1+2 29/127 5/15 Q 3+4 21/38 54/105 Density: OR 1.63 (1.04-2.53) Q 1+2 29/127 5/15 VDG 1+2 VDG 3+4 (cancer/control) (cancer/control) Q 3+4 21/38 54/105 Q 1+2 29/127 5/15 texture: Q 3+4 vs Q 1+2: Deep learning tecturs: OR 2.19 (1.37-3.49) high density/ high texture risk Examples Examples score Low density/ low texture risk score 14
6/8/2017 low density/ high texture Examples Examples risk score low density/ high texture risk high density/ low texture score: risk score textural masking Compression and masking Compression and masking (presented at RSNA 2016) • Breast compression may have a different effect on lesions and Too much compression may reduce visibility of lesions in spot the surrounding breast tissue compressions (Sylvia Heywang-Kohbrunner) • Does compression influence detectability? • Compression pressure can be measured with image analysis “Small lobular carcinomas may disappear with strong compression, so spot views in particular may be misleading in very early lesions.” 15
6/8/2017 Computing the contact surface Measurement of compression • Mean compression pressure is obtained by dividing force by Images from Thesis of Jerry de Groot, University of Amsterdam area of the contact surface Pressure = Force / Contact Area • Contact area is computed by modeling the 3D breast shape and digital image analysis Fig. 2 Force and pressure in two screening Screening performance and pressure centers in NL and US Branderhorst W , de Groot JE , Highnam R , Chan A , Böhm-Vélez M , Broeders MJ Pressure: Very Low Low Medium High Very High den Heeten GJ , Grimbergen CA . European Journal of Radiology 2015 84, 596-602 Total 26,496 26,535 26,634 26,535 26,583 Screen detected 177 162 190 152 152 cancers Interval cancers within 43 58 51 69 73 30 months Interval cancers within 19 15 13 26 37 12 months False positive 486 381 404 426 495 examinations 16
Recommend
More recommend