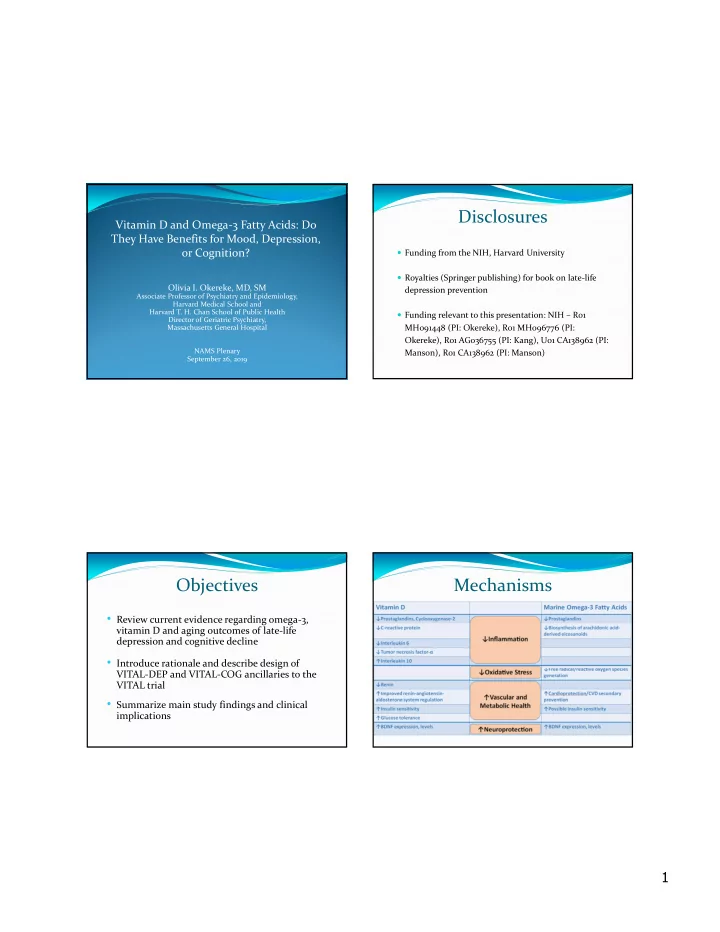
Disclosures Vitamin D and Omega ‐ 3 Fatty Acids: Do They Have Benefits for Mood, Depression, or Cognition? Funding from the NIH, Harvard University Royalties (Springer publishing) for book on late ‐ life Olivia I. Okereke, MD, SM depression prevention Associate Professor of Psychiatry and Epidemiology, Harvard Medical School and Harvard T. H. Chan School of Public Health Funding relevant to this presentation: NIH – R01 Director of Geriatric Psychiatry, Massachusetts General Hospital MH091448 (PI: Okereke), R01 MH096776 (PI: Okereke), R01 AG036755 (PI: Kang), U01 CA138962 (PI: NAMS Plenary Manson), R01 CA138962 (PI: Manson) September 26, 2019 Objectives Mechanisms • Review current evidence regarding omega ‐ 3, vitamin D and aging outcomes of late ‐ life depression and cognitive decline • Introduce rationale and describe design of VITAL ‐ DEP and VITAL ‐ COG ancillaries to the VITAL trial • Summarize main study findings and clinical implications 1
Omega-3 Fatty Acids and Depression: Omega-3 Fatty Acids and Cognition: Review of Evidence Review of Evidence Observational Observational Largely support high fish and omega ‐ 3 intake as associated Largely support high fish and omega ‐ 3 intake as with better mood associated with slower cognitive decline in older adults (prospective, community ‐ based) Experimental Experimental Over a dozen trials, meta ‐ analyses; few with higher dose range ( ≥ 1 g/d) and long duration; most <6 months Few trials with large samples, >12 month duration; fewer with very long duration (>4 years) Track record in depression treatment context; EPA>DHA Results largely null Largely null for prevention (including recent MooDFOOD trial – Bot et al., JAMA 2019) Trials focused on higher ‐ risk groups such as with MCI support benefit (e.g., OmegAD trial, JAMA/Archives Mendelian randomization study in ~500,000: no evidence Neurolgy) for association of n ‐ 3 PUFA with depression (Milaneschi et al., Transl Psychiatry, 2019) Summary and Limitations of Current VITAL ‐ DEP: NAM Framework for Evidence Prevention Observational Studies Modality Target Bias and confounding Indicated Presence of sub ‐ syndromal depressive Variable exposure (fish, n ‐ 3 from diet, etc.) symptoms Experimental Studies Short treatment durations Selective Presence of high ‐ risk factors: e.g., physical/ Variable dosing functional impairment, living alone, anxiety Smaller sample sizes (very low power for primary or universal prevention) Universal General population, regardless of risk status Low diversity Inconsistent use of biochemical nutrient markers 2
Summary of Characteristics: Summary of Characteristics: VITAL ‐ DEP VITAL ‐ COG N 18,353 Table 1. Key Pre ‐ randomization characteristics (n=3583) Mean age ± SD, years 67.5 ± 7.1 Male/female ratio 49.6/50.4 Sex, % female 9,023 (49.2) Mean age ± SD, yrs 67.2 ±7.0 Race/ethnicity, % High school diploma/GED Non ‐ Hispanic White 13,097 (72.8) or higher, % 99.2 African American 3,407 (18.9) African American (AA), % 10.0 Hispanic (not African American) 708 ( 3.9) Current smoker, % 4.4 Mean body mass index, kg/m 2 28.5 Asian/Pacific Islander 294 ( 1.6) Obesity (BMI ≥ 30 kg/m 2 ), % 27.8 American Indian/Alaskan Native 150 (0.8) History of diabetes, % 11.9 Mean body mass index (kg/m 2 ) ± SD 27.8 (5.5) History of hypertension, % 53.1 Current smoking, % 1,121 ( 6.1) Lifetime history of diagnosed depression Hypertension, treated, % 9,198 (50.4) or having used antidepressants, % 18.6 High cholesterol, treated, % 6,624 (36.3) Diabetes, % 2,308 (12.6) 409 AA added post ‐ randomization, for total of 767 (out of n=3,992) Vitamin D Potential Confounding Paths: Vitamin D and Depression: Review of Role of Aging Evidence Older Age Observational (systematic reviews and meta ‐ Poor Nutrition: Low Intake of Low Sun Exposure analyses) Vitamin D Majority of prospective studies show association between 25(OH)D level and lower risk of depression (Okereke et al., J Affect Dis, 2016) Evidence of dose ‐ response: 12% ↓ HR of depression per Low 25(OH)D 10 ‐ ng/ml increment 25(OH)D (Li et al., AJGP, 2019) Experimental/Quasi ‐ experimental Low Physical Activity Obesity Almost all RCTs null, including recent D ‐ Vitaal and MooDFOOD (2019) – both at >800 IU/d for 12 months ? ? Mendelian randomization study in ~500,000: no evidence for association of 25(OH)D with depression (Milaneschi et al., Transl Psychiatry, 2019) Depression and Poor Cognition 3
Vitamin D and Cognition: Review of Summary: VITAL ‐ DEP and VITAL ‐ COG Evidence Strengths: Observational (systematic reviews and meta ‐ Large ‐ scale nationwide racially/ethnically diverse cohort Power to address universal prevention analyses) Experimental design Long ‐ term (>4 years) prospective studies consistent with High follow ‐ up rates and compliance favorable association, especially if clear contrast of >75 vs Validated measures for endpoints, strong follow ‐ up and low 25(OH)D safety plans Experimental/Quasi ‐ experimental Limitations: Longest term, large study to date in WHI – null Dosing – optimal match of dose for each outcome? Long treatment duration (7.8 y) but low dose (400 IU/d) Balance of EPA, DHA for mood or cognition Mendelian randomization study in >170,000: no evidence Shorter follow ‐ up for cognitive outcome (2 years) for association of 25(OH)D with global memory composite Questions about exposure timing for cognitive outcome score (Maddock et al., Sci Rep, 2017) Generally sufficient biochemical levels in cohort VITAL ‐ DEP: Schematic of Current and PRACTICAL PRACTICAL TIPS SUMMA TIPS SUMMARY Future Plans VITAL parent trial 25,871 initially healthy men (aged ≥50) and women (aged ≥55) randomized • Use substitutions VITAL blood VITAL CTSC equally to vitamin D 3 and/or marine n~17,000 N=1,054 • Calories ≠ Quality 1 omega‐3 fatty acids or placebos Plasma 25(OH)D VITAL‐DEP VITAL‐DEP CTSC • Consider: Type vs. Total and omega‐3 Psychiatric interviews, Yearly questionnaires to identify incident • Sources: Plant vs. Animal assays in all self‐rated symptoms, 2 and recurrent depression cases (18,353), participants with cognitive tests at baseline PHQ‐8 scores (all) blood samples and 2‐yr follow‐up (N~700) • Use color • Biochemical nutrient Testing effects of vitamin D 3 and/or levels of vitamin D and • Healthy plate is varied omega‐3 on long‐term mood outcomes; 3 • High‐risk factors omega‐3 and long‐ CMS linkage; racial/ethnic disparities (indicated and term depression selective prevention) outcomes (n~11,500) • Serum BDNF, plasma • Bioavailable vitamin D metabolomics (N~1,000) Okereke et al., Contemp Clin Trials , 2018 Available through AARP, GCBH 4
Clinical and Public Health Implications Omega ‐ 3 Fatty Acids: No change to encouraging fish intake >2 servings/week No change to existing guidelines or practices re: use of omega ‐ 3 in treatment contexts (unipolar depression and bipolar disorder) Vitamin D No clinical guidelines exist re: vitamin D and depression prior to study No changes from current guidelines for daily intake in older persons 5
Recommend
More recommend