D ISTRACTION O STEOGENESIS Shelby Marks, Kijeon Choi, Taylor Tebano, Stanley Gelin, and Sarah Bradner
L EARNING O BJECTIVES To understand the advancement of bone elongation techniques that lead to modern day practice. Be able to describe what distraction osteogenesis is and how it works. Identify and compare the different distraction osteogenetic surgical processes to achieve skeletal reconstruction. Understand the many causes/diseases for which distraction osteogenesis is used. Recognize the complications and risks associated with the process and identify post-operative care.
D ISTRACTION O STEOGENESIS Surgical reconstruction of skeletal deformities and lengthening of the long bones of the body Procedure that moves 2 bone segments apart using an external saw and allows new bone in gap Many FDA approved distraction devices
H ISTORY ‣ Skeletal traction was described as long ago as by Hippocrates (460-377 B.C.) when traction on long bones was performed by means of rubber straps ‣ Alessandro Codivilla (1861 -1912), Pioneer of bone elongation techniques ‣ Italian Surgeon ‣ Published 1905 case report of femoral extension using axial forces ‣ Introduced Limb lengthening techniques that had a high complication rate ‣ Popularized by Russian orthopedic surgeon Gavril Ilizarov
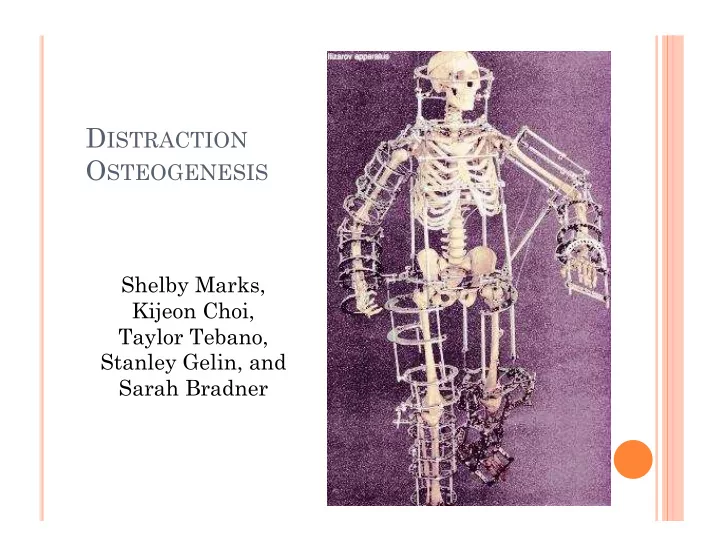
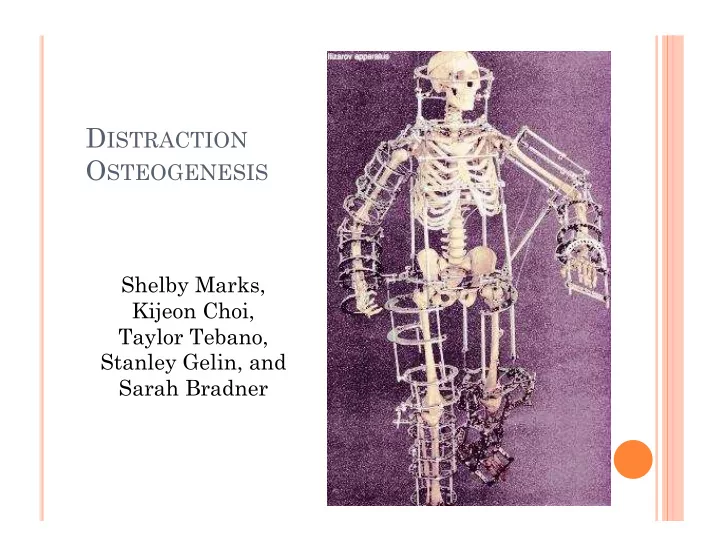
G AVRIL I LIZAROV – Gavriil Abramovich Ilizarov was born in Caucasus (former USSR) in 1921 – No formal schooling till age 11 – Lone physician in Kurgan, Serbia – Developed Ilizarov method – An external fixator to regenerate bone under tension – modular ring – Died July 24 1992 in Kurgan, Russia due to heart failure
R USSIAN ILIZAROV S CIENTIFIC C ENTER FOR R ESTORATIVE T RAUMATOLOGY AND O RTHOPAEDICS • Founded in 1971 in Kurgan, Serbia • Home to Ilizarov method • The first department in Russia for managing bone infection • Place where limb lengthening techniques were first devised and introduced into clinical practice.
H OW DOES IT WORK ? Must be gradual too quick : fibrous union instead of osseointegration too slow: early bone union Steps: Surgeon makes ostectomy (break) in abnormal bone 1) and places distraction device. Allowed to start a few days of healing. Parent/ guardian turns a screw on distractor after 2) surgery at home to stretch healing tissue (stretch~1mm/day) Stretch regenerated tissue forms into new bone 3) over next 2 months After bone is formed at necessary length, device is 4) removed through a 2 nd surgery
C ELLULAR LEVEL : Aka callus distraction Inflammation: formation of blood clot and ingrowth of angiogenic elements Soft callus: replacement of blood clot with granulation tissue and fibrocartilage Hard Callus: granulation and fibrocartilage is is replaced with woven bone Remodeling: woven bone is replaced with lamellar bone
T ECHNIQUES RIGID external device (RED) Frames surgery Intramedullary Nail -Albizzia -Guichet -FITbone -ISKD LRS
I. R IGID E XTERNAL D EVICE (RED) Found to give reliable results, control bone movements easy removal Cranial halo (semicircular piece) encircles front of patients forehead and secured with pins. Pins touch but do not penetrate bone. Cranial halo is attached to vertical graphite
E XTERNAL D EVICE Ex: Midface advancement - metal “halo” device and dental splint remain after operation during healing (10weeks) - 2 nd surgery removes halo & splint - caregiver turns twice a day - 1/8 th inch scar on lower eyelid but heals well
M IDFACE A DVANCEMENT Make cut in bones of face at specific points Loosen midface from rest of skull Advance into correct position New advantages: -bone grafts from rib and skull are no longer needed with plates and screws -larger advances in midface are achievable -skin and muscles are now stretched too and do not fight to push back -duration of procedure is shorter
II. F RAMES S URGERY “I LIZAROV S URGERY ” Oldest and most common method Application of circular frame or external fixator Most common 1) Ilizarov frame 2) Taylor Spatial frame
F RAME MAKE - UP Frames are circular external fixators that surround limb Consists of 4-6 rings made of stainless steel or carbon fiber Thin wires and half pins are fixed to rings and pass through skin to bone Half pins: attached on one side of frame Wires: other side through bone and attached and held under tension Rods and struts: between rings for stability and adjustment
I NTRAMEDULLARY NAIL
A LBIZZIA - D R . G UICHET 1987 Internal telescopic nail with lengthening mechanism Lengthening achieved by rotation Rotation makes “click” noise Click allows higher accuracy, patient knows how much they lengthened it 15 clicks~1 mm Fully implantable nail allows for full weight bearing 4 inch gain Small scar
G UICHET - ADVANCED A LBIZZIA (2009) Improved method Stronger steel makes it weight bearing No longer “one size fits all” Can accommodate different sized limbs
FIT BONE (F ULLY INTEGRATED TELESCOPIC BONE ) Nail is distraction device powered by internal engine Engine activated by hand remote Activates distraction by sending messages to receiver below skin
H OW DOES IT WORK ? Similar function as car antenna Fitbone elongation is propelled by gear Inserted through “model entrance point” Tiny scar
III. ISKD ( INTRAMEDULLARY S KELETAL K INETIC D ISTRACTOR ) Activated by polar movements through small rotation of bone segment being lengthened Amount of length is determined pre-op and set at time of insertion Allows 3’’ gain
IV. LRS ( LIMB RECONSTRUCTION SYSTEM ) Includes different clamps that slide on rigid rail and connected with distraction units Relies on callus distraction Stability by allowing different bone screw position in clamp along length of bone Rail length pick depending on size of limb Osteotite bone screws with hydroxyapetite coating
Distraction Osteogenesis for Congenital Deformities Types of Congenital Deformities: limb lengthening facial deformities amputation at the elbow correction of airway obstruction in micrognathia Fibular hemimelia Hemihypertrophy Ollier � s disease
L IMB L ENGTHENING Procedure: a bone segment is surgically cute and a distraction device is used to slowly pull the two ends apart. After the desired lengthening has been achieved, the bone consolidates until the lengthened gap has completely calcified. Distraction phase and Consolidation Phase in distraction osteogenesis. History: Discovered by Russian Orthopedic Gavril Ilizarov Technique: external fixator Today: minimally invasive techniques performed with internal distraction device
A MPUTATION AT THE ELBOW • Patients with short congenital amputations below the elbow often function as if they have had a disarticulation of the elbow • Patients had lengthening of stumps by the Ilizarov technique to improve fitting of prostheses
C ONGENITAL F ACIAL D EFORMITIES Hemifacial Microsomia: a rare congenital disease characterized by facial asymmetry Cleft palate: separation of the roof of the mouth that occurs in early development of fetus Severe mandibular hypoplasia (small lower jaw): causes breathing problems includes conditions as: Brachygnathia : abnormal shortness or recession of the lower jaw Micrognathia : an abnormally small, lower jaw and chin. Why?
Hemifacial Microsomia Distraction Process Bimaxillary distraction osteogenesis allows correction of mandibular asymmetry with simultaneous correction of the position of the maxilla Cleft Palate
C ORRECTION OF AIRWAY OBSTRUCTION Micrognathia Can use tracheostomy: May be life saving but is associated with complications and developmental problems Alternative: internal mandibular distraction osteogenesis
F ACIAL D EFORMITIES Treacher-Collins syndrome: a condition that affects the development of bones and other tissues in the face Pierre-Robin Sequence: a group of disorders occurring together that includes a small, lower jaw, breathing problems, and a tongue that tends to ball up at the back of the mouth Facial Injuries: cause damage to the maxilla or mandible most common condition for which distraction osteogenesis is performed
M AXILLOFACIAL D ISTRACTION O STEOGENESIS Two Main Uses: 1. Congenital Craniofacial Defects 2. Facial injuries from trauma/ impact Requires making bones longer
M AXILLOFACIAL DO P ROCESS Bonus Question : Why is it the hardest to grow bone in the face considering the current methods?
M AXILLOFACIAL DO Bone movements must be carefully planned before a device is implanted There are no devices that can change trajectory mid-course
M AXILLOFACIAL DO P ROCEDURES Current Methods: Future device goals External and linear Curvilinear devices (one dimension) (capable of moving bone in 3 dimensions) Move bone continuously, not in increments of 1mm Causes less pain, wouldn’t require patient compliance, might promote faster bone growth
D EVELOPMENTAL D EFORMITIES Clavicle Lengthening Reconstruction of forearm deformity Foot deformities Bow legs
Recommend
More recommend