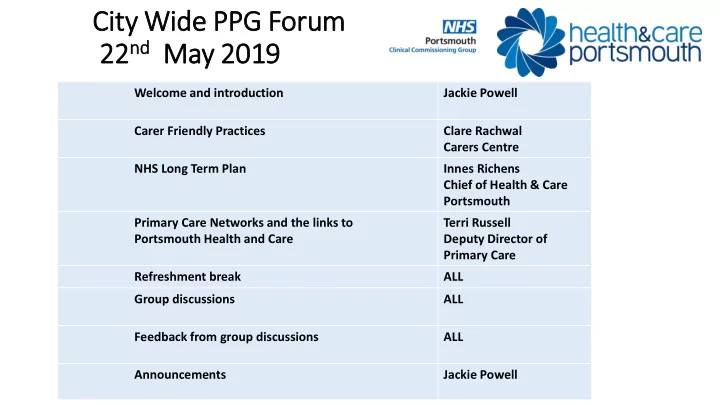
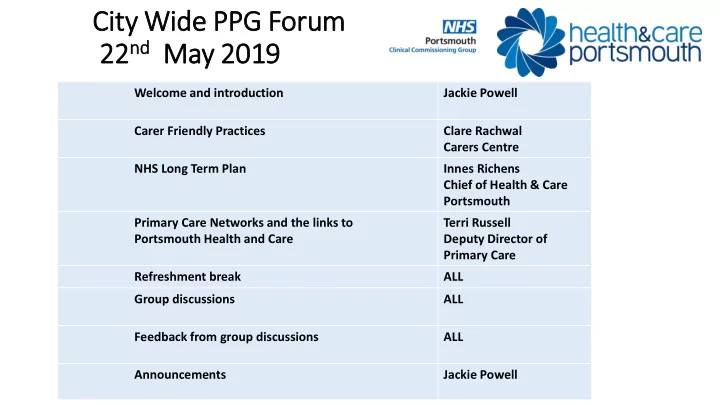
Cit ity Wid ide PPG Foru rum 22 nd nd 22 May 2019 Welcome and introduction Jackie Powell Carer Friendly Practices Clare Rachwal Carers Centre NHS Long Term Plan Innes Richens Chief of Health & Care Portsmouth Primary Care Networks and the links to Terri Russell Portsmouth Health and Care Deputy Director of Primary Care Refreshment break ALL Group discussions ALL Feedback from group discussions ALL Announcements Jackie Powell
Helping general practice become more carer-friendly: a framework of quality markers • Clare Rachwal – Team Manager, Carers Service • Adult Social Care • Clare.Rachwal@portsmouth.gov.uk
• Carers save health and social care an estimated £132 billion a year • GPs are often the first point of contact for carers • More than 90% of carers go unidentified by GPs • As a result carers can miss out on vital support including help for them to maintain their own health and wellbeing • 72% of carers suffer mental ill health as a result of caring • 61% of carers suffer physical ill health as a result of caring • Carers attribute their health risk to a lack of support, with 64% citing a lack of practical support
• Social Care Green Paper due… “NHS England…will work with the Care Quality Commission on the development of quality • NICE Adult Carers standards for carer-friendly GP practices, and is Guidelines due 2020 developing a framework of questions (quality markers) that can be used by doctors' surgeries to demonstrate how effective they are in recognising and supporting carers ” (p.10) "2.33. We will continue to identify and support carers, particularly "2.33. We will continue to identify and support carers, particularly those from vulnerable communities. Carers are twice as likely to those from vulnerable communities. Carers are twice as likely to suffer from poor health compared to the general population, primarily suffer from poor health compared to the general population, primarily due to a lack of information and support, finance concerns, stress due to a lack of information and support, finance concerns, stress and social isolation. Quality marks for carer-friendly GP practices, and social isolation. Quality marks for carer-friendly GP practices, developed with the Care Quality Commission (CQC), will help carers developed with the Care Quality Commission (CQC), will help carers identify GP services that can accommodate their needs. identify GP services that can accommodate their needs.
Quality Markers • Six questions that can be used by doctor’s surgeries to demonstrate how effective they are in recognising and supporting carers • The questions ask the general practice to show how they go about supporting carers for each of the six themes identified • Each question is supported by a number of practical ideas that general practices can put into place to help them develop the support they give to carers • The general practice completes an annual declaration as evidence of how it is supporting carers • This evidence can be used for CQC inspections
Support available • The Carers Centre in an Adult Social Care Service providing practical and emotional support to carers through a number of services and initiatives • The young carers team within Children's Services support children and young carers aged 5 up to 24 • Referrals are accepted via phone, post, e-mail and online. We can work with you set up direct referral processes • Carers can visit without appointment and request to see the duty worker For more information visit - https://www.portsmouth.gov.uk/ext/health-and- care/carers/portsmouth-carers-centre
The NHS Long Term Plan A Very Quick Overview
Quality & Outcomes Prevention • • • Smoking Air pollution Access standards for emergency mental health • • Diet Lack of exercise from 2020 • • High blood pressure Maternity and neonatal • • Children’s mental health Obesity • • Alcohol/drug use CQC emphasis on system-wide quality • Rapid Diagnostic Centres for cancer from 2019 NHS Long Term Plan New Service Models Digital Care • • Primary Care Networks Access to digital first primary care by 2022 • Online consultations for secondary care within • Social prescribing/ personal health budgets 5yrs • Same day emergency care & discharge in all • All trusts to digitise by 2024 hospitals • ICSs to have Chief Clinical Information Officer • Clinical assessment service as single point of by 2021 access • Investment in CT and MRI diagnostics
Enabling the NHS Long Term Plan Workforce Finance Structure • • • Regulation for NHS managers 3.4% growth over 5yrs Integrated Care Systems (ICS) • • • NHS leadership code Expectation of increased funding Integrated Care Providers (ICP) going to primary, community and • • More doctors encouraged to mental health Primary Care Networks (PCN) train as generalists • • Worst performing trusts subject Joint committees for NHS • Flexible rostering to be to accelerated turnaround England and NHS Improvement mandatory process • • New entry routes: Finance Recovery Fund for • apprenticeships, nursing associates, trusts with identifiable risks & online qualification, ‘earn & learn’ plans • £2.3m to support volunteers • NHS expected to save £700m from admin over 5yrs • £290m commissioners • £400m providers
The LTP and Health & Care Portsmouth • Strong alignment, particularly in our focus on primary and community (health) care: • Primary Care Alliance, clusters and Primary Care Networks • Co-located community health & social care teams • Integrated health & care delivery for: children, mental health, intermediate care, learning disabilities, substance misuse • Single digital care record for primary, community and adult social care • Long term conditions hub pilot • Connecting 111 and SCAS to single care record • NHS and Local Authority integrated commissioning
Integrated Care Systems • ICSs to cover whole of England by April 2021 • will ‘grow out of’ the current STPs • ICS brings commissioners and providers together to make shared decisions on resource use, service design and population health • ‘Streamlined’ set of commissioning arrangements: ‘typically an ICS will involve a single CCG for its area’ • CCGs: ‘leaner, more strategic organisations that support providers to partner with local government/community organisations for population health, service design and Plan implementation’
Features of Integrated Care Systems • Partnership Board • Non Executive Chair • Arrangements to involve NEDs and Governing Bodies • Clinician & management capacity from partners • Primary care representation via Clinical Director of ‘each Primary Care Network’ • CQC involvement • All providers to contribute to ICS performance goals (duty to collaborate) • Clinical leadership via alignment of clinical networks
Working with Local Government • Integration with local government is throughout the LTP • ‘continue to support local approaches to blending health & social care budgets where councils and CCGs agree this makes sense’ • Four models highlighted • Pooling of budgets • Individual service user pooled budgets • NHS oversees defined Local Authority budgets • Local Authority Chief Executive Officer or Director of Adult Social Services is CCG Accountable Officer • ‘ICSs and Health & Wellbeing Boards will also work closely together’
Social Care • LTP assumes the government commitment to ensure adult social care funding is at a level that does not impose additional pressure on the NHS • Social care green paper ‘forthcoming’
Integrated Care Providers • Community NHS services to be configured on the same basis as new primary care network footprints • Multi-disciplinary teams to operate in same footprints • GPs, pharmacists, district nurses, community geriatricians, dementia workers, allied health professionals • Social care and voluntary sector should join these arrangements • New Integrated Care Provider contract available from spring 2019 • which will allow for primary medical services integration with other services. • An ICP contract will be held by 'public statutory providers'
Primary Care Networks (PCNs) • PCNs are ‘based on neighbouring GP practices that work together typically covering 30- 50,000 people’ • GP contract changes will allow GP practices in a local area to enter into a ‘network contract’ which is an extension to their current contract • Funds will be designated to ‘flow’ through these new network contracts • CCG enhanced services contracts to be part of network contract
Recommend
More recommend