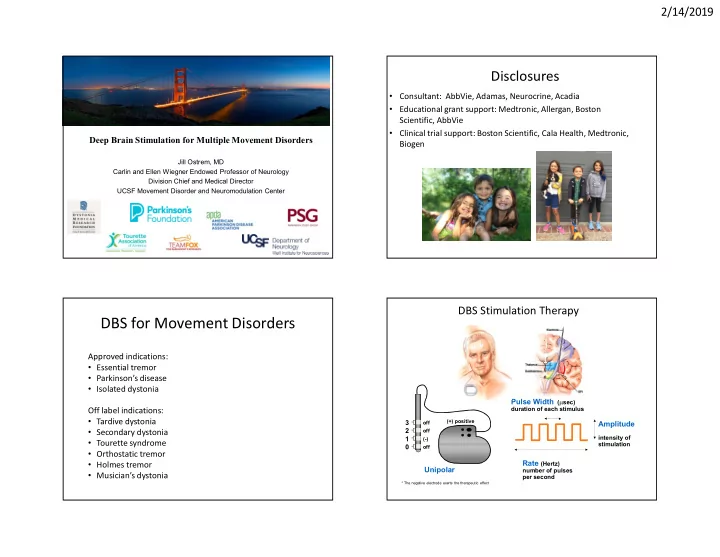
2/14/2019 Disclosures • Consultant: AbbVie, Adamas, Neurocrine, Acadia • Educational grant support: Medtronic, Allergan, Boston Scientific, AbbVie • Clinical trial support: Boston Scientific, Cala Health, Medtronic, Deep Brain Stimulation for Multiple Movement Disorders Biogen Jill Ostrem, MD Carlin and Ellen Wiegner Endowed Professor of Neurology Division Chief and Medical Director UCSF Movement Disorder and Neuromodulation Center DBS Stimulation Therapy DBS for Movement Disorders Approved indications: • Essential tremor • Parkinson’s disease • Isolated dystonia Pulse Width ( sec) duration of each stimulus Off label indications: • Tardive dystonia 3 (+) positive off Amplitude • Secondary dystonia 2 off intensity of 1 (-) • Tourette syndrome stimulation 0 off • Orthostatic tremor Rate (Hertz) • Holmes tremor Unipolar number of pulses • Musician’s dystonia per second * The negative electrode exerts the therapeutic effect 1
2/14/2019 History of DBS Landmarks and Current Approved Indications Major Randomized Parkinson’s Disease Trials Comparing DBS to Medical Therapy European Approvals First DBS Advanced Abbott implanted ET OCD Main findings: PD steering DBS better than medical PD tremor Dystonia therapy alone: Boston MICC Epilepsy ET steering • Decreased OFF time (4.6 hours/day) 1987 1993 1995 1997 1998 2002 2003 2009 2010 2015 2016 2017 2018 2019 • Improved quality of life measures Advanced PD OCD (HDE) Tremor Dystonia FDA >4 ET+PD Boston (HDE) yrs PD MICC Abbott US Approvals steering Boston steering Who is a Candidate for DBS? Who is a Candidate for DBS? (Increased Benefit) (Increased Benefit) Most Candidates: Minority: • Moderate/advanced PD disease Overall milder disease, but: • Levodopa-responsive • Severe rest tremor resistant to levodopa • Experiencing motor fluctuations • Painful off-medication state dystonia • Experiencing dyskinesia • Severe dyskinesia with low doses levodopa • “Failed” good control with medical treatments • Disability preventing employment 2
2/14/2019 Who are not good DBS candidates? Realistic Expectations from DBS (Increased Risk) Identify your patient specific PD symptoms you hope DBS will improve: • Significant psychiatric illness • Tremor • Psychosis • Are these symptoms DBS responsive? Slow movement • Stiffness How levodopa responsive are these symptoms? • Depression • Dyskinesia Tremor and/or dyskinesia in the top 3? • Significant cognitive impairment • Falls/balance • Painful dystonia • Awake surgery, requires patient input • Depression/Anxiety • Hallucinations • Complex, long-term therapy • Poor Speech • Worsening of cognition after surgery, even if motor • Poor Sleep • Freezing symptoms improve? • Unexpected Off time • Significant medical co-morbidities • Medication side effects • Poor dexterity • Unrealistic goals and expectations • Motor fluctuations • Fatigue Parkinson’s Disease Candidacy for DBS Age Cut Off? • Optimization of medications • Detailed motor testing (on and off medications) • Historically over 70 • years not considered Neuropsychological testing candidates for DBS • Psychiatric evaluation (in some cases) • Pre-operative Brain MRI • Now a more individual • Genetic testing? approach is applied Off Medications On Medications Charles, P.D. et al. Neurology 2002;59:932-934 3
2/14/2019 Personalized Parkinson’s Disease DBS Alternative Diagnoses- Poor DBS Responders Which surgical method? One or both sides? Multiple System Atrophy Progressive Supranuclear Palsy Cortical Basal Syndrome • MSA-P, MSA-C, MSA-A • Often no rest tremor • Can be very asymmetric • RBD • Early dementia signs and symptoms • Parkinsonian signs • Early Falls • Problems with skilled • Sometimes “head drop” • Gaze palsy movements - • Stridor • Poor levodopa response apraxia/alien limb • Poor levodopa response Tauopathy • • Cognitive impairment • Autonomic problems Poor levodopa response • Digestive, BP, erectile • T auopathy dysfunction Asleep • Synucleanopathy Awake Need for multi-disciplinary team approach! Which Target? New Generation DBS Systems Major Randomized Parkinson’s Disease Clinical Trials STN Verses GPi DBS • Three commercial DBS companies in the US with FDA approved systems • STN and GPi DBS • Smaller profile, longer-lasting, re-chargeable neurostimulators offer similar overall motoric and quality • Delivering constant current stimulation of life improvement • Segmented steering or current shaping leads • STN DBS allows for • Improved physician and patient interfaces greater medication • reduction Some MRI conditional devices • Some evidence for • Some offer personalized closed-loop adaptive stimulation platforms more cognitive and mood issues with STN • One study secondary endpoint showed STN greater improvement in UPDRS III off meds score 4
2/14/2019 How Early Should We Offer DBS in PD ? DBS Therapy Typical Progression and Clinical Course Typical Progression and Clinical Course Honeymoon Period Preclinical Motor Complication Resistant Cognitive Phase Period Symptoms Decline 0 -2 to -6 3 8 15 20 Years Onset Therapy Diagnosis Fahn. Ann NY Acad Sci. 2003;991:1-14. Ramirez-Zamora, Ostrem; JAMA Neurology 2018 “Early Stim Trail” Schuepbach W. et al • 2 year long German trial • 251 PD with early motor complications (starting 4 mo to 3 years earlier) • Divided patients to DBS plus medication OR medication alone • Primary objective was measurement of quality of life • DBS group improved quality of life scores by ~8 points • Best medical therapy worsened by 0.2 points • DBS superior in motor disability, activities of daily living, levodopa-related complications and time with good mobility New label language – DBS improves quality of life 5
2/14/2019 DBS for Essential Tremor • Largest (N=127 pts) prospective, controlled trial of Vim DBS for ET • DBS system- Constant-current, non directional lead • Unilateral and bilateral leads Who is a Candidate? • 60% improvement in tremor score Failed control with ET meds • Also significant improvement in QoL, • Propranolol depression symptoms, and ADL • Primadone scores • Others? Disability from tremor Most DBS surgery for ET still done awake DBS for Isolated Dystonia Deep Brain Stimulation for ET Candidacy: 1. Failed reasonable, medication • Unilateral stimulation can sometimes treat axial tremor treatment (Artane, Baclofen, benzodiazepine) • Bilateral stimulation results in higher risk for ataxia and 2. Failed botulinum toxin injections for balance issues or dysarthric speech focal dystonia • Loss of stimulation effect over time may be due to tolerance 3. Negative trial of levodopa (R/O DRD) or disease progression 4. Significant disability or pain • Turning stim off at night may result in less “tolerance” to 5. Absence of significant dementia or stim – but controversial depression 6. Absence of significant surgical risk • Posterior Subthalamic Area (PSA) target for proximal tremor factors phenotype or refractory VIM DBS tremor being explored 7. Realistic expectations 8. Risk/benefit acceptable Age at surgery: 11 yo female, 4 year duration of disease, DYT1 6
2/14/2019 Class I Evidence for use of GPi DBS in Isolated GPI DBS Long-term Outcomes DYT1 Generalized and Segmental Dystonia Randomized sham- stimulation N=47 control design Mean improvement in BFMDRS-MS score 25 Markun L, et al. Neurosurgery 71:325–330, 2012 DYT1 Segmental Dystonia Baseline 3 Years after Bilateral STN DBS Neurology 2017;88:25-35 Improvement (36mo) BFMDRS m - 70% N=20 TWSTRS t - 67% 17 yo male, 6 year duration of dystonia Medications: None Previous medication trials: • Botulinum toxin injections both arms • Sinemet and Artane no benefit 7
2/14/2019 Class I Evidence for Use of GPi DBS in Cervical Dystonia Use of GPi DBS in Cranial Dystonia – Meige Syndrome Cranial dystonia can improve but usually not as much compared to other body regions Improvement in dystonia after 6 mo of Gpi DBS Variability in Outcomes Shorter disease duration predicts better outcome (GPI DBS) Generalized dystonia - disease duration correlates with outcomes UCSF experience – DYT1+ Percent improvement in BFMDRS-MS at 100 y = -3.05x + 94.45 90 ρ = -0.71 80 70 final follow-up 60 Non-responders: n=8/40, 20% 50 40 30 20 10 0 0 5 10 15 20 25 Duration of Disease (years) Disease duration (x-axis) correlates with percent improvement in BFMDRS-MS (y-axis) at final follow-up. Each square represents a patient (1-14). Patients with fixed skeletal deformities (3, 4, 6, and 14) are indicated by a square with an “x.” Markun L, et al. Neurosurgery 71:325–330, 2012 31 8
2/14/2019 Secondary/Combined Dystonia Acquired Dystonia - Less Responsive to DBS • Generally poor responders • How to identify new target with abnormal anatomy? • 13 patients, 24% mean improvement, variable Witt J, Starr P, Ostrem J. Stereotact Funct 2013 Neurodegeneration with Brain Iron Accumulation (NBIA), GPi DBS Tardive Dystonia Syndromes • Can show some improvement, but not as much as isolated Typically respond well to GPi DBS cases - Similar to primary/isolated dystonia • Does not help other neurological signs – spasticity, dysarthria Sako W, Goto S, Shimazu H, et al. (N=5) Pre-Op 12 Months Post-Op Age at surgery: 13 yo male 9
Recommend
More recommend