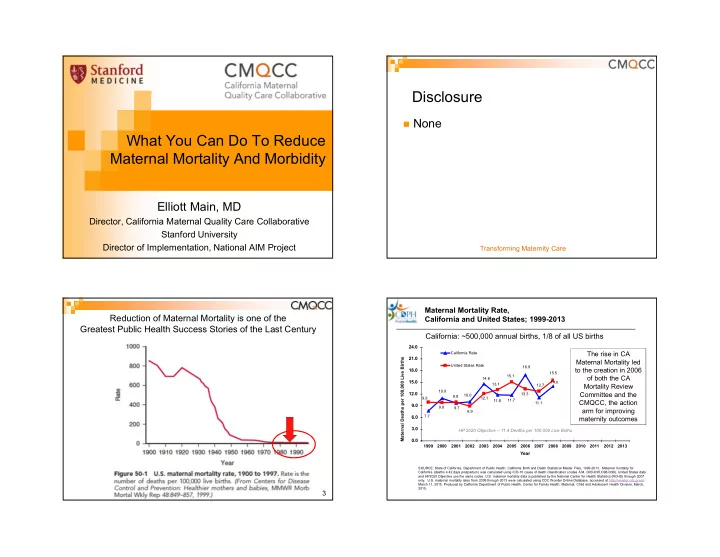
Disclosure None What You Can Do To Reduce Maternal Mortality And Morbidity Elliott Main, MD Director, California Maternal Quality Care Collaborative Stanford University Director of Implementation, National AIM Project Transforming Maternity Care Maternal Mortality Rate, Reduction of Maternal Mortality is one of the California and United States; 1999-2013 Greatest Public Health Success Stories of the Last Century California: ~500,000 annual births, 1/8 of all US births 24.0 22.0 California Rate The rise in CA 21.0 Maternal Deaths per 100,000 Live Births 19.3 Maternal Mortality led United States Rate 16.9 to the creation in 2006 19.9 18.0 16.6 15.5 16.9 15.1 of both the CA 14.6 15.0 14.0 13.1 Mortality Review 12.7 11.6 10.9 Committee and the 12.0 13.3 10.0 9.9 9.9 12.1 11.7 9.2 11.8 CMQCC, the action 11.1 9.0 9.8 7.4 9.7 arm for improving 8.9 7.3 6.0 7.7 maternity outcomes 6.2 3.0 HP 2020 Objective – 11.4 Deaths per 100,000 Live Births 0.0 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 Year SOURCE: State of California, Department of Public Health, California Birth and Death Statistical Master Files, 1999-2013. Maternal mortality for California (deaths ≤ 42 days postpartum) was calculated using ICD-10 cause of death classification (codes A34, O00-O95,O98-O99). United States data and HP2020 Objective use the same codes. U.S. maternal mortality data is published by the National Center for Health Statistics (NCHS) through 2007 only. U.S. maternal mortality rates from 2008 through-2013 were calculated using CDC Wonder Online Database, accessed at http://wonder.cdc.govon March 11, 2015. Produced by California Department of Public Health, Center for Family Health, Maternal, Child and Adolescent Health Division, March, 2015. 3
US Maternal Mortality Rates Have Risen Using Either Death Certificates (NCHS) Or Using MD Case Reviews by CDC PMSS 20 The US has the Mortality Rate (per 100,000 Live births) 19 highest Maternal 18 17 Mortality rate of 16 16 any high resource 15 14.5 country and the 14 only country 12 11.5 11.5 outside of 10 Afghanistan and 9 Sudan where the 8 8 7.5 rate is rising. 6 4 (CDC, Gates Foundation) 1987-1990 1991-1997 1998-2005 2006-2010 2011-2013 July 17, 2015 MMR (NCHS Death Certificate) MMR (CDC PMSS) The U.S. has the worst rate of maternal deaths in the developed world, and 60 percent are preventable PBS NewsHour August 18, 2017 1.6% Why are more American women dying after childbirth? 2X Why are more American women “The Last Person You’d Expect to Die dying after childbirth? in Childbirth” cdc.gov 7
Maternal Mortality and Severe Morbidity Underlying causes, compiled from multiple studies Severe Morbid Mortality ICU Admit Cause ( 1-2 per (1-2 per (1-2 per 10,000) 1,000) 100) VTE and AFE 15% 5% 2% Infection 10% 5% 5% Hemorrhage 10-15% 35% 55% Preeclampsia 15% 25% 25% Cardiac Disease 25% 15% 5% 10 Assessments of Preventability Provider Contributing Factors in Maternal Deaths (California) Cause of Death North Carolina California United Kingdom “Preventable” “Good or strong “Substandard chance to alter care that had a the outcome” major contribution” Hemorrhage 93% 70% 44% Preeclampsia 60% 60% 64% Sepsis / Infection 43% 50% 46% DVT / VTE 17% 50% 33% From detailed chart reviews of maternal deaths Cardiomyopathy 22% 29% 25% (CA-Pregnancy Associated Mortality Review Committee; CDPH-MCAH) Amniotic Fluid 0% 0% 15% Embolism Main EK, McClain CL, Morton CH, Holtby S, Lawton ES. Pregnancy-related mortality in 11 California: Causes, characteristics and improvement opportunities. Obstet Gynecol 2015
Key Provider QI Opportunities: Obstetric Hemorrhage and Hemorrhage and Preeclampsia Preeclampsia: Summary • California Pregnancy Associated Mortality Reviews Most common preventable causes of – Missed triggers/risk factors: abnormal vital signs, pain, altered mental status/lack of planning for at risk patients maternal mortality – Underutilization of key medications and treatments—did not Present in >95% of cases Far and away the most common causes have a plan! of Severe Maternal Morbidity – Difficulties getting physician to the bedside – “ Location of care ” issues involving Postpartum, ED and PACU High rates of provider • University of Illinois Regional Perinatal Network “quality improvement opportunities” - Failure to identify high-risk status Present in >90% of cases - Incomplete or inappropriate management CDPH/CMQCC/PHI. The California Pregnancy-Associated Mortality Review (CA-PAMR): Report from 2002 and 2003 Maternal Death Reviews. 2011 (available at: CMQCC.org) Geller SE etal. The continuum of maternal morbidity and mortality: Factors associated with 13 14 severity. Am J Obstet Gynecol 2004; 191: 939-44. Hemorrhage Toolkit >10,000 Downloads to date
Maternal Safety Bundles Obstet Gynecol. 2015 Jul;126(1):155-62 First Bundle: What are they? July 2015 • “Checklist” of items and practices for every birthing site • Not a national protocol !! J Obstet Gynecol Neonatal Nurs. • Facilities will modify content 2015 Jul;44(4):462-70. based on local resources Uniform Structure: Anesth Analg 2015;121:142–8 • R eadiness Every unit—prepare and educate • R ecognition & Prevention Every patient—before event • R esponse Every Event—team approach Available at: • R eporting/Systems Learning Every unit—systems safehealthcareforeverywoman.org improvement with resource links 18 J Midwifery Womens Health. 2015 Jul;60(4):458-64. OB Hemorrhage - Readiness “Just in Time” Education Every unit Hemorrhage cart with supplies, checklist, Put into the hands of doctors, midwives and nurses instruction cards and posters key information… at the moment of its use (Cart) Immediate access to hemorrhage medications Response Education Establish a response team – who to call when Management Plan with checklist (reminders) help is needed Uterotonic Medication Guide: pros and cons Establish massive and emergency release How To Do: Steps to place an intrauterine balloon transfusion protocol/policies How To Do: B-Lynch Suture Unit education on processes, unit-based drills Blood Product Information (with debriefs)
Example Patient Level Readiness Hemorrhage Emergency Women with Placenta Accreta or Percreta Response Plan Women with inherited coagulation disorders Jehovah’s Witness Tools are adapted Informed Consent and Decline checklists, for each hospital's Pregnancy planning guide resources Iron Sucrose and Ferric Carboxymaltose Protocols www.CMQCC.org CMQCC OB Hemorrhage Care Guidelines Intervention Delay that increased risk for severe hemorrhage Oxytocin administration >10 minutes Obstetrician present or >10 minutes notified Anesthesiologist present or >10 minutes notified Manual examination of the >20 minutes uterine cavity Can be posted on L&D or Placed on the Charge Nurse’s Clipboard Driessen M et al., Obstet Gynecol 2011; 117:21-31 23
Deciding to Transfuse: Lancet 2017;389:2105-16 (on line April 26) “Combination Logic” EBL >1500? EBL and even QBL are not perfect Vital Signs suggesting hypovolemia? How much crystaloid is on board, is it barely RCT of 20,000 women with PPH in both low and high maintaining the BP? Good to a point… resource countries, dose was 1gm IV (may repeat x1) Is the bleeding under control or continuing? Maternal death was reduced by 30% among women treated within 3 hours of bleeding Any chance for concealed hemorrhage? Hysterectomy was not reduced (many cases were already at that stage at time of randomization) Be Wary of CMQCC TXA Recommendations for PPH Concealed Hemorrhage TXA is not for prophylaxis or initial treatment Consider use after higher dose oxytocin/ methergine have been tried and before additional drugs/procedures (after CMQCC Stage 1) Respect the dose: 1 gm IV, may repeat in 30min x1 Intra-abdominal bleeding Post Cesarean Safety issues: Posterior Uterine Rupture Task overload—need to ensure that basic PPH tasks Extension of Cervical or Vaginal Side-wall are attended to Potential for serious drug error, vial can be confused Laceration with bupivicaine; intrathecal TXA injection is serious Higher doses of TXA are associated with renal toxicity Extra, objective eyes are critical! See summary document on TXA Recommendations at www.CMQCC.org
Not just placenta accreta… 8/3/2017 8/21/2017 How Judge Hatchett’s Son Is Coping After (Healthy woman with major His Wife’s Childbirth Death complications during “routine” repeat Cesarean: “Near Miss” (Healthy woman with complications resulting now with PTSD) in death during “routine” repeat Cesarean) 30 Patient Safety Bundle for Hypertension Practical advice for Focus points establishing Use standard language and Patient definitions for preeclampsia Family and (e.g. with severe features) Staff support Standardize the measurement of blood pressure! on your unit: Use ACOG protocols for treatment of severe range BP within 60 min Standard protocols for the use of MagSO4 Early Postpartum follow-up www.safehealthcareforeverywoman.org 31
Recommend
More recommend