Disclosure Early Prediction of Chronic Pulmonary Not a cardiologist - PDF document
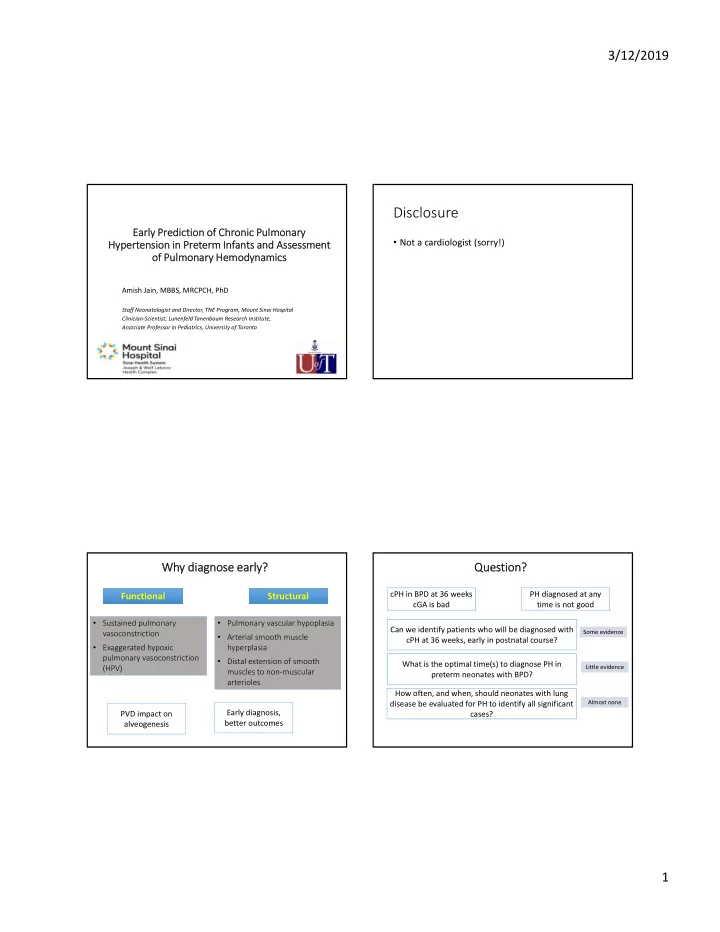
3/12/2019 Disclosure Early Prediction of Chronic Pulmonary Not a cardiologist (sorry!) Hypertension in Preterm Infants and Assessment of Pulmonary Hemodynamics Amish Jain, MBBS, MRCPCH, PhD Staff Neonatologist and Director, TNE Program,
3/12/2019 Disclosure Early Prediction of Chronic Pulmonary • Not a cardiologist (sorry!) Hypertension in Preterm Infants and Assessment of Pulmonary Hemodynamics Amish Jain, MBBS, MRCPCH, PhD Staff Neonatologist and Director, TNE Program, Mount Sinai Hospital Clinician‐Scientist, Lunenfeld Tanenbaum Research Institute, Associate Professor in Pediatrics, University of Toronto Why diagnose early? Question? cPH in BPD at 36 weeks PH diagnosed at any Functional Structural cGA is bad time is not good • Sustained pulmonary • Pulmonary vascular hypoplasia Can we identify patients who will be diagnosed with Some evidence vasoconstriction • Arterial smooth muscle cPH at 36 weeks, early in postnatal course? • Exaggerated hypoxic hyperplasia pulmonary vasoconstriction • Distal extension of smooth What is the optimal time(s) to diagnose PH in (HPV) Little evidence muscles to non‐muscular preterm neonates with BPD? arterioles How often, and when, should neonates with lung disease be evaluated for PH to identify all significant Almost none Early diagnosis, PVD impact on cases? better outcomes alveogenesis 1
3/12/2019 4‐6 weeks < 28 weeks, N=120, 10 ePH, 5 PH 10‐14 days FiO2 @ 10 days ‐>ePH ‐> BPD ePH≠PH 7 days 5‐7 days ‘Early’ PH studies Retrospective – selection bias (343/1172 had a clinical echo) 3‐14 days ePH 23% ePH ‐> BPD/mortality ePH≠PH < 30 weeks, N=67, ePH 16% 2‐14 days ePH ‐>BPD ePH≠PH (low sEI on late scan) 4‐6 weeks <30 weeks, O2>4 weeks, N=126 32 weeks CGA ePH 28% (4‐6 weeks) 22% (32 weeks) 17%(36 weeks) [@ any 38%] ePH≠PH 4‐6 weeks Day 5‐7 (N=98) 36 weeks (N=164) 7 days 5‐7 days 2
3/12/2019 Sensitivity 62% At day 7, 41% had PH Specificity 61% Diagnostic criteria used GA/Weight Lung disease (MV/high Severity of BPD FiO2 early in course) Levy/ Mourani Bhat • RV hypertrophy • RVSP > 40 mmHg • Flat IV septum • RVSP:SBP > 0.5 “Late” PH “Early” PH • TR jet • BD/RL shunt Mortality • ‘elevated’ RV pressure • Flat IV septum at end systole In‐hospital resp morbidity Post‐discharge resp ?adverse ND YES YES Currently employed diagnostic criteria (flat septum) are unlikely to be effective in identifying cPH kids early in NO NO postnatal course We are struggling to identify pulmonary vascular disease in preterm neonates early in NICU course 3
3/12/2019 Pulse‐wave Doppler of main pulmonary artery Time in milliseconds Echocardiography indices of pulmonary hemodynamic alternations Velocity (cm/s) b a Echocardiography indices of Right heart • Right ventricular ejection time (RVET) = a performance • Pulmonary artery acceleration time (PAAT) = b ‐ inversely related to PVR Exploratory vs. planned diagnostic investigation • Pulmonary vascular resistance index (PVRI) = a/b ‐ directly related to PVR Steady (resistance) vs. Pulsatile (compliance) afterload Compliance Resistance 4
3/12/2019 RVOT Doppler Shape Resistance vs. Compliance Joye et al PAS 2019 5
3/12/2019 Early identification of preterm neonates with evolving chronic pulmonary hypertension: utility of functional echocardiographic markers Sample size: 350 to estimate a sensitivity of 85% with an absolute precision of 0.07 6
Recommend
More recommend
Explore More Topics
Stay informed with curated content and fresh updates.