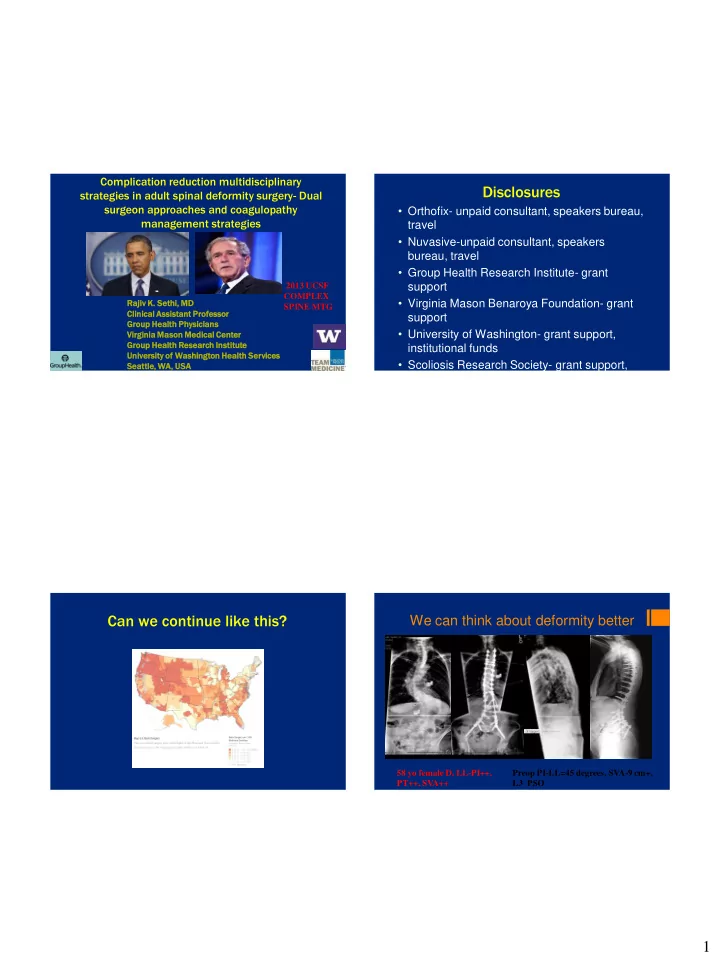
Complication reduction multidisciplinary Disclosures strategies in adult spinal deformity surgery- Dual surgeon approaches and coagulopathy • Orthofix- unpaid consultant, speakers bureau, management strategies travel • Nuvasive-unpaid consultant, speakers bureau, travel • Group Health Research Institute- grant 2013 UCSF support COMPLEX • Virginia Mason Benaroya Foundation- grant Rajiv K. Sethi, MD SPINE MTG Clinical Assi sist stant Prof ofess ssor or support Group Health Physi sicians • University of Washington- grant support, Virginia Mason on Medical Center Group Health Rese search Inst stitute institutional funds Universi sity of Wash shington on Health Services • Scoliosis Research Society- grant support, Seattle, WA, USA travel, committee work Can we continue like this? We can think about deformity better 58 yo female D, LL-PI++, Preop PI-LL=45 degrees, SVA-9 cm+, PT++, SVA++ L3 PSO 1
Fixing iatrogenic problems: PSO of L2 and L4 needed to achieve spinopelvic balance •Major surgical complications 56% - 75% •Unplanned reoperation rates 18 -58% •Unproven benefits regarding improvement of HRQOL Preop PI-LL= 70 degrees, SVA- 24 cm+; Postop PI-LL-3, SVA 3 cm Here is what we know • Risk of pulmonary or cardiac complications is significant • Increased LOS, cost to patient and society, compromised outcomes • Our spine procedures are getting more complex (revision, # levels, age of patient) • Can we minimize the risk of complications with preop or perioperative optimization? 2
We have some honest leaders with us today The Seattle Spine Team Approach to Adult Spinal Deformity and Reduction in Perioperative Complication Rates IMAST 2013 VANCOUVER • Dedicated spine physicians representing mutliple specialties Submitted, Spine Deformity • Working in teams • Standardization of pre, during and post Rajiv K. Sethi, MD phases Group Health Physicians Virginia Mason Medical Center Group Health Research Institute University of Washington Health Services 3
The Seattle Spine Team Our live multidisciplinary Approach preoperative conference 3 arms Screens all adult spinal deformity patients prior to providing full clearance for elective corrective adult • Live preop multidisciplinary deformity surgery This committee consists of orthopaedic spinal surgeons, clearance conference neurosurgeons, spine anesthesiologists, internists, physiatrists and nurses • Two attending surgeons in the OR • Intraoperative protocol for mgmt of coagulopathy Surgical rate for adult scoliosis at three Methods Seattle tertiary spine centers:2008-2012 • Group A (2008-2009) managed without the three pronged approach---NO PROTOCOL • Group B (2010-2011) were managed according to the three pronged approach--- SEATTLE PROTOCOL • Complications and readmissions assessed by an independent research team with both approaches at 30,60 and 90 days Sethi, Wernli, Andersen, UW CHASE 2013, Submitted JAMA 4
Patient Demographics Results NO PROTOCOL GROUP- 40 PATIENTS (2008-2009) COMPLICATION NO PROTOCOL SEATTLE P VALUE PROTOCOL Age Levels Fused Anterior and Posterior Lateral (XLIF) Overall Complication 52 percent 16 percent <0.001 Posterior Alone(TLIF) +Posterior Rate 62 (39-84) 9-15 levels 25 % 75% 0% Wound Infection(%) 12.5 percent 0.8 percent Not significant Return to OR (%) 7.5 percent 1.6 percent <0.001 DVT/PE (%) 10 percent 3.2 percent Not significant PROTOCOL GROUP- 124 PATIENTS (2010-2011) Postop neuro deficit 2.5 percent 0.5 percent Not significant (%) Age Levels Fused Anterior and Posterior Lateral (XLIF)+ Urinary tract 32 percent 9.7 percent <0.001 Posterior Alone(TLIF) Posterior infection (%) 64 (18-84) 9-15 levels 9% 75% 16% D dimer elevation during adult Combined orthopaedic and neurosurgical attending surgeon de novo scoliosis surgery approach to adult spinal deformity surgery: a multi-center and multi-disciplinary perspective . Rajiv K. Sethi hi, , MD 18 Assi sist stan ant Clini nical al Professo essor 16 Group Health Phy hysi sician ans 14 Virginia a Maso son n Medical al Cent nter er 400 12 360 Group Health Resear search h Inst stitute 320 10 D-dimer (mcg/ml) 280 Univer ersi sity of Was ashi hing ngton n 8 240 Seat attle, e, WA, , USA 200 6 160 4 120 SRS LYON 2013 2 80 0 Time after incision (minutes) 13 11 40 Authors: Sethi, Rajiv K.; Qamirani, Erion; 9 7 5 0 3 Theologis, Alexander A.; Leveque, Jean- Patient Number 1 Sethi et al, Coagulopathy in Adult Deformity Surgery…Fibrinogen and D dim Christophe; Ames, Christopher P.; Deviren, SRS/IMAST 2012, Paper #9, Submitted, J SpInal Dis Tech Vedat 5
Neurosurgery and Orthopaedics meet together at the spine • Cardiac surgery position statement recommends two surgeons • “A minimum of two qualified cardiac surgeons is required” • “Complex operating room environment” requires teams http://www.facs.org/fellows_info/guidelines/cardiac.html 6
Methods Methods • 312 consecutive cases with an attending • All cases were major adult deformity cases neurosurgeon and orthopaedic surgeon from with 9-15 levels fused two tertiary spinal deformity centers in Seattle • Three column osteotomies, MIS lateral and San Francisco approaches and traditional anterior • Retrospective review of all cases approaches represented at both centers • 30 and 90 day readmission rates • Two attending surgeons involved in all cases even though fellows or residents may participate Complications assessed Results • Wound infections requiring reoperation • Hardware failure requiring reoperation • Pneumonia • Urinary tract infection (UTI) • Stroke • Thromboembolic events (deep venous thrombosis and/or pulmonary embolism) • Iatrogenic neurological injury • Death. 7
Results Results • Similar downward trend in complications Complication 30 day 90 day Wound Infection 4% 6.4% assessed at both centers CVA 0.64% 0.64% • Overall complication rates- 18 percent at 30 DVT/PE 2.2% 2.2% days Return to OR for hardware 1.6% 3.5% modification • Overall complication rates- 23 percent at 90 Death 0.3% 0.3% days Pneumonia 1.9% 1.9% UTI 3.8% 4.9% Coagulopathy in adult de novo scoliosis surgery: Timing and onset of breakdown of the coagulation cascade as measured by D dimer and Conclusions fibrinogen levels Rajiv K. Sethi MD , Ryan Pong MD ;JC Leveque MD ; Thomas Dean MD; Stephen Olivar MD, Sarah Hipps MD, Vishal Gala MD ; Chong Lee MD PhD ; Kyle Kim MD PhD • A combined orthopaedic and neurosurgical Virginia Mason Medical Center and Group Health Physicians Departments of Neurosurgery attending approach to adult spinal deformity and Anesthesia, Seattle, WA surgery can enhance patient safety and substantially reduce perioperative complication Whitecloud Clinical Research Award Nominee, IMAST, rates by approximately 50% compared to current Istanbul 2012; Submitted J Spi Dis Tech rates. • This is the first report detailing this approach at two spinal deformity centers. 8
Do we understand the Intraoperative protocol shouldn’t be subject to the whim of the anesthesiologist of the day problem? • Hourly measurements, EBL, Hct, INR, Plt, • Most surgeons use PT-INR or the appearance of the wound as a Fibrinogen, D dimer surrogate for the status of the coagulation cascade during adult spinal deformity surgery • Same surgeons and anesthesiologists (complex • Anesthesia asks “How does it look down there” spine team) • A better tool is needed to track coagulopathy and to help the team increase patient safety and determine the need for staging, • STANDARDIZED INTRAOPERATIVE etc. MANAGEMENT Methods Inclusion criteria • • Dual attending surgeon as presented at previous IMAST/SRS meetings All adult de novo cases (others excluded) • Complex spine protocol followed in all cases • • Single stage Hourly measurements, EBL, Hct, INR, Plt, Fibrinogen, D dimer • 13 consecutive cases in the study period meeting criteria • T10-pelvis pedicle screw • fixation Same surgeons and anesthesiologists (complex spine team) • TLIFS at L4-L5 and L5-S1 • Iliac fixation • Operative steps exactly the same in each case • PSOs, VCRs or staged cases excluded 9
Recommend
More recommend