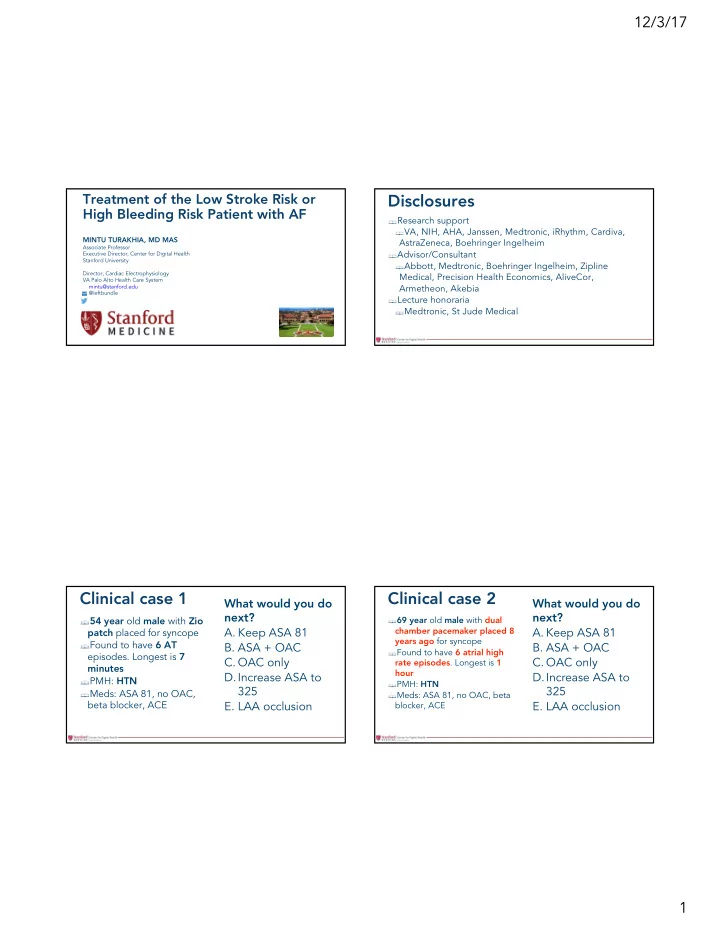
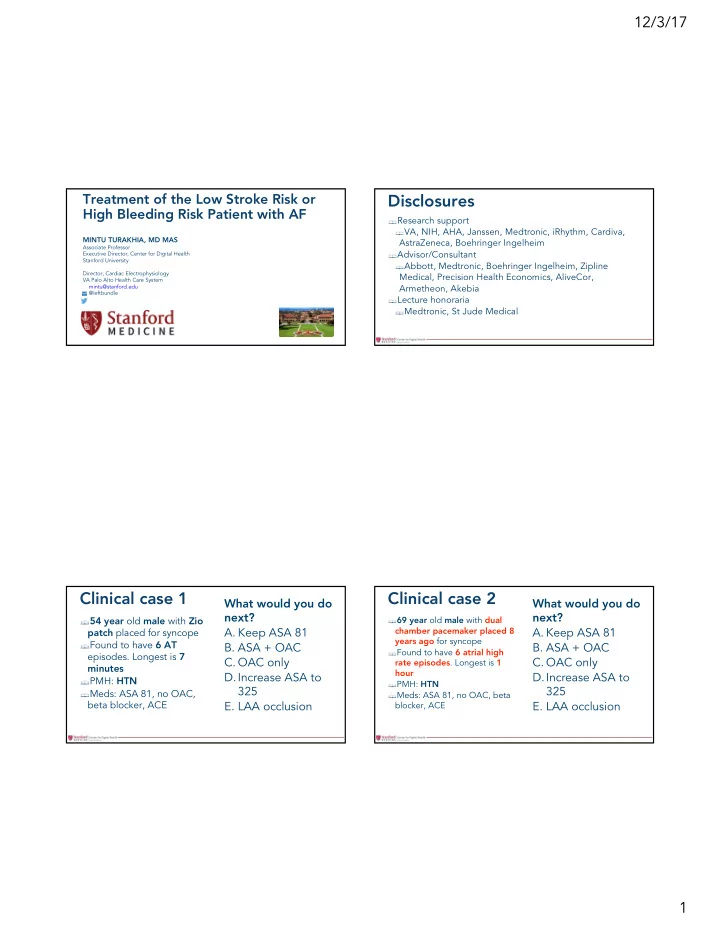
12/3/17 Treatment of the Low Stroke Risk or Disclosures High Bleeding Risk Patient with AF § Research support § VA, NIH, AHA, Janssen, Medtronic, iRhythm, Cardiva, MINTU TURAKHIA, MD MAS AstraZeneca, Boehringer Ingelheim Associate Professor § Advisor/Consultant Executive Director, Center for Digital Health Stanford University § Abbott, Medtronic, Boehringer Ingelheim, Zipline Director, Cardiac Electrophysiology Medical, Precision Health Economics, AliveCor, VA Palo Alto Health Care System Armetheon, Akebia mintu@stanford.edu @leftbundle § Lecture honoraria § Medtronic, St Jude Medical Clinical case 1 Clinical case 2 What would you do What would you do next? next? § 54 year old male with Zio § 69 year old male with dual A. Keep ASA 81 A. Keep ASA 81 chamber pacemaker placed 8 patch placed for syncope years ago for syncope § Found to have 6 AT B. ASA + OAC B. ASA + OAC § Found to have 6 atrial high episodes. Longest is 7 C. OAC only C. OAC only rate episodes . Longest is 1 minutes hour D.Increase ASA to D.Increase ASA to § PMH: HTN § PMH: HTN 325 325 § Meds: ASA 81, no OAC, § Meds: ASA 81, no OAC, beta beta blocker, ACE E. LAA occlusion E. LAA occlusion blocker, ACE 1
12/3/17 Clinical case 3 Clinical case 4 What would you do What would you do next? next? § 76 year old female with ILR § 70 year old female with chronic AF A. Keep ASA 81 and small intracranial hemorrhage A. ASA only placed 1 year ago for syncope 90 days ago while on on warfarin comes for routine check B. ASA + OAC B. NOAC only (INR 2.7) + ASA. Minor speech and § Found to have 6 AF motor deficits C. OAC only C. ASA + NOAC episodes . Longest is 3 days § PMH: HTN , stroke 3 years ago, EF § PMH: HTN , diabetes, EF 45% D.Increase ASA to D.LAA occlusion 50%, GFR 74 § Meds: ASA 81, no OAC, beta § Meds: beta blocker, ACE, no OAC 325 E. Nothing or ASA blocker, ACE E. LAA occlusion § ECG: AF, LVH, V-rate 70s Prevalence of AF “When the gods wish § 4% of the population over age 60; 10% over age 80 to punish us, they 2030: 7.00 answer our prayers.” 5M-12M 2017: 2009: (3-5M) 5.25 1995: 2.23M 1.8M 3.50 1.75 Projections of AF Prevalence in the USA 0.00 Go AS. JAMA. 2001 / Miyasaka Y. Circulation 2006 / Naccarelli GV. Am J Cardiol. 2009 2
12/3/17 Take home points Stroke shortens lifespan the most 1. Clinical decision making is based on poor data Framingham Heart Study 2. AF-stroke relationship is complex Average Remaining Life Expectancy at Age 60 (Men) § Causation vs. risk marker vs. coincident 20 -7.4 -12 years -9.2 years § Atrial rhythm vs. atrial substrate years 16 3. Well-managed and well-selected anticoagulation is 12 generally low risk even after major bleeding 8 4. Don’t use aspirin as an attempted compromise 4 0 Healthy History of History of History of Cardiovascular Disease AMI Stroke Peeters A, et al. Eur Heart J. 2002 First, there was CHADS2 § 1 point for § C ongestive heart failure § H ypertension Risk stratification § A ge ≥ 75 § D iabetes for stroke § 2 points if prior S troke or TIA § Not generalizable! § Bad data § QI Medicare registry (age > 65) from 7 states in the South § 1733 inpatients discharged with AF. Follow-up < 3 years § ICD9 codes, not chart review Gage BF, JAMA 2001 3
12/3/17 Validation: how good is CHADS2? Then came CHA 2 DS 2 -VASc… § Answer: not very § c-statistic = 0.56-0.62 § (0.50 = pure chance) § Substantial misclassification § Untreated “low risk” patients who get strokes § Treated “high risk” patients who bleed (Fang M, JACC 2006) (Lip GY, Chest 2010) Weaknesses of CHA 2 DS 2 -VASc Why did guidelines go with CHA2DS2-VASc? § CHADS2 score gets § Score is calibrated for for high sensitivity reclassified upward § Contemporary therapy has tilted in favor § Age, CAD, female of having a low treatment threshold § Few stroke events in derivation § Low bleeding risk with NOACs § European Heart Survey § Warfarin: less ICH, major bleeding now § 1,577 of 5,333 untreated AF patients 2003-2004 § 1-year follow up (Lip GY, Chest 2010) 4
12/3/17 Summary of NOAC trials ESC AHA ACC HRS RE-LY (Dabigatran) ROCKET-AF ARISTOTLE ENGAGE AF (Apixaban) (Rivaroxaban) TIMI 48 (Edoxaban) 1.69 vs. 1.11 Efficacy % 1.60 vs. 1.27 p < 1.80 vs. 1.57 p=.08 2.42 vs. 2.12 p=.12 p<.001 .001 Warfarin vs. OAC (1.5 vs. 1.18 on treatment) NNT = 167 (2.2 vs 1.7 on treatment) NNT = 303 (CVA or SE) *High-dose (60 mg) *150 mg shown 3.57 vs. 3.32 3.09 vs. 2.13 Major Bleeding % 3.45 vs. 3.6 p=0.58 3.43 vs. 2.75 p<.001 p=0.31 p<.001 0.74 vs. 0.30 0.74 vs. 0.49 0.47 vs. 0.24 p< ICH% 0.85 vs. 0.39 p< .001 p=.019 .001 p< .001 4.13 vs. 3.64 3.94 vs 3.52 4.35 vs. 3.99 p=0.08 All-cause mortality 4.91 vs. 4.52 p=NS p = 0.051 %/yr p = 0.05 NNT = 277 NNT = 204 NNT = 238 Conclusion vs. Superior efficacy, Superior efficacy, less Non-inferior on efficacy Non-inferior on efficacy; similar bleeding, less major bleeding and warfarin and safety measures less bleeding ICH ICH, lower mortality Low stroke risk is the greatest area of uncertainty R 2 CHADS 2 : Yet another risk score § Derivation: ROCKET-AF (rivaroxaban) 20 Annual Risk of Stroke (%) Lip GY, Am J Med . 2010 CHADS 2 Camm AJ, Eur Heart J . 2010 § Validation: Kaiser 18 Friberg L, JACC , 2015 CHA 2 DS 2 -VASc § Adding a binary predictor of GFR < 60 to 16 14 CHADS2 score substantially improves discrimination and reclassification 12 10 § c-statistic 0.74 8 § AHA/ACC/HRS 2014 guidelines did not 6 endorse R2CHADS2 4 2 0 0 1 2 3 4 5 6 7 8 9 (Piccini J, Circulation 2012) 5
12/3/17 Limitations of stroke risk scores Q: What is this patient’s annual risk of stroke? Answer choices: § Risk factors § AF defined by treatment, not disease 1. Very low (< .5%) § Age 67 § Hospitalization with AF; cardiology care 2. Low (~1-2%) § Female § ICD9 codes, not AF burden 3. Medium (~3-6%) § Carotid disease § Transient or lone AF not well represented 4. High (~8-18%) § GFR < 60 § Diagnosis creep § Device-detected AF, ambulatory ECG, episodic ‣ CHADS 2 : 0 (low) detection with wearables ‣ CHA 2 DS 2 -VASc: 3 (med) § Result: external miscalibration and overtreatment ‣ R 2 CHADS 2 : 2 (med) Vascular risk factors also predict AF Mechanisms of stroke in AF are diverse § In non-AF patients, § Cardioembolic CHADS2 and other scores § Atheroembolic predict… § Small vessel § Left atrial dysfunction, § CHA2DS2-VASc increase LAA thrombus risk of all types § Ischemic stroke § More AF in all types § AF Welles C / Turakhia M, JACC 2011 Welles C / Turakhia M, Am Heart J 2013 Wong J / Turakhia M, Am Heart J 2014 Melgaard L, JAMA 2015 6
12/3/17 Rethinking the conceptual framework LA dysfunction AF Stroke LA AF Stroke dysfunction How much AF is too much? LA Stroke dysfunction AF Other vascular AF LA dysfunction risk factors Stroke ASSERT Study § AF subtype clinically classified, not based on ECG monitoring (Healey JS, NEJM 2012) Vanassche T, Eur Heart J , 2015 7
12/3/17 Short AT/AF and stroke (ASSERT) ASSERT § Among 51 patients with stroke/SE § Only 1 had AT/AF at time of stroke § Subclinical atrial tachyarrhythmias (AT) (> 6 § 25 (49%) had no AT/AF minutes) in 10% by 3 months § Only 4 (8%) had AT/AF > 6 min in prior 30 days AT associated w/clinical AF (HR 5.6) § Median time to AF was 339 days prior § AT associated w/ischemic stroke/SE (HR 2.5) § 8 had AT/AF only after stroke § But, population attributable Atrial tachycardia risk low: 13% Healey JS, NEJM 2012 (Brambatti M, Circulation 2014) SOS-AF § Pooled analysis § 10,000 patients with PPM, ICD, CRT Boriani G et al. Eur Heart J , 2014 Freedman B, Circulation , 2017 8
12/3/17 Is there transient risk? REVEAL AF Threshold did not Enrollment matter (30 sec to 6 DESIGN: Baseline hours) – risk pattern • Prospective, single-arm, open-label, multi- Successful Reveal was the same center, post-market study ICM insertion • Enrollment November 2012 – June 2015 Contribution to Monthly device INCLUSION CRITERIA: transmission prediction • CHADS 2 score of ≥ 3 or CHADS 2 = 2 and at least 1 of the following: (attributable risk) In-office follow-up • CAD, CKD, Sleep apnea, COPD visits every is low 6 months for a minimum of 18 and Primary outcome maximum of 30 months • Incidence of adjudicated AF ≥6 minutes at 18 months Turakhia M, et al . Circ EP , 2015 Reiffel J, et al. Am Heart J 2014;167:22-27. Trial pipeline RE REVEAL AF: In Incid idence of AF AF Last stin ing ≥ 6 Min inutes • Median time to detection: 123 • [IQR 41-330] days. • Detection rate at: Incidence Rate, % – 18 months (primary endpoint): 29.3%. – 30 days: 6.2%. – 30 months: 40.0%. • AF may have gone undetected in over ¾ of patients had monitoring been limited to 30 days Number of Months Post-Insertion Gorenek B, et al (EHRA Consensus Document), Europace, 2017 Data presented by James A. Reiffel, MD. HRS Chicago May 5, 2017. 9
12/3/17 Clinical recommendations Clinical recommendations OAC treatment by site for AF ≥ 1 hour (PPM, ICD) § 12,000 VA patients with Carelink data + EHR + labs § 1,967 with AF ≥ 1 hour and > 75% remote monitoring coverage § ≥ 6 minutes: 292/2431 (12%) § > 6 hours: 279/1455 (19%) § > 24 hours: 232/914 (25%) Gorenek B, et al (EHRA Consensus Document), Europace, 2017 Perino AC / Turakhia MP, in review 10
Recommend
More recommend