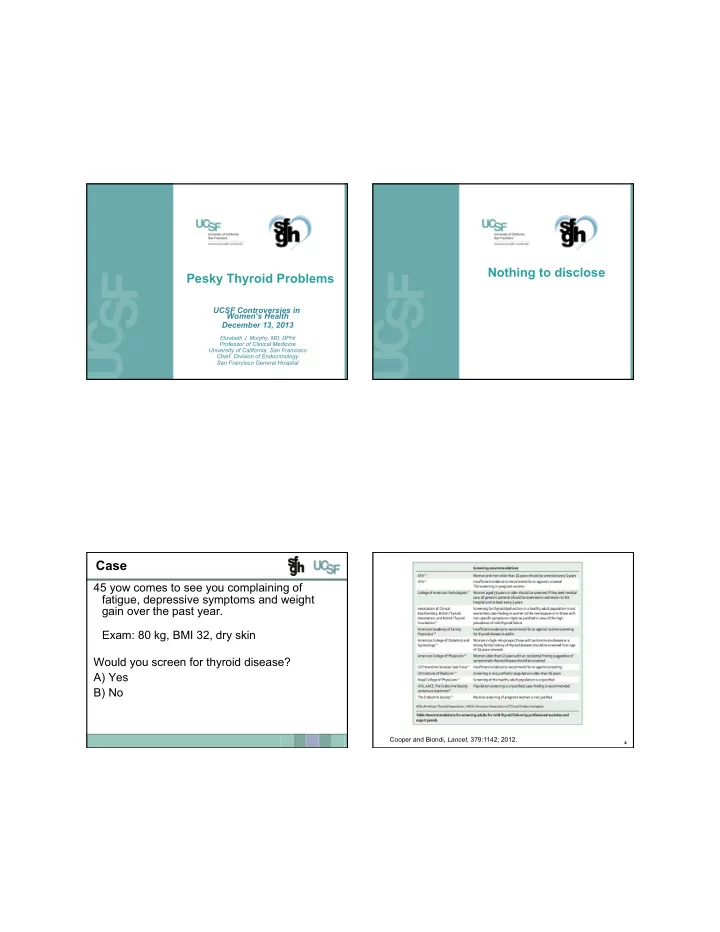
Nothing to disclose Pesky Thyroid Problems UCSF Controversies in Women’s Health December 13, 2013 Elizabeth J. Murphy, MD, DPhil Professor of Clinical Medicine University of California, San Francisco Chief, Division of Endocrinology San Francisco General Hospital Case 45 yow comes to see you complaining of fatigue, depressive symptoms and weight gain over the past year. Exam: 80 kg, BMI 32, dry skin Would you screen for thyroid disease? A) Yes B) No Cooper and Biondi, Lancet , 379:1142; 2012. 4
Case for Routine Screening Screening for Thyroid Disease • If you do check a TSH and it’s completely normal, 65 yow followed in endocrine for primary there is no need to recheck for 5 years unless there hyperparathryoidism and DM2. is a clinical change Date TSH • “ Screening” is recommended for 6/2002 1.30 10/2004 1.37 Newborns • 11/2005 1.31 DM1, Down Syndrome, Turner’s Syndrome, • Addision’s disease 12/2006 1.63 5/2007 1.78 Amiodarone, lithium • 5/2008 1.65 New onset a.fib. • 2/2009 1.37 History of neck irradiation • 7/2009 1.16 • Consider screening prior to pregnancy 5/2010 1.12 3/2011 1.55 9/2011 1.17 5 6 Case Factors Altering TSH 45 yow comes to see you complaining of • Diurnal variation (nocturnal surge resulting in fatigue, depressive symptoms and weight highest values in the morning and lower values in gain over the past year. the afternoon) • Non-thyroidal illness Exam: 80 kg, BMI 32, dry skin • Assay Issues o Heterophile antibodies TSH 8.9 H (0.45-4.20) o HAMA antibodies What now? o Assay variability a) Treat with levothyroxine b) Order thyroid peroxidase antibody (TPO) c) Recheck a TSH d) Recheck a TSH and Free T4 7 8
Case Case 45 yow comes to see you complaining of fatigue, 45 yow comes to see you complaining of depressive symptoms and weight gain over the past fatigue, depressive symptoms and weight year. gain over the past year. Exam: 80 kg, BMI 32, dry skin Exam: 80 kg, BMI 32, dry skin Thyroid: firm, normal size TSH 8.9 H (0.45-4.20) TSH 9.2 H (0.45-4.20) • TSH 8.9 H (0.45-4.20) FT4 1.1 (0.65-1.78) • TSH 12 H (0.45-4.20) FT4 0.63 L (0.65-1.78) Subclinical Hypothyroidism Hypothyroid - Treat 9 10 Case Relationship of TSH to Free T4 45 yow comes to see you complaining of fatigue, depressive symptoms and weight gain over the past year. Exam: 80 kg, BMI 32, dry skin Thyroid: firm, normal size TSH 8.9 H (0.45-4.20) TSH 9.2 H (0.45-4.20) FT4 1.1 (0.65-1.78) – Normal for the population A given individual will have a narrower normal range. Quest Diagnostics, D. Fisher, J. Nelson 11 12
Case Subclinical Hypothyroidism 45 yow comes to see you complaining of fatigue, • Prevalence in US depressive symptoms and weight gain over the past o 4.3% NHANES III year. o 9.5% Colorado Mall Study Exam: 80 kg, BMI 32, dry skin • Prevalence Thyroid: firm, normal size TSH 8.9 H (0.45-4.20) o Increased in iodine sufficient areas TSH 9.2 H (0.45-4.20) FT4 1.1 (0.65-1.78) o Increases with age What now? o Increased in women a) Treat with levothyroxine b) Order thyroid peroxidase antibody (TPO), treat if o Decreased in African Americans positive • Only 25% of people with subclinical c) Recheck a TSH in 6 months d) Recheck a TSH and Free T4 in 6 months hypothryoidism have TSH > 10 13 14 Subclinical Hypothyroidism Race and Ethnicity Specific TSH Distributions – NHANES III Deciding When to Treat • There is no clear right or wrong answer • Consensus Statement 2004 1 Routine treatment for TSH 4.5-10 mIU/L is not warranted as there is no evidence of benefit. Treat for TSH > 10 mIU/L. • Subsequently societies took issue with this recommendation as lack of evidence is not the same as evidence against • There is no clear right or wrong answer 1 JAMA 2004; 291:228-238 Hollowell J G et al. JCEM 2002;87:489-499 15 16
Subclinical Hypothyroidism Progression to Hypothyroidism Deciding When to Treat • Reasons to treat Increased likelihood for the development of overt o Prevent progression to frank hypothyroidism hypothyroidism : o Improve symptoms o Female, older, TPO antibody positive, higher TSH Approximately 2.5% of antibody negative individuals per o Improve lipids year progress to overt hypothryoidism and 4.5% of TPO o Pregnant/considering pregnancy antibody positive individuals o Associated with increased mortality and/or morbidity Women with +TPO antibodies have a 38 fold increased • Reasons not to treat risk of developing hypothyroidism o Treatment has not yet been shown to improve TSH normalizes in about 5% of individuals at one year mortality in a prospective trial Almost half of patients with subclinical hypothyroidism o Expense (43%) will have progressed in 10 years o Could do harm Tunbridge et al., Clinical Endocrinology 7:481, 1977; Vanderpump et al., Clinical Endocrinology 17 43:55, 1995; Walsh et al., JCEM 95:1095, 2010 18 Subclinical Hypothyroidism Progression to Hypothyroidism Deciding When to Treat • Reasons to treat Increased likelihood for the development of overt o Prevent progression to frank hypothyroidism hypothyroidism : o Improve symptoms o Female, older, TPO antibody positive, higher TSH o Improve lipids Approximately 2.5% of antibody negative individuals per o Pregnant/considering pregnancy year progress to overt hypothryoidism and 4.5% of TPO antibody positive individuals o Associated with increased mortality and/or morbidity • Reasons not to treat Women with +TPO antibodies have a 38 fold increased risk of developing hypothyroidism o Treatment has not yet been shown to improve mortality in a prospective trial TSH normalizes in about 5% of individuals at one year o Expense The majority of patients with subclinical hypothyroidism o Could do harm (57%) will not have progressed in 10 years Tunbridge et al., Clinical Endocrinology 7:481, 1977; Vanderpump et al., Clinical Endocrinology 19 20 43:55, 1995; Walsh et al., JCEM 95:1095, 2010
Subclinical Hypothyroidism Subclinical Hypothyroidism Deciding When to Treat Deciding When to Treat • Reasons to treat • Reasons to treat o Prevent progression to frank hypothyroidism o Prevent progression to frank hypothyroidism o Improve symptoms o Improve symptoms o Improve lipids o Improve lipids o Pregnant/considering pregnancy o Pregnant/considering pregnancy o Associated with increased mortality and/or morbidity o Associated with increased mortality and/or morbidity • Reasons not to treat • Reasons not to treat o Treatment has not yet been shown to improve mortality o Treatment has not yet been shown to improve mortality in a prospective trial in a prospective trial o Expense o Expense o Could do harm o Could do harm 21 22 Recommendations For Thyroid Screening in Endo Society High Risk Pregnancy The Endocrine Society 2012 • Universal screening of healthy women before pregnancy is not recommended (USPSTF I, evidence poor ) • Screen high risk women (I, evidence poor) JCEM 97:2543, 2012 23 24
Recommendations For Thyroid Screening Maternal Thyroid and Kid IQ in Pregnancy The Endocrine Society 2012 • Universal screening of healthy women before pregnancy is • Studied children not recommended (USPSTF I, evidence poor ) of women with • Screen high risk women (I, evidence poor) undiagnosed • Newly pregnant women hypothryoidism o Screen all pregnant women by week 9 or at time of first visit (TSH 13) 1 (C, evidence fair) o Don’t know, so only do high risk unless that’s too hard and then do everyone (I, evidence poor) Offspring IQ Age 7 Haddow et al, NEJM , 341:549; 1999. JCEM 97:2543, 2012 25 26 Maternal Thyroid and Kid IQ SHEP Study Antenatal screening at 12w3d gestation • Subclinical Hypothryoid and Iodine • 21,800 women screened (390 rx, 404 control) Deficiency in Early Pregnancy and Women o Planning for Pregnancy: Screening and TSH 3-4 o Treatment for hypothryoidism didn’t improve cognitive Intervention Trial o function at age 3 1 • Screening 21,5000 women and treat 4,800 Study Flaws • • Treat pre-pregnancy Fetal thyroid develops at wk 12 o Median TSH 3.8/3.1 o Half of those enrolled were enrolled for a low FT4 alone o Age 3 might be to early to study o Doesn’t provide useful data for prepregnancy • screening 1 Lazarus et al, NEJM , 366:493; 2012. 27 28
Recommend
More recommend