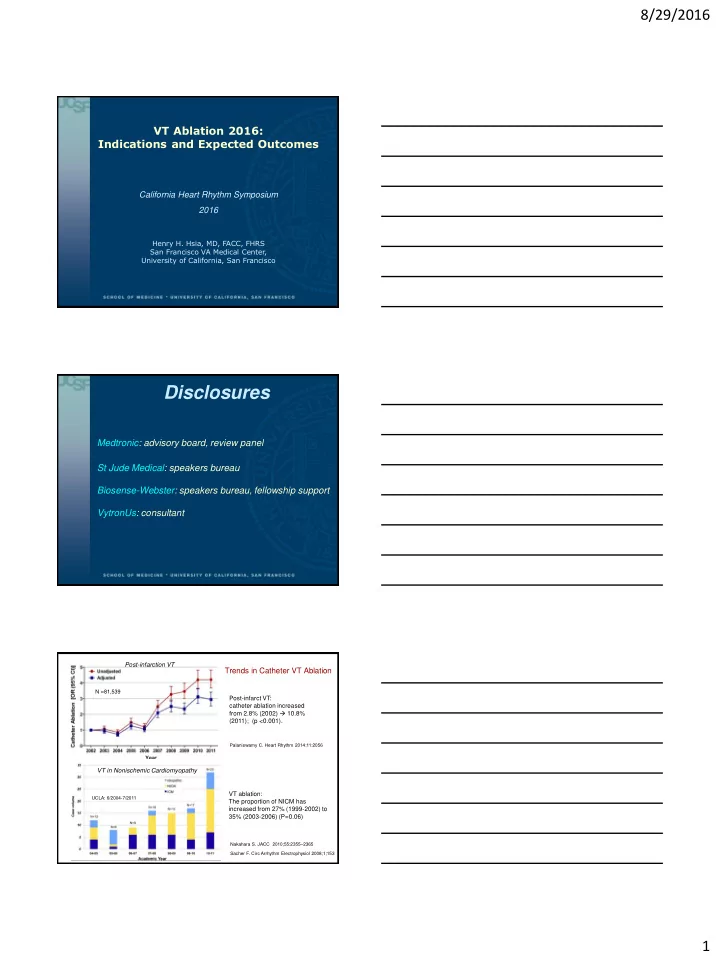
8/29/2016 VT Ablation 2016: Indications and Expected Outcomes California Heart Rhythm Symposium 2016 Henry H. Hsia, MD, FACC, FHRS San Francisco VA Medical Center, University of California, San Francisco Disclosures Medtronic: advisory board, review panel St Jude Medical: speakers bureau Biosense-Webster: speakers bureau, fellowship support VytronUs: consultant Post-infarction VT Trends in Catheter VT Ablation N =81,539 Post-infarct VT: catheter ablation increased from 2.8% (2002) 10.8% (2011); (p <0.001). Palaniswamy C. Heart Rhythm 2014;11:2056 VT in Nonischemic Cardiomyopathy VT ablation: UCLA: 6/2004-7/2011 The proportion of NICM has increased from 27% (1999-2002) to 35% (2003-2006) (P=0.06) Nakahara S. JACC 2010;55:2355 – 2365 Sacher F. Circ Arrhythm Electrophysiol 2008;1;153 1
8/29/2016 Anatomical Substrate Post-Myocardial Slow conduction in the infarcted tissue, Infarction with ‘zigzag' course of activation Tung R. Circulation 2011;123:2284 deBakker J. Circulation 1988; 77:589 deBakker J. Circulation 1993;88;915 RBRS VT: Entrainment with Concealed Fusion Isthmus, #196 Sti-QRS=Egm-QRS 142 msec I II III AVR AVL AVF sti-QRS Egm-QRS 142 ms 142ms V 1 V 2 V 3 V 4 V 5 V 6 Abl d PPI=360 ms VTCL=363 ms Abl p His d His p RV Inferolateral Scar AoV RBRS VT Ent 170 Outer 255 Loop LP 180ms Exit 190 198 Isth Dysynchrony on ICE 2
8/29/2016 Ablation at Isthmus: RBRS VT Termination in 1.5 sec I II III AVR AVL AVF V 1 V 2 V 3 V 4 V 5 V 6 Abl d Abl p His d His p RV Stim 0.5-1.6 mV 0.36-0.55 mV 0.21-0.31 mV I II III AVR AVL AVF V 1 Late potentials with V 2 V 3 decremental local V 4 conduction delay V 5 V 6 Abl d Abl p His RVA I II III aVR aVL Pacemap aVF Spontaneous within the V 1 LBB-RI VT channel V 2 V 3 V 4 V 5 V 6 LP 180 ms LP 171 ms LP 194 ms Decremental LP delay Perfect pacemap 0.21-0.31 mV 0.5-1.6 mV 3
8/29/2016 Kaplan – Meier Estimate of Survival Free from Kaplan-Meier Estimates for Survival ICD (Shock & ATP) Therapy Free from VT or VF Ablation P=0.045 Control P=0.007 Ablation Control SMASH VT Trial VTACH Trial Thermocool VT Ablation Trial N=231, VT (median, 11 in preceding 6 mo), primary end point of freedom from VT after 6 month f/u. VT episodes were reduced from a median of 11.5 to 0 (P<0.0001). Reddy VY. NEJM 2007;357:2657-65. Kuck KH. Lancet 2010; 375: 31 – 40 Stevenson WG. Circ 2008;118:2773-82 Catheter Ablation in Post-infarct VT LVEF Acute Follow-up Recurrent Adverse N Indications (%) success (months) VT/ICD Rx events SMASH-VT Recur/induc 64 31±10 ----- 24 13%* 4.6% (2007) VT/VF ThermoCool 231 MMVT 25 49% 6 47% 7.3% (2008) VTACH 52 Stable VT 34±9.6 ----- 21.9±8.3 53% 3.8% (2010) Euro-VT 63 Recur VT 30±13 81% 12±3 49% 5% (2010) Yokokawa Recur VT 98 27±13 63% 35±23 34% 7.1% (2012) ICD Rx Silberbauer Drug 155 31±9.4 ----- ~19 32% 7% refractory VT (2014) Dinov 164 Recur VT 32±11 77.4% 27 43% 11.1% (2014) VT Recurrences After the Ablation Procedure Thermocool VT Ablation (2008) Yokokawa et al (2012) Success Failure No recurr Recurrent p p (123) (108) VT (65) VT (33) 65 69 LVEF (%) 29 ± 14 25 ± 12 0.26 Age 0.012 (58-70) (62-73) Anterior MI 18 (28%) 14 (42%) 0.14 Heart failure 52% 73% 0.002 Scar area 25 25 69 ± 30 93 ± 40 0.002 LVEF (%) 0.387 (cm 3 ) (20-35) (15-35) # clinical VT 4 ± 5 3 ± 3 0.29 Multiple MI 5% 14% 0.016 Clinical VT VT events in 10 14 359 ± 73 350 ± 77 0.34 0.37 prec 6 mo (4-30) (6-38) CL # induced 3 4 # induced 13 (20%) 9 (27%) 0.41 0.002 VT/pt (2-4) (3-6) VT Longest VT 440 450 Identified 3 ± 2 4 ± 3 0.49 0.251 CL (370-500) (380-538) critical sites Shortest VT 330 305 RF duration 63 ± 44 73 ± 48 0.35 0.029 CL (271-400) (272-350) (min) Total # RF 24 26 Postop VT- 24/63 (38%) 11/32 (34%) 0.72 0.029 nonclinical lesions (11-32) (16-39) Postop VT Postop VT- 0/63 (0%) 0/63 (0%) 1.0 30 58 <0.001 clinical Induction 4
8/29/2016 VT Recurrence Rate vs Ablation Strategies Recurrence Rate During Follow-up 13.4 ± 4 months Complete LP abolition 100 No VT inducible All Patients (n=50) 90 Incomplete LP abolition Percentage of Patients (%) 75% 80 Persistent VT inducibility 70 60 50% 50 40 30 20 12.5% 9.5% 10 0 Silberbauer J et al. Circ Arrhythm Electrophysiol, 2014. 7(3):424-435 Local Abnormal Ventricular Activities 1 2 3 4 (LAVA) 5 Regional Variation of LAVA Latency Freedom from Recurrent VT or Death * Latency of LAVA is affected by locations. Only 3% of septal LAVA were separated from far-field ventricular egm Jais P. Circulation 2012;125:2184 Komatsu Y. Heart Rhythm 2013;10:1630 Ventricular Arrhythmia/ICD Therapy-Free Survival by the Ablation Approach In Post-infarct VT N=92, f/u of 25 ± 10 months N= 160, f/u ~19 months Homogenization (Endo ± Epi): 19% 16% P<0.001 VT non-inducible+LP abolition p=0.006 Endo substrate ablation: 47% VT non-inducible, no LP abolition VT inducible DiBiase L . JACC 2012;60:132 Silberbauer J. Circ Arrhythm Electrophysiol. 2014;7:424 5
8/29/2016 16.4% Scar De-channeling Berruezo A. Circ Arrhythm Electrophysiol . 2015;8:326-336 Recurrence after Catheter Ablation of Post-infarct VT Limited substrate ablation Extensive 38% RRR substrate modification Santangeli et al, Indication for Ablation and Trials, Ventricular Tachycardia Ablation: A Practical Guide, 2014. CardioText Differences Between NICM and ICM Substrates Endo Scar and Endo DS area : ICM >> NICM Endo and Epi LP : ICM >>NICM. LP-targeted ablation was more effective in ICM (82% non-recurrence at 12±10 mon f/u) vs NICM patients with less favorable outcomes (50% at 15±13 mon f/u). 101±55 4.3% 4.1% 56±33 55±41 53±28 1.3% 2.1% Nakahara S. JACC 2010;55:2355 – 2365 6
8/29/2016 Epicardial VT Ablation: A Multicenter Safety Study Characteristics of the Patient Population Ischemic Dilated Other Total ARVC No CMP CMP CMP CMP patients (n=14) (n=17) (n=51) (n=39) (n=13) (n=134) Relative to a control 16% 35% 41% 6% 18% 19% population(n=722) 48 32 9 10 10 109 Sex (Male %) (94%) (82%) (64%) (59%) (77%) (81%) 46 33 9 15 12 115 Prior endocardial ablation (90%) (85%) (64%) (88%) (92%) (86%) Epicardial mapping 42 36 14 12 9 113 and ablation (82%) (92%) (100%) (71%) (69%) (84%) Sacher F. JACC 2010; 55: 2366 Endo Scar area (cm 2 ) Epicardial vs Endocardial Low Epi Voltage Scar Distributions in Non-Ischemic Cardiomyopathy Wide/split/late egm: epicardial (49.7%) controls (2.3%). Soejima K. JACC 2004; 43;10:1834 Cano O. JACC 2009;54:799 – 808 Endo-Epicardial Mapping in Patient with Nonischemic Cardiomyopathy LV endocardium: LV epicardium: minimal scar extensive scar MV MV I II III AVR AVL AVF Entrainment with V 1 concealed fusion: V 2 Isthmus V 3 V 4 V 5 V 6 Abl d Abl p RV 7
8/29/2016 Scar Patterns and Ablation in Nonischemic Cardiomyopathy Basal anteroseptal scar (42%): -aortic root ± anteroseptal endo LV (89%) -anterior cardiac vein (11%), with -RV septum (22%) -epicardium (11%) Green: good pacemap Yellow: ECF White: VT termination Inferolateral scar (47%): -epicardium (63%) -inferolateral endo LV (37%) Piers, S. Circ Arrhythm Electrophysiol. 2013;6:875 Nonischemic Cardiomyopathy: Anteroseptal vs Inferolateral Scar Endocardial unipolar voltage: - Anteroseptal (AS): 44/87 (51%) - Inferolateral (IL): 43/87 (49%) -AS has more extensive endo unipolar scar, freq involves an intramural septal substrate. Epi LPs: common in the IL (81%) vs INFEROLATERAL GROUP AS (4%), p<0.001) and correlated with VT termination sites (p=0.014). VT recurred in 44 patients (51%) during a median f/u 1.5 years. AS scar was associated with higher VT recurrence (74% vs 25%, p<0.001) and redo procedure rates (59% vs 7%, p<0.001). Oloriz, T. Circ Arrhythm Electrophysiol. 2014;7:414-423 Outcome of Catheter Ablation in Nonischemic Cardiomyopathy F/U Acute N Approach No Recurrence Noninducibility (months) Marchlinski 8 10 Endo 1 (12%) 3 (38%) (2000) Hsia 19 22 Endo 8 (42%) 5 (26%) (2003) Soejima Endo (22) 12/22 (55%) 12/22 (55%) 22 11±9 (2004) ± Epi (7) 6/6 (100%) 4/6 (67%) Cano 14/21 (67%) 15/21 (71%) 22 18±7 Endo+Epi (22) (2009) 12/17 (71%) 12/14 (86%) Kuhne Endo (24) 67% if LP+ 24 18 45/67 (67%) (2010) ± Epi (7) 7% if LP- Della Bella Endo+Epi (57) 67 17±18 45/67 (67%) 60.7% (2011) Epi only (10) Tung Endo only (35) 40% 33% 56 12 (2013) Endo+Epi (29) 45% 36% Dinov Endo only (43) 63 20 42 (66.7%) 23% (2014) Endo+Epi (20) 8
Recommend
More recommend