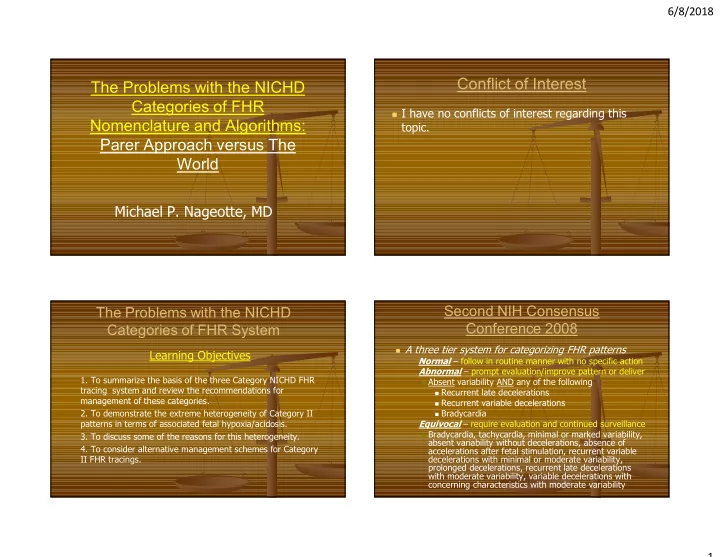
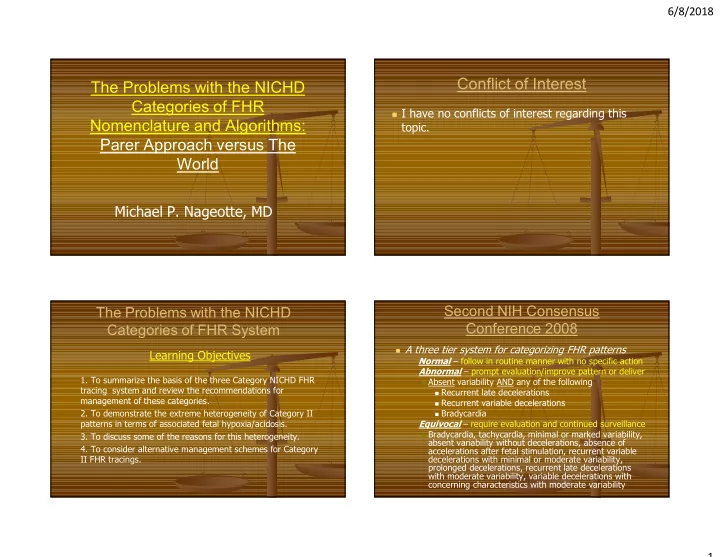
6/8/2018 Conflict of Interest The Problems with the NICHD Categories of FHR I have no conflicts of interest regarding this Nomenclature and Algorithms: topic. Parer Approach versus The World Michael P. Nageotte, MD Second NIH Consensus The Problems with the NICHD Conference 2008 Categories of FHR System A three tier system for categorizing FHR patterns Learning Objectives Normal – follow in routine manner with no specific action Abnormal – prompt evaluation/improve pattern or deliver 1. To summarize the basis of the three Category NICHD FHR Absent variability AND any of the following tracing system and review the recommendations for Recurrent late decelerations management of these categories. Recurrent variable decelerations 2. To demonstrate the extreme heterogeneity of Category II Bradycardia patterns in terms of associated fetal hypoxia/acidosis. Equivocal – require evaluation and continued surveillance Bradycardia, tachycardia, minimal or marked variability, 3. To discuss some of the reasons for this heterogeneity. absent variability without decelerations, absence of 4. To consider alternative management schemes for Category accelerations after fetal stimulation, recurrent variable II FHR tracings. decelerations with minimal or moderate variability, prolonged decelerations, recurrent late decelerations with moderate variability, variable decelerations with concerning characteristics with moderate variability 1
6/8/2018 The intention of EFM should be to avoid How were these categories established? serious acidosis rather than to ensure a strong correlation with it. Primarily they are based on the likelihood that a FHR pattern within a given category correlates with an increased or decreased risk of fetal metabolic acidosis The categorization was based on the likelihood of There are two basic concerns with this concept: predicting fetal metabolic acidosis Never have abnormal FHR patterns been prospectively blinded without clinical interventions to assess their true The goal of fetal monitoring is to have intervention correlation with specific neonatal outcomes before severe fetal acidosis results in cellular damage There is no knowledge of how often or how quickly different Category II patterns become Category III Ideally, in order to determine if a pattern or combination EFM is not a diagnostic test and has very poor specificity of patterns accurately predicts acidosis, one would need and positive predictive value. It is more like an exercise a prospective series of such patterns which were NOT ECG that identifies abnormal findings which may correlate INTERVENED upon. with bad outcomes allowing for intervention. The EFM questions we are asking: Question Is the fetus hypoxic? Within how many minutes should one be able to establish the category of FHR? 43% 44% Is there a metabolic acidosis? A. ten Is there a likelihood that the fetus is having B. twenty tissue or organ damage from asphyxia at this point in time? C. thirty 13% If we are unable to correct the suspected hypoxia and/or acidosis and we do not effect delivery, will the fetus die or become damaged n y y e t t n r before or subsequent to birth? t e i h w t t 2
6/8/2018 More than 40 combinations of FHR patterns qualify a Clinical Correlations with Acidosis? tracing as Category II Baseline rate Threshold for Metabolic Acidosis • Bradycardia not accompanied by absent variability Associated with Newborn Complications • Tachycardia Low et al:AJOG 1997; 177:1391 Baseline FHR variability • Minimal baseline variability Case-control study (gestational age and birth weight) • Absent variability unaccompanied by recurrent decelerations of base deficit in 233 term newborns (58 with BD <8, • Marked baseline variability 58 BD 8-12, 58 BD 12-16, 59 with BD >16 mmol/l) Accelerations Moderate or severe encephalopathy and respiratory • Absence of induced accelerations after fetal stimulation complications only associated with BD >12 mmol/l Periodic or episodic decelerations Moderate/severe encephalopathy: 10% with BD 12 – • Recurrent variables with minimal/moderate variability 16; however, 40% with BD >16 (<2% with BD <12) • Prolonged deceleration >2 minutes but <10 minutes Uncommon endpoint as BD 12-16 occurs in only 2% • Recurrent lates with moderate baseline variability of term newborns; BD>16 in only 0.5 % of term • Variable decelerations with other characteristics such as slow newborns (due to intervention for clinical indications) return to baseline, “overshoots”, nadir >60 bpm below baseline Frequency of Fetal Heart Rate Categories Ignores the issue that there is little likelihood of and Short-Term Neonatal Outcome hypoxia in the absence of decelerations Jackson, M; Holmgren, C.; Esplin, S.; Henry, E; Varner, M. Obstetrics & Gynecology: 2011: 118; 4; 803–808 Physiologically in labor, hypoxia does not occur in the absence of decelerations (late, variable or prolonged) Loss of variability is not caused by hypoxia alone but by Reviewed 48,444 tracings from ten hospitals neurologic depression at the more extreme end – usually Category II patterns were found in 40,758 with hypoxia and acidosis (84.1%) of tracings, and Category III In animal models of hypoxia, (confirmed by pulse oximetry in humans) decelerations always precede loss of variability patterns present in 54 (0.1%) of tracings So, isolated evolving patterns (excepting those that the patient arrives with where the preceding events are How can a categorization be useful if 84% unknown) such as tachycardia and minimal variability without decelerations are unlikely to be associated with of patients have equivocal tracings? acidosis 3
6/8/2018 Problems with Category II Management of FHR Tracings Practice Bulletin 116, Nov. 2010 Assumes that the goal of intervention is to wait until there is correlation with acidosis rather than to avoid serious acidosis. Over Acknowledges “diverse spectrum” of category II FHR patterns 80% of all patients have Category II tracings More than 40 combinations of fetal heart rate characteristics qualify a fetal heart rate pattern as Category II. Lumps patterns unlikely to be associated with hypoxia with those that are very likely to be associated with hypoxia Relies heavily on variability Ignores data from fetal pulse oximetry studies Ignores the issues of deceleration progression and duration; combinations of FHR patterns with severity of decelerations Ignores the low likelihood of hypoxia without decelerations Hospitals (nurses, doctors, and policies) are often equating Category II patterns with not requiring intervention Nothing in the algorithm mentions decelerations The 3 Tiered system relies heavily Variability Does NOT Reliably Rule In or Rule on variability Out Metabolic Acidosis Minimal or Absent Variability Does Not Rule To reach Category 3 one must have In Acidosis absent variability with late, variable or Sleep cycles prolonged decelerations/bradycardia Previous neurologic insult Drugs Infection Even with the proposed management Anomaly algorithm one needs to have absent or Genetic Disorder minimal variability with Category II Brain Tumor tracings to warrant intervention Trauma Toxins 4
6/8/2018 Abruption case Metabolic Acidosis and/or Patient presents at term with painful Neurologic Damage May Occur contractions and about 150 cc of bright red Without Absent FHR Variability vaginal bleeding which subsides just after admission. 5
6/8/2018 DELIVERY At 1506, NSVD of 2765 gm male Apgar scores 3/7/7 at one, five and ten Cord gases: Artery: 6.96/66/22/-14 Vein: 7.06/48/26/-10 Subsequent admission to NICU with neonatal encephalopathy and possible HIE Question The 3 Tiered system relies heavily on variability Two studies evaluated inter-observer interpretation of FHR When did this fetus/newborn suffer acidosis and Blackwell et al: 154 tracings, 3 MFM’s reviewed damaging asphyxia? Kappa agreement for various FHR parameters poor (0.81 to 0.16) 83% For the parameter of absent variability, Kappa was the poorest A. before admission to the hospital Moderate 0.69 B. during labor Minimal 0.51 Absent 0.16 C. during period of time off monitor Chauhan et al: 100 tracings, 5 clinicians reviewed before delivery 11% 5% Kappa for variability = poor (0.0 – 0.19) 1% Kappa for tachycardia = good (0.44-0.59) D. unable to determine r e . o n . . b . s . i a m . m o l h r g f e Hard to base a system on the one variable e n f o t h i e u r d t e o d m o t t t i n e o f l o b i s d a which is least agreed upon s n i o m i u r d e a p e g r n o i f r e u b d 6
Recommend
More recommend