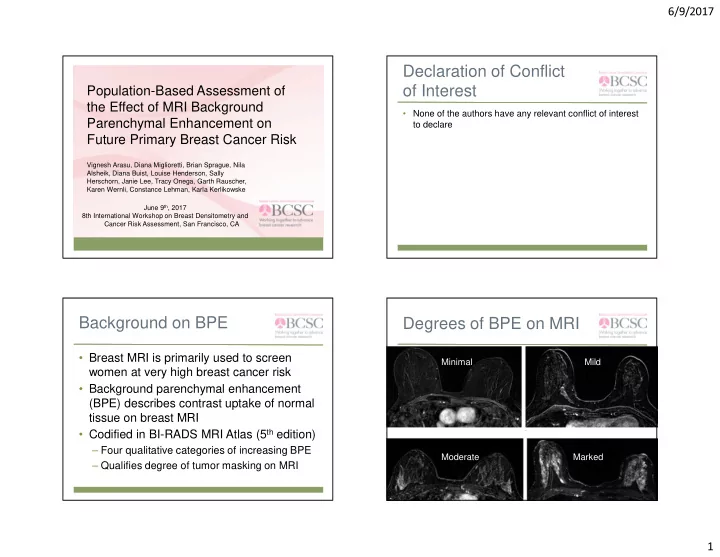
6/9/2017 Declaration of Conflict of Interest Population-Based Assessment of the Effect of MRI Background • None of the authors have any relevant conflict of interest Parenchymal Enhancement on to declare Future Primary Breast Cancer Risk Vignesh Arasu, Diana Miglioretti, Brian Sprague, Nila Alsheik, Diana Buist, Louise Henderson, Sally Herschorn, Janie Lee, Tracy Onega, Garth Rauscher, Karen Wernli, Constance Lehman, Karla Kerlikowske June 9 th , 2017 8th International Workshop on Breast Densitometry and Cancer Risk Assessment, San Francisco, CA Background on BPE Degrees of BPE on MRI • Breast MRI is primarily used to screen Minimal Mild women at very high breast cancer risk • Background parenchymal enhancement (BPE) describes contrast uptake of normal tissue on breast MRI • Codified in BI-RADS MRI Atlas (5 th edition) – Four qualitative categories of increasing BPE Moderate Marked – Qualifies degree of tumor masking on MRI 1
6/9/2017 BPE as imaging Research objectives biomarker • Recognition as novel imaging biomarker • Evaluate MRI BPE risk prediction on future • Reflects breast vascularity, permeability, and primary breast cancer risk peri-vascular factors present in stroma • Evaluate comparative risk prediction to – Whereas breast density reflects ducts and stroma breast density • Dynamic with hormonal variation – Influenced by age, menstrual cycle, menopause, and hormone therapy • Single-center studies demonstrate high BPE is associated with increased breast cancer risk (see King et al. 2011, Dontchos et al 2015) Methods BCSC registries • Observational cohort study from six US Breast Cancer Surveillance Consortium (BCSC) registry sites – 40 breast imaging facilities, 123 radiologists • Study period: 2005-2014 • Predictor: BI-RADS BPE assessment – Cases: BPE at least 3 months prior to diagnosis • Outcome: Cancer diagnosis ascertained through linkage with state or regional cancer registries and pathology databases Active registries Historic registries 2
6/9/2017 Methods Results • Covariates obtained prospectively via clinical • 4976 MRI examinations among 3,358 history surveys and medical record data women included • Primary analysis: Cox proportional hazards • 135 women developed breast cancer model using baseline BPE, stratified by BCSC – 99 invasive (73%) registry site and MRI indication, adjusted for age – 27 DCIS (27%) • Secondary analysis: • Average of 2.5 years of follow-up – Partly conditional repeated measures model – Dichotomized BPE measurement for improved • 60% of examinations were screening MRI interpretation biologically, inter-rater agreement • (min BPE vs. mild/mod/marked BPE) Results: Baseline Table: BPE risk at baseline Characteristics Cancer Cohort Control Cohort • Age: over 80% less than 60 years old BPE Hazard Ratio (95% CI) (N=135 women) (N=3223 women) • Race/ethnicity: 80% were white N % N % • Cases had a higher proportion of Minimal 25 19% 1,080 34% Reference – Pre-menopausal women (54% vs 49%) 1.91 (1.12, 3.27) Mild 41 30% 982 30% – 1 st degree breast cancer family history (64% vs. 59%) 2.23 (1.29, 3.84) Moderate 42 31% 763 24% 2.69 (1.49, 4.87) Marked 27 20% 398 12% 3
6/9/2017 Table: BPE risk, with Table: Breast Density Risk multiple observations Cancer Cohort Control Cohort Cancer Cohort Control Cohort Breast BPE Hazard Ratio Hazard Ratio Density (95% CI) (95% CI) (N=135 women) (N=3223 women) (N=200 obs) (N=4,776 obs) N % N % N % N % Almost entirely Minimal 45 23% 1,679 35% Reference 4 3% 124 5% 1.12 (0.38, 3.25) fat Scattered 1.56 (1.05, 2.33) Mild 61 31% 1,435 30% 24 20% 738 30% Reference fibroglandular Heterogeneously 1.57 (1.00, 2.48) Moderate 53 27% 1,080 23% 53 45% 1,089 44% 1.35 (0.81, 2.24) dense 1.97 (1.14, 3.39) 1.85 (1.06, 3.21) Marked 41 21% 582 12% Extremely dense 38 32% 550 22% Table: BPE versus Table: Stratified analysis of other risk subgroups Breast Density risk Dichotomized BPE overall hazard ratio: 2.17 (1.34, 3.50) (Minimal vs. Mild/Moderate/Marked BPE ) Not dense Dense Other risk subgroups Hazard Ratio (95% CI) P-value 2.58 (1.52, 4.36) Family history Minimal BPE Reference 1.49 (0.61, 3.66) 0.11 1.90 (1.06, 3.43) No family history 2.76 (1.62, 4.68) Mild, Moderate, Pre-menopausal 2.46 (1.04, 5.81) 3.03 (1.40, 6.53) 0.19 Marked BPE 2.21 (1.25, 3.90) Post-menopausal 2.21 (1.14, 4.25) BCSC risk <1.67% • Test for interaction between BPE and density is 0.054 2.76 (1.50, 5.07) BCSC risk >=1.67% not statistically significant (p=0.72) 4
6/9/2017 Table: Stratified analysis of invasive Discussion versus noninvasive disease Dichotomized BPE overall hazard ratio: 2.17 (1.34, 3.50) • High levels of BPE predict increased risk (Minimal vs. Mild/Moderate/Marked BPE ) of primary breast cancer Subgroups Hazard Ratio (95% CI) • In a high risk population, BPE predicted 1.42 (0.60, 3.37) DCIS breast cancer risk independent of breast 2.58 (1.50, 4.44) Invasive density • BPE had a stronger association with cancer than breast density Discussion (continued) Limitations • BPE risk prediction is independent of other • Qualitative BPE is subjective and prone to breast cancer risk factors (age, family inter and intra-observer differences history, benign breast biopsies, – Similar to breast density menopausal status, and BCSC risk score) • Unclear phase of menstrual cycle • BPE is more strongly associated with • BPE “missing data” invasive cancer than DCIS – 2005: 99% • Largest study to date in population-based – 2014: 15% cohort among diverse facilities, replicates prior results 5
6/9/2017 Conclusion Acknowledgements • BPE is a predictor of future breast cancer • Participating women risk independent of breast density with • BCSC investigators stronger associations with invasive cancer • Radiologists and mammography facilities than DCIS • Data collection for this work was • BPE should be considered for supported by the National Cancer incorporation into risk prediction models Institute-funded Breast Cancer for high-risk women undergoing MRI Surveillance Consortium (P01 CA154292 and HHSN261201100031C) Additional slides: Sensitivity analyses for first BPE measure Covariate Hazard Ratio (95% CI) 2.32 (1.40, 3.84) Family history 2.27 (1.36, 3.81) Benign breast biopsy 2.37 (1.40, 4.02) Family History and benign breast biopsy 2.50 (1.39, 4.52) Menopausal status Family History, benign breast biopsy, menopausal 2.48 (1.37, 4.49) status 6
Recommend
More recommend