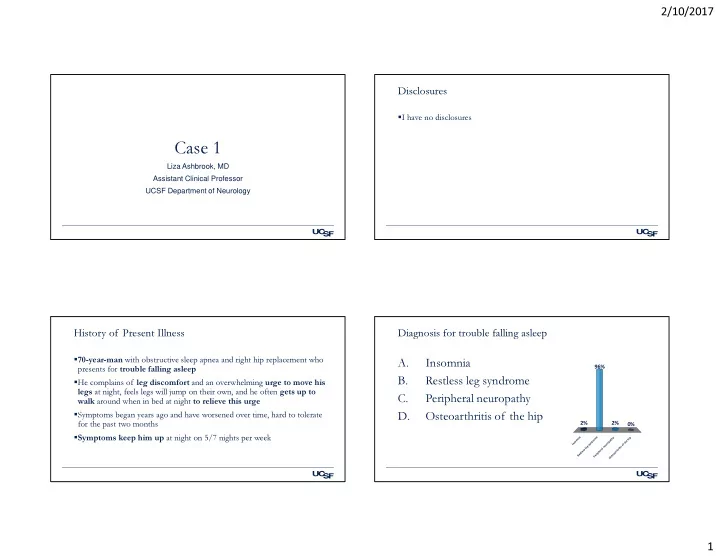
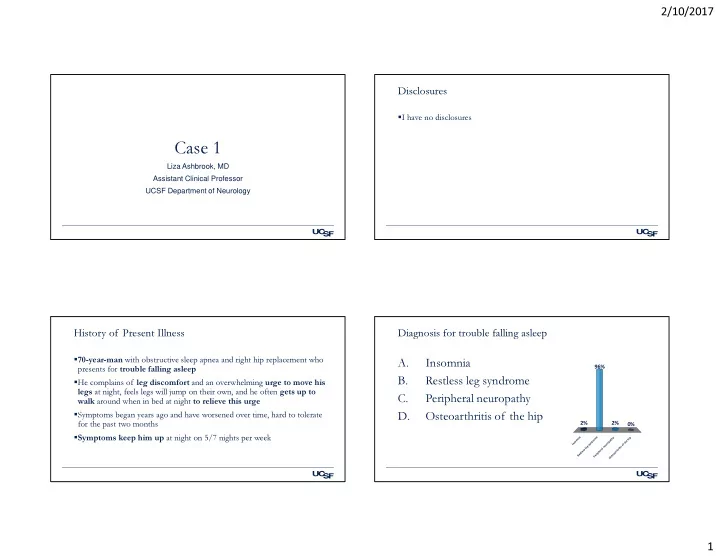
2/10/2017 Disclosures � I have no disclosures Case 1 Liza Ashbrook, MD Assistant Clinical Professor UCSF Department of Neurology History of Present Illness Diagnosis for trouble falling asleep � 70-year-man with obstructive sleep apnea and right hip replacement who A. Insomnia 96% presents for trouble falling asleep B. Restless leg syndrome � He complains of leg discomfort and an overwhelming urge to move his legs at night, feels legs will jump on their own, and he often gets up to C. Peripheral neuropathy walk around when in bed at night to relieve this urge � Symptoms began years ago and have worsened over time, hard to tolerate D. Osteoarthritis of the hip for the past two months 2% 2% 0% � Symptoms keep him up at night on 5/7 nights per week a e y p n i m h h i m o a t r e o d p h s n o t n y r I s u o f e g n s e i l l i t s a r s r h e e t l h r t p a s i o e r e R e t P s O 1
2/10/2017 Diagnosis of restless leg syndrome Additional history � Also called Willis-Ekbom disease (WEB) PMH: Obstructive sleep apnea (OSA), hypertension, hyperlipidemia, degenerative joint disease � Criteria: • An urge to move the legs, often triggered by unpleasant sensation Medications: pramipexole 0.25 mg nightly, tramadol 50 mg prn, hydrocodone/acetaminophen 5/325 prn, diphenhydramine prn • Begins/worsens during inactivity Physical Exam: No hip pain, intact strength and sensation in legs • Urge relieved, at least in part, by movement • Worse during the evening • Symptoms cause distress or impairment ** rule out other etiologies including myalgias, venous stasis, edema, cramping, position, habitual foot tapping What would you choose as initial nightly treatment? What would you choose as initial nightly treatment? A. Pregabalin (Lyrica) 75 mg A. Pregabalin (Lyrica) 75 mg 43% B. Pramipexole (Mirapex) 0.5 mg B. Pramipexole (Mirapex) 0.5 mg 36% C. Carbidopa/levodopa (Sinemet) 25/100 C. Carbidopa/levodopa (Sinemet) 25/100 D. Ropinirole (Requip) 0.25 mg D. Ropinirole (Requip) 0.25 mg 12% 6% 4% E. Clonazepam (Klonopin) 0.5 mg E. Clonazepam (Klonopin) 0.5 mg g g g g m . m e . m m 5 5 m 5 5 . 2 . 7 0 e 0 n 0 . a ) ) i ) c x S ) n i e ( p i r p a i p y a u o L p q n ( i r o n M d e o R l l i ( o ( K a v ( b e e e m o l l l a / o a g x a r e e p n i p r p e P i o p i z m d a i o n a b R r r o P a l C C 2
2/10/2017 Dopamine agonists vs Alpha-2-delta ligands: NEJM 2014 Recommended dosing “Comparison of Pregabalin with Pramipexole for Restless Legs Syndrome” (sponsored by Pfizer) � 719 participants Starting Dose Maximum recommended dose Dopamine Agonists � IRLS severity at 12 weeks vs placebo Pramipexole (Mirapex) 0.125mg 0.75mg • pramipexole 0.5 mg (<0.001) Ropinirole (Requip) 0.25mg 4mg • pregabalin 300 mg (<0.001) Rotigotine (Neupro) 1mg/day 3mg/day • not pramipexole 0.25 mg (0.36) Alpha-2 Delta Ligands Starting Dose Maximum recommended dose � At 52 weeks: More augmentation with pramipexole • Pregabalin 300 mg 5/235 (2.1%) Pregabalin (Lyrica) 50-75mg 150-450mg • Pramipexole 0.25 mg 12/225 (5.3%, P=0.08) Gabapentin (Neurontin) 100-300mg 900-2400mg • Pramipexole 0.5 mg 18/235 (7.7%, P=0.001) Gabapentin enacarbil (Horizant) 300-600mg 600-1200mg Allen RP et al. NEJM, 2014 D. Garcia-Borreguero et al. / Sleep Medicine 21 (2016) 1–11 Additional history Characteristics of augmentation • He has noted leg discomfort on airplane rides for many years but did not � RLS symptoms seek care • start earlier in the day (two hours used as cut off) • In 2011 periodic leg movements were noted in a sleep study, he was • more severe questioned about restless leg symptoms and was started on pramipexole 0.25mg (note recommended starting dose is 0.125 mg), this helped for • faster onset of symptoms following rest several years • affect other parts of the body (arms) • In 2014 symptoms returned and pramipexole dose increased from 0.25 • shorted duration of medication efficacy and/or mg to 0.5 mg to 1 mg (maximum recommended dose is 0.75 mg) • paradoxical response to treatment • The time of onset and intensity of his symptoms worsened: starting 5-6 pm, now include arm symptoms, more severe 3
2/10/2017 Management of augmentation: step 1 Management of augmentation: Step 2 1. If mild, consider keeping the same medication � Check serum iron: Serum ferritin goal >50-75 ng/mL a) move the timing earlier � Screen for other triggers such as b) split the dose to two times • exacerbating medications including dopamine antagonists, c) increase the dose if still below maximum recommended dose (do antihistamines, antidepressants (except bupropion) only once) • sleep deprivation or sleep disruptor (OSA) 2. Change medications to long acting DA agonist (rotigotine) or alpha-2- • Medical conditions such as renal insufficiency or pregnancy delta ligand • alcohol use a) Switch medications • decreased mobility b) Cross titration c) Wash out period After 2.5 months of inadequately treated symptoms despite trial of gabapentin, Our patient – further clinical course gabapentin enacarbil, iron supplementation, stopping pramipexole, tramadol, and diphenhydramine and prescription of rotigotine patch � Reduced pramipexole to 0.5 then 0.25, but was increasingly using What would you do next? tramadol and hydrocodone/acetaminophen from hip surgery 71% � Ferritin 71.2, iron tabs did not help A. Push for trial of rotigotine patch (Neupro) � Cross taper: gabapentin 300mg ->600mg with wean of pramipexole B. Pregabalin 75 mg with plan to increase to 150 � Timing did improve, but symptoms still very bothersome in legs and arms C. Intravenous iron infusion � Rotigotine patch prescribed, patient did not want to pursue DA agonist 13% 13% D. Methadone 5 mg � Changed to gabapentin enacarbil (Horizant) without improvement 4% � Told stop taking diphenhydramine prn Methadone 5 mg Pregabalin 75 mg with plan t... Intravenous iron infusion Push for trial of rotigotine p... � Still taking 2 hydrocodone/acetaminophen nightly to control symptoms 4
2/10/2017 Our patient Management of refractory RLS � He has no personal history of substance abuse � Around the clock symptoms � Methadone 5mg started � DA agonist and alpha-2 delta ligand do not work � Provided great relief and patient reported urge to move the legs resolved � Consider opioids • Low dose oxycodone • Methadone **Screen for history of substance abuse, use of other sedating medications Opioids for RLS Opioids for RLS � 10 year longitudinal study (Silver et al. Sleep Medicine, 2011) � RCT of long acting oxycodone/naloxone 5mg/2.5mg (Trenkwalder et al. Lancet Neurol 2013, study funded by Mundipharma Research) • Subjects: 164 patients on pramipexole, 77 patients on pergolide, and 76 • Subjects: 132 to prolonged release oxycodone/naloxone vs 144 to patients on methadone. placebo • First year discontinuation (side effects): pramipexole 17%, pergolide 23%, • At 12 weeks of treatment mean IRLS rating scale drop on methadone 15% oxycodone/naloxone: 16.5 vs placebo: 9.4 (p<0·0001) • Annual discontinuation rate over 5 years: pramipexole 9% , pergolide 8%, methadone 0% • Methadone dose: Median dose at six months: 10mg, median daily dose � Before using ensure risk of abuse is low by screening for a history of after 8–10 years no more than 10 mg greater than at 6 months substance abuse 5
2/10/2017 A note about supplemental iron Take home points � Data mixed slow but can be very effective for some patients RLS Pitfalls � PO iron: • Starting medication when not needed or prn dosing would be enough • 325 mg of ferrous sulfate BID, combine with vitamin C • Starting higher dose than needed to control symptoms � IV iron: (Cho Y et al. Sleep Med 2013) • Escalating DA agonist dose despite worsening symptoms • Low-molecular weight iron dextran 250mg weekly x 4 (total dose of 1 g) • Missing iron deficiency Side effects: allergic reaction headache, nausea, muscle pain, edema • Missing exacerbating medications that can be safely discontinued • One and six weeks after treatment and the treatment benefits lasted from one month to 22 months. For severe RLS symptoms • NOTE parenteral infusion risk with low molecular weight iron dextran is lower (1 per 200,000) than • Consider supplemental intravenous iron that with high molecular weight iron dextran. Other formulations also available. • Consider long acting, low dose opioid Patient history � 20-year-old woman with a history of chronic refractory migraine and hip pain who presents for trouble falling asleep and staying asleep for 1.5 years Sleep/wake pattern: Case 2 � Bedtime: 10 pm, sleep latency: 6 hours, wake time: 5 pm � When awake in bed at night watches television, colors, talks on the phone � Awakenings from sleep: 6-7 times with frequent trouble falling asleep � Ideal (dessert island) bedtime: 2 am; Goal sleep schedule: 11:30 pm-7:30 am � Never feels well rested, endorses daytime sleepiness � Snores sometimes, no gasping, choking, witnessed pauses 6
Recommend
More recommend