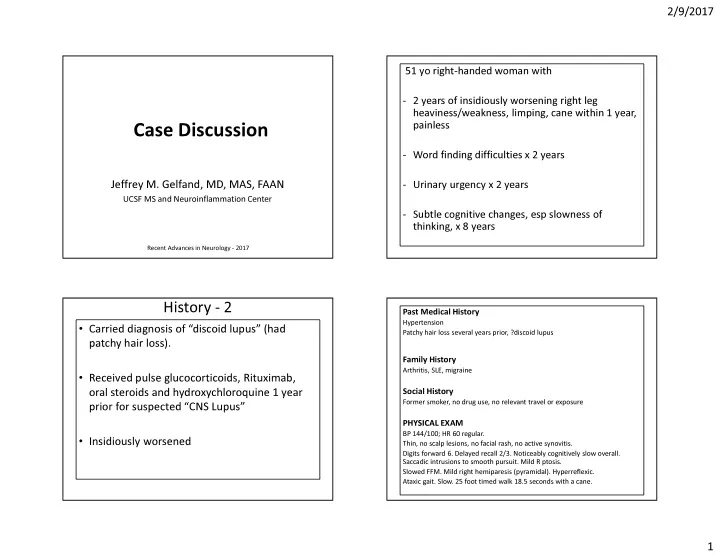
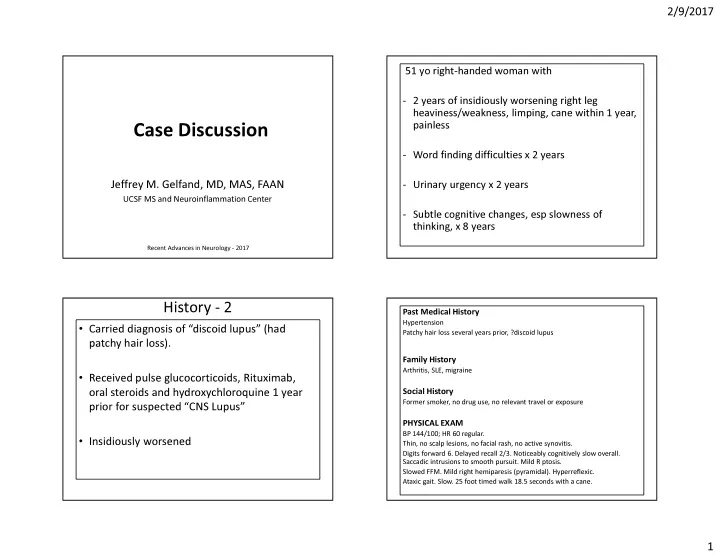
2/9/2017 51 yo right-handed woman with - 2 years of insidiously worsening right leg heaviness/weakness, limping, cane within 1 year, painless Case Discussion - Word finding difficulties x 2 years Jeffrey M. Gelfand, MD, MAS, FAAN - Urinary urgency x 2 years UCSF MS and Neuroinflammation Center - Subtle cognitive changes, esp slowness of thinking, x 8 years Recent Advances in Neurology - 2017 History - 2 Past Medical History Hypertension • Carried diagnosis of “discoid lupus” (had Patchy hair loss several years prior, ?discoid lupus patchy hair loss). Family History Arthritis, SLE, migraine • Received pulse glucocorticoids, Rituximab, Social History oral steroids and hydroxychloroquine 1 year Former smoker, no drug use, no relevant travel or exposure prior for suspected “CNS Lupus” PHYSICAL EXAM BP 144/100; HR 60 regular. • Insidiously worsened Thin, no scalp lesions, no facial rash, no active synovitis. Digits forward 6. Delayed recall 2/3. Noticeably cognitively slow overall. Saccadic intrusions to smooth pursuit. Mild R ptosis. Slowed FFM. Mild right hemiparesis (pyramidal). Hyperreflexic. Ataxic gait. Slow. 25 foot timed walk 18.5 seconds with a cane. 1
2/9/2017 - Bilateral supratentorial FLAIR hyperintensities. - Numerous foci of reduced diffusion in the bifrontal periventricular MRI 1 and deep white matter year after - No abnormal the above enhancement - MRA brain normal - MRI Spine with mild DJD, no cord lesions ADC DWI Diagnostics LABS + ANA, + RNP, +Smith antibodies. PLT 138. SPEP with polyclonal gammopathy. Negative or normal: DS-DNA, Smith. SSA/SSB, RF, SCL-70, Jo-1, Histone, ESR, complements, CK, ACE, HIV, Lyme, TSH, TPO, UA. A Diagnostic Test was CSF Performed… Opening Pressure: 16 cm 0 WBC, 1 RBC, protein 33, glucose 59 (serum 81) IgG index 0.48; Matched bands in CSF and serum VDRL NR EMG-NCS: Mild right axonal peroneal neuropathy that does not explain her right leg weakness 2
2/9/2017 CSF1R – Adult Onset Leukodystrophy with Whole Exome Sequencing Spheroids and Pigmented Glia (ASLP) - Syndrome described 1984; CSF1 receptor mutations recognized 2012; Autosomal dominant • CSF1R mutation : Novel non- - Encompasses two pathological conditions: hereditary diffuse leukoencephalopathy with neuroaxonal spheroids (HDLS) and familial conservative amino acid substitution L817Q in pigmentary orthochromatic leukodystrophy (POLD). exon 19 in the CSF1R gene. All pathogenic mutations to date have been reported in this • CSF1R primarily expressed on microglia, lesser on neurons – increasingly tyrosine kinase residue. Considered to be viewed as a “microglial-opathy” + axon loss pathogenic and diagnostic. • Median age of onset 42 (range 18-60 yrs in larger series). Relatively rapid neurological progression (cognitive, motor, gait) to death (e.g. Guerreiro, JAMA Neuro , 2013; Konno, Neurology , 2014) • Allo-HSCT may slow progression, possibly by chimerism of wild type CSF1R from monocytes – can HSCs can replace microglia when injured? (Eichler, et. al. Brain 2016) Clinical Pearls • Leukoencephalopathy plus persistent foci of reduced diffusion can be a helpful radiographic clue for CSF1R diagnosis. • This condition, which may account for ~10% of adult onset leukodystrophies, can be mistaken for MS or other vasculopathies • Prompt use of whole exome sequencing to confirm a genetic cause of adult-onset leukodystrophy can accelerate diagnosis, spare brain biopsy and allow for timely treatment • Exome sequencing is a complex process in which every variant cannot possibly be examined in detail -- missense mutations are most likely to be missed. Meticulous phenotyping can nominate specific genes (i.e. CSF1R) for closer scrutiny and increase diagnostic yield. MRI 8 months later: Interval bifrontal diffusion restriction. Unchanged bilateral supratentorial white matter volume loss and thinning of the callosal body. Referred for allo-HSCT 3
Recommend
More recommend