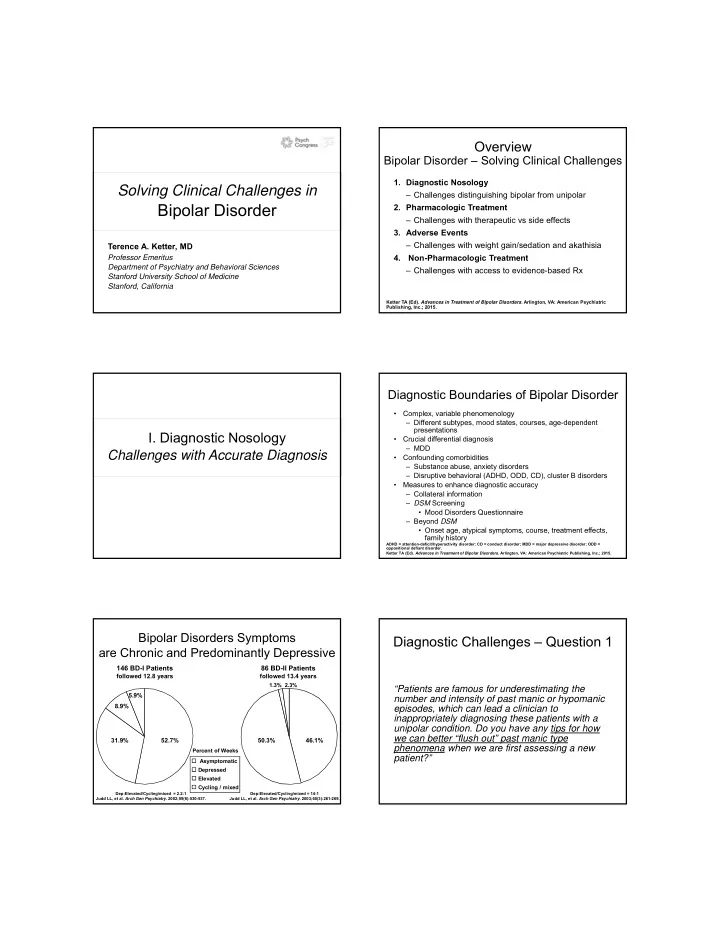
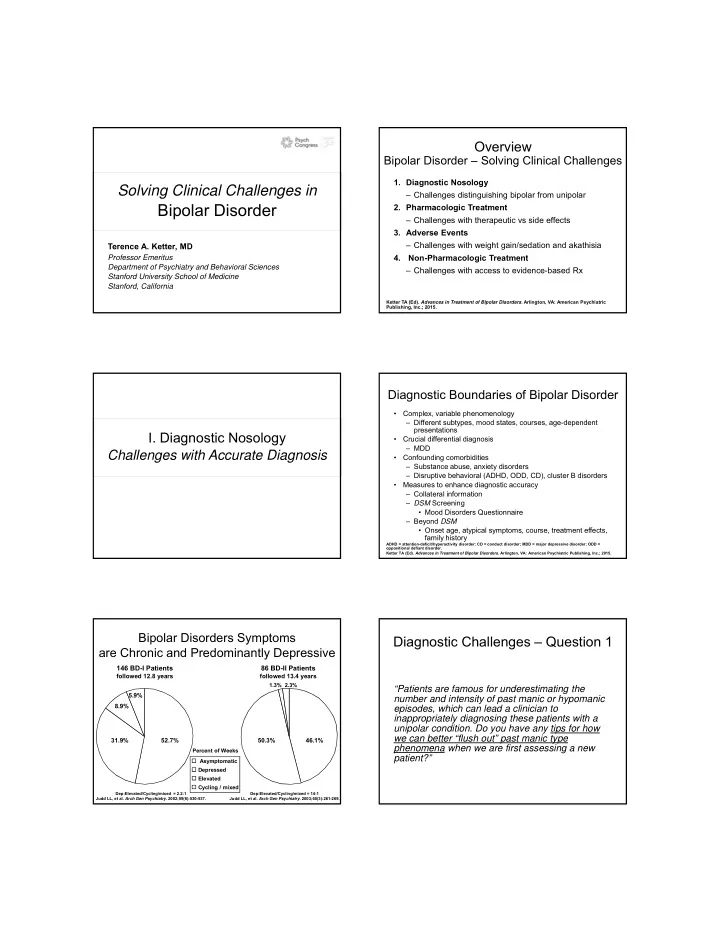
Overview Bipolar Disorder – Solving Clinical Challenges 1. Diagnostic Nosology Solving Clinical Challenges in – Challenges distinguishing bipolar from unipolar Bipolar Disorder 2. Pharmacologic Treatment – Challenges with therapeutic vs side effects 3. Adverse Events – Challenges with weight gain/sedation and akathisia Terence A. Ketter, MD 4. Non-Pharmacologic Treatment Professor Emeritus Department of Psychiatry and Behavioral Sciences – Challenges with access to evidence-based Rx Stanford University School of Medicine Stanford, California Ketter TA (Ed). Advances in Treatment of Bipolar Disorders . Arlington, VA: American Psychiatric Publishing, Inc.; 2015. Diagnostic Boundaries of Bipolar Disorder • Complex, variable phenomenology – Different subtypes, mood states, courses, age-dependent presentations I. Diagnostic Nosology • Crucial differential diagnosis – MDD Challenges with Accurate Diagnosis • Confounding comorbidities – Substance abuse, anxiety disorders – Disruptive behavioral (ADHD, ODD, CD), cluster B disorders • Measures to enhance diagnostic accuracy – Collateral information – DSM Screening • Mood Disorders Questionnaire – Beyond DSM • Onset age, atypical symptoms, course, treatment effects, family history ADHD = attention-deficit/hyperactivity disorder; CD = conduct disorder; MDD = major depressive disorder; ODD = oppositional defiant disorder. Ketter TA (Ed). Advances in Treatment of Bipolar Disorders . Arlington, VA: American Psychiatric Publishing, Inc.; 2015. Bipolar Disorders Symptoms Diagnostic Challenges – Question 1 are Chronic and Predominantly Depressive 146 BD-I Patients 86 BD-II Patients followed 12.8 years followed 13.4 years 1.3% 2.3% “Patients are famous for underestimating the 5.9% number and intensity of past manic or hypomanic 8.9% episodes, which can lead a clinician to inappropriately diagnosing these patients with a unipolar condition. Do you have any tips for how we can better “flush out” past manic type 31.9% 52.7% 50.3% 46.1% phenomena when we are first assessing a new Percent of Weeks patient?” Asymptomatic Depressed Elevated Cycling / mixed Dep:Elevated/Cycling/mixed = 2.2:1 Dep:Elevated/Cycling/mixed = 14:1 Judd LL, et al. Arch Gen Psychiatry . 2002;59(6):530-537. Judd LL, et al. Arch Gen Psychiatry . 2003;60(3):261-269.
Substance/Medication-Induced Diagnostic Challenges I Bipolar and Related Disorder • Patients present with depression more than mood elevation • Get collateral history from significant other (more • Prominent, persistent elevated/irritable/expansive and/or depressed mood/anhedonia sensitive rater of mood elevation) • Look for mood elevation symptoms • During/soon after substance intoxication/withdrawal or medication exposure – Immediately before or after depressions • Substance/medication capable of producing above mood – Triggered by pharmacotherapy symptoms – Mixed depressions • Not better explained by non-substance induced bipolar • In depressed patients, assess bipolar outcome risk disorder factors – eg, Symptoms persist < 1 month without – Depression onset prior to age 25; lifetime history of psychosis, substance/medication 1° relative with mania – Presence of 1 risk factor doesn’t substantively increase bipolar • Not merely delirium outcome risk (which is approximately 25% overall) • Distress, social/occupational impact – In contrast, 2 or 3 risk factors substantively increase bipolar outcome risk (to approximately 50% and 67%, respectively) American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA: American Psychiatric Association; 2013. Ketter TA (Ed). Advances in Treatment of Bipolar Disorders . Arlington, VA: American Psychiatric Publishing, Inc.; 2015. Antidepressant-Induced Mania More Common in Antidepressant Treatment-Emergent Bipolar II Compared to Unipolar Depression Evolution of Bipolar I Disorder from MDD Meta-Analysis from Clinical Trials 14 Unipolar Depression Bipolar II Depression Severe MDD, Single Episode, Elevation 12 11.2% Moderate (296.22) Switching to Mania (%) Antidepressant Moderate ≥ 7 days or 10 hospitalization Mild 8 None 6 ≥ 14 days 4.2% Mild 3.7% Depression 4 Antidepressant Bipolar I Disorder, Manic Moderate discontinued (296.40) 2 0.7% 0.5% 0.2% 2716 10,246 3788 125 242 48 = N Severe 0 Significance: TCA = SSRI > Placebo TCA > SSRI = Placebo Ketter TA (Ed). Handbook of Diagnosis and Treatment of Bipolar Disorders . Arlington, VA: American SSRI = selective serotonin reuptake inhibitor (fluoxetine, fluvoxamine, paroxetine, or sertraline); TCA Psychiatric Publishing, Inc.; 2010. = tricyclic antidepressant. Peet M. Br J Psychiatry . 1994;164(4):549-550. Bipolar Mixed State Conceptualization Main Changes for Bipolar and Related Disorders in DSM-IV-TR vs DSM-5 in DSM-5 Compared to DSM-IV-TR • “with mixed features” specifier added for Manic, Hypomanic, and Major Depressive Episodes • Manic Episode with mixed features replaces Mixed Episode • Antidepressant switching – full Manic/Hypomanic Episode emerging during antidepressant treatment and persisting beyond physiological treatment effect now sufficient for Manic/Hypomanic Episode American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Hu J, et al. Prim Care Companion CNS Disord . 2014;16(2). Edition. Arlington, VA: American Psychiatric Association; 2013.
“Overlapping” Symptoms Not Included DSM-5 Major Depressive Episode with mixed features (AKA Mixed Depression) in DSM-5 Mixed Specifier Symptoms characteristic of both poles: • Predominant, full depressive episode and ≥ 3 most days: • Psychomotor agitation (?) ‒ Elevated / expansive mood – Inflated self-esteem / grandiosity ‒ Overtalkativeness – Racing thoughts • Distractibility ‒ Increased goal-directed activity – Impulsivity • Irritability ‒ Decreased sleep need • Mixed symptoms objectively evident, not usual behavior • Insomnia per se • Mania trumps depression • Indecisiveness • Not due to substance / medication American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA: American Psychiatric Association; 2013. Edition. Arlington, VA: American Psychiatric Association; 2013. History of Bipolar I Disorder in Outpatients with History of Major Depressive Episode Diagnostic Challenges II 70 Risk Factor Odds Ratio Percentage among Patients with 66.7% History of psychosis 3.28 • Additional bipolar outcome risk factors 60 (22/33) First-degree relative with mania 2.56 – “Atypical” depressive symptoms Depression onset < 25 years 1.93 50 History of Mania 48.8% • Hyperphagia, hypersomnia, anergia (84/172) 40 – Episode accumulation (≥ 5 lifetime depressions) Overall 26.9% (200/744) 30 – Postpartum mood elevation – Comorbid anxiety/substance use disorder 20 19.3% – 3 consecutive generations with mood disorders 14.7% (62/322) 10 (32/217) – Hyperthymic/cyclothymic temperament 0 None One Two Three Number of Risk Factors Mean age = 37.5 years; P < .0001. Akiskal HS, et al. J Affect Disord . 1983;5(2):115-128. Akiskal HS, et al. Arch Gen Psychiatry . Data from Othmer E, et al. J Clin Psychiatry . 2007;68(1):47-51. Ketter TA (Ed). Handbook of Diagnosis 1995;52(2):114-123. Geller B, et al. Am J Psychiatry . 2001;158(1):125-127. Goldberg JF, et al. Am J and Treatment of Bipolar Disorders . Arlington, VA: American Psychiatric Publishing, Inc.; 2010. Psychiatry . 2001;158(8):1265-1270. Most Bipolar Disorder Patients Have Probabilistic Approach to Bipolar Depression at Least 1 Comorbid Axis I Disorder Bipolar I Depression if ≥ 5: Unipolar Depression if ≥ 4: 80 Symptomatology 70 Hypersomnia Insomnia Hyperphagia Decreased appetite 60 Psychomotor retardation Psychomotor agitation Patients (%) 50 Other “atypical” symptoms All BD 40 Psychosis and/or pathological guilt Somatic complaints BD-I Mood lability or manic symptoms 30 BD-II Onset and Course 20 Earlier onset (< 25 years) Later onset (> 25 years) 10 Multiple depressions (≥ 5 episodes) Long current depression (> 6 months) Family history 0 Bipolar disorder No bipolar disorder None ≥ 3 ≥ 1 ≥ 2 Number of Lifetime Comorbid Axis I Disorders Confirmation of specific numbers requires further study. McElroy SL, et al. Am J Psychiatry . 2001;158(3):420-426. Adapted from Mitchell PB, et al. Bipolar Disord . 2008;10(1 Pt 2):144-152.
Recommend
More recommend