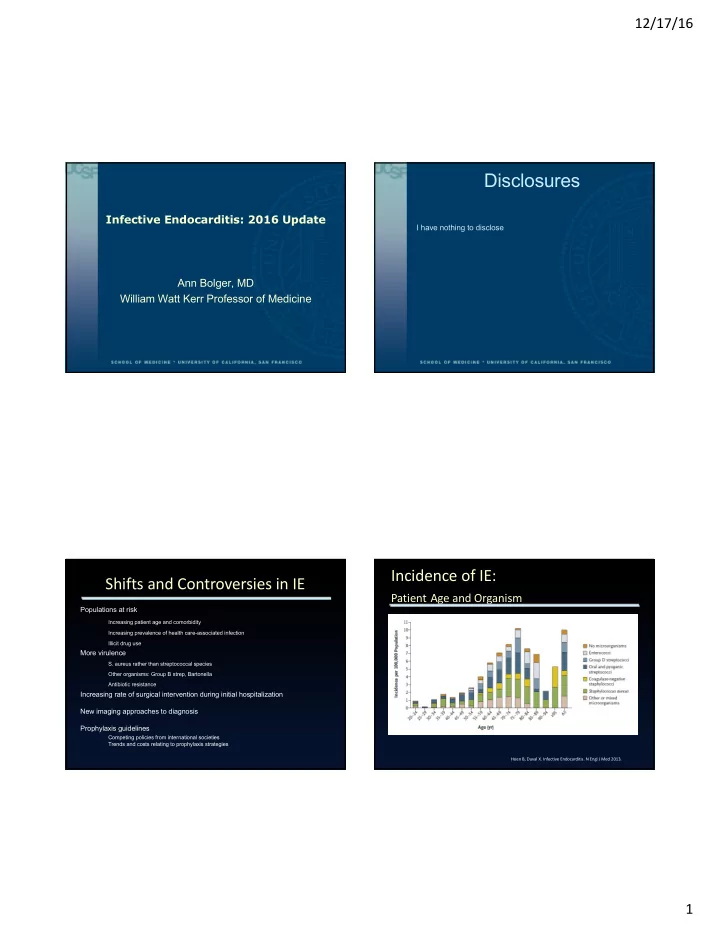
12/17/16 Disclosures Infective Endocarditis: 2016 Update I have nothing to disclose Ann Bolger, MD William Watt Kerr Professor of Medicine Incidence of IE: Shifts and Controversies in IE Patient Age and Organism Populations at risk Increasing patient age and comorbidity Increasing prevalence of health care-associated infection Illicit drug use More virulence S. aureus rather than streptococcal species Other organisms: Group B strep, Bartonella Antibiotic resistance Increasing rate of surgical intervention during initial hospitalization New imaging approaches to diagnosis Prophylaxis guidelines Competing policies from international societies Trends and costs relating to prophylaxis strategies Hoen B, Duval X. Infective Endocarditis. N Engl J Med 2013. 1
12/17/16 Device-related Endocarditis Healthcare-Associated IE Seven-hospital cohort study in Spain 795 consecutive IE cases 16% Health care-associated infection older patients more co-morbid conditions more staphylococcal infections (58% vs 25% in community-acquired infection) Main cause: Vascular access (venous catheter infection in 30%) In-hospital mortality of Healthcare associated infection was 45% (vs 24% in community-acquired, P<0.001) Lomas JM, et al. Healthcare-associated infective endocarditis: an undesirable Bor DH, et al. (2013) Infective Endocarditis in the U.S., effect of healthcare universalization. Clin Microbiol Infect 2010. 1998–2009: A Nationwide Study. PLoS ONE 8(3), 2014 Patient: 57 year old male with ESRD/HD CC: Fatigue and malaise for 6 weeks No dyspnea or fever No intolerance of HD Outpatient workup: Urine culture: S. viridans Blood cultures at dialysis: MSSA Vancomycin begun at HD Sent for outpatient echocardiogram 2
12/17/16 The Burden of IE in Hemodialysis Patients Patient course: No CHF or evidence of embolization Blood cultures negative Rate of IE per 1000 patients Hemodialysis catheter replaced 400,000 patients on RRT in the US in 2009 CT for detection of embolization followed 6-8% increase per year by pulmonary edema; IE is second leading cause of mortality rapid improvement with hemodialysis Incidence 308/100,000 patient-years: Could we have prevented this infection? 50-fold higher than general population How should we manage it? Jones DA, et al. Characteristics and outcomes of dialysis patients with infective endocarditis. Nephron Clin Pract 2013 Werdan K et al. Mechanisms of infective endocarditis: pathogen–host interaction and risk states. Nat Rev Cardiol 2013 3
12/17/16 The Burden of IE in Hemodialysis Patients TAVR vs SAVR: Early endocarditis Mortality approximately 50% (47 - 66%) Mostly Staphylococcal Mostly left-sided Frequent heart failure and embolism Poor prognostic factors Age >60 years Septic emboli MRSA Jones DA, et al. Characteristics and outcomes of dialysis patients with infective endocarditis. Nephron Clin Pract 2013 Amat-Santos IJ et al. Prosthetic valve endocarditis after transcatheter valve replacement JACC: Cardiovascular Interventions 8:2015 UN Office on Drugs and Crime: Time from TAVR or TPVR to Infective World Drugs Report 2012 Endocarditis 230 million people (1 in 20) around the world used illicit drugs in 2011 27 million (0.6%) of the world’s adult population are “problem drug users” Mostly heroin and cocaine dependent Methamphetamine Prescription opiates are expanding rapidly http://www.guardian.co.uk/news/datablog/interactive/2012/jul/02/d Amat-Santos IJ et al. Prosthetic valve endocarditis after transcatheter rug-use-map-world valve replacement JACC: Cardiovascular Interventions 8:2015 4
12/17/16 Heroin in Brown, Black and White Influence of Drug of Choice on IE Characteristics Heroin source dictates distribution, and type predicts practice Retrospective cohort of 247 cases of IE Colombia Eastern US Mexico Western US 74% cases in IDU, most with heroin Southeast Asia Au s tralia and Canada Afghanistan/Pakistan Europe S. aureus IE was most prevalent and more likely to occur in IDUs versus non-IDUs (OR Black tar heroin (Mexico): 5.5, p<0.0001). Heavier, distributed by land. Vaporizable but acidic and irritating. Requires heat to dissolve. Tricuspid valve (TV) IE was more likely to More venous scarring; SQ or IM routes have lower HIV transmission. occur in IDUs (OR 4.37, p=0.001) More soft tissue infections, botulism and clostridial infections. Heroin use may underlie the TV IE occurred more frequently in heroin association between IDU and White heroin (Southeast Asia): users vs. IDUs not using heroin (OR 4.03, right-sided endocarditis. Lighter, water soluble and vaporizable. p=0.033) HIV prevalence higher with powder heroin. Ciccarone D. Heroin in brown, black and white: Structural factors and medical Jain V et al. Infective endocarditis in an urban medical center: association consequences in the US heroin market. International Journal of Drug Policy 2009 (20). of individual drugs with valvular involvement. J Infect (57) 2008 The next controversy? IE prevention in the current context French population-based surveys in 1991, 1999, 2008 Chirouze C, et al. Infective endocarditis prophylaxis: moving from dental prophylaxis to global prevention? Eur J Clin Microbiol Infect Dis 2012 5
12/17/16 Predictors of Operative Mortality Society of Thoracic Surgeons (STS) Adult Cardiac Surgery Database, 2002 through 2008 19,543 IE operations Operative mortality: 8.2% Nearly half of patients did not have active IE at the time of surgery Independent predictors of mortality: Urgency of surgery Hemodynamic status Renal failure Active infection Multiple valve involvement Diabetes mellitus Arrhythmia Previous cardiac surgery Gaca JG, et al. Outcomes for endocarditis surgery in North America: a simplified risk scoring system. J Thorac Cardiovasc Surg 2011 Impact of Early Surgery on Mortality Stroke in Endocarditis (International Collaboration of Endocarditis) Heart failure Conventional surgical indications: Intracardiac abscess Embolic events Stroke occurs in Left-sided IE in 20-40% Severe valvular regurgitation Failure of antibiotic therapy 5% are intracranial hemorrhage Prospective cohort study of 1552 patients with native valve IE Mycotic aneurysm forms in 2-4% of patients with IE Surgery in 46% during index hospitalization 50% resolve with therapy In-hospital mortality of early surgery vs medical therapy: Mortality in un-ruptured is 30%, ruptured 80% 12.1% vs 20.7% (P<0.001) Absolute risk reduction: -5.9% ( after propensity-based matching and adjustment for survivor bias) 95% are embolic In-hospital mortality (%) 70% of emboli occur in the first 15 days after diagnosis No surgery Surgery Mortality 58% Asymptomatic emboli can be detected in 30% of aortic or mitral IE Quintile of surgical likelihood Lalani T, et al. Analysis of the impact of early surgery on in-hospital mortality of native valve endocarditis: use of propensity score and instrumental variable methods to adjust for treatment selection bias. Circulation, 2010 6
12/17/16 Influence of Stroke on Surgical Timing Current Guidelines: Stroke and Surgery for Endocarditis Risk of neurological deterioration in case of symptomatic brain infarction (small, retrospective series) < 4 days: 20% 4-14 days: 20–50% 15-28 days: <10% >28 days: <1% Conclusion: Surgery should be considered within the first 72 h if a patient with stroke has severe CHF, otherwise after 4 wks Angstworm K, et al. J Neuro 2004 Multicenter prospective study of 496 consecutive IE patients Cerebrovascular complications in 22% of patients Neurological exacerbation in 6.3% (only in patients with symptomatic CVA) No excess surgical mortality with silent CVC or TIA Conclusion: Safe to proceed to valve replacement despite transient ischemic attacks or ‘‘silent’’ cerebral embolism Thuny F, et al. Eur Heart J 2007 Amat-Santos IJ et al. Prosthetic valve endocarditis after transcatheter valve replacement JACC: Cardiovascular Interventions 8:2015 Beyond Echo: Imaging in IE Stroke and Surgery for Endocarditis in TAVR CT Cerebral “Timing of surgery in patients with symptomatic ischemic stroke should be a All patients at admission to detect balance of the severity of cardia decompensation and pathology and the severity cerebral infarction, hemorrhage, aneurysms of the neurological symptoms. Abdominal Uncontrolled infection or difficult situations, to detect visceral infarction, abscess or aneurysm Patients with severe cardiac decompensation and severe mechanical cardiac MRI lesions should be operated on emergently or urgently unless the neurological status (eg coma, large intracranial hemorrhage) precludes heparinization or Cerebral Better sensitivity for small cerebral infarctions and when neurological recovery to reasonable quality of life is very unlikely (eg, hemorrhages without radiation or contrast multiple strokes or severe neurological deficits in patients with preexisting Angiography comorbidities. Cerebral In patients with hemorrhage, suspicion of aneurysm with For patients with IE and parenchymal hemorrhage, it is reasonable to proceed negative CT or MRI, or aneurysm detected on CT or MRI for small lesions or to delay surgery, typically between 0 and 4 weeks, depending PET/CT on the size of involvement and the urgency of the operations.” Suspicion of prosthetic valve or pacemaker lead endocarditis with negative echo Thuny F, et al. Imaging investigations in infective endocarditis: Current approach and perspectives. Arch Cardiovascular Dis, 2013 Amat-Santos IJ et al. Prosthetic valve endocarditis after transcatheter valve replacement JACC: Cardiovascular Interventions 8:2015 7
Recommend
More recommend