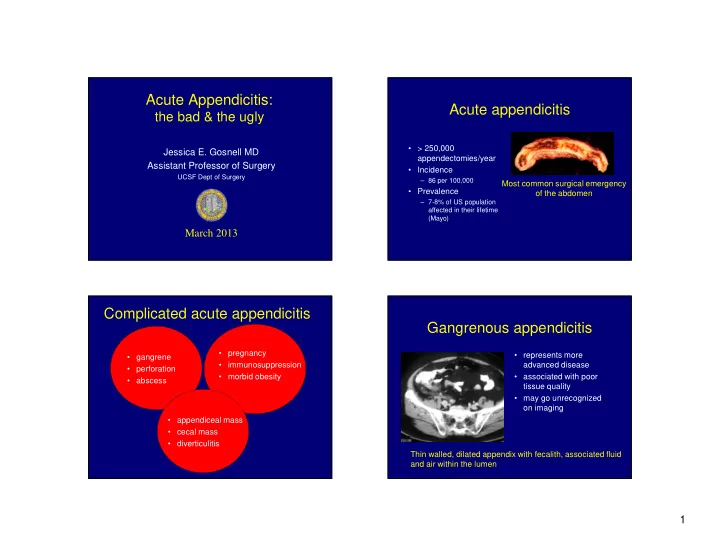
Acute Appendicitis: Acute appendicitis the bad & the ugly • > 250,000 Jessica E. Gosnell MD appendectomies/year Assistant Professor of Surgery • Incidence UCSF Dept of Surgery – 86 per 100,000 Most common surgical emergency • Prevalence of the abdomen – 7-8% of US population affected in their lifetime (Mayo) March 2013 Complicated acute appendicitis Gangrenous appendicitis • pregnancy • represents more • gangrene • immunosuppression advanced disease • perforation • morbid obesity • associated with poor • abscess tissue quality • may go unrecognized on imaging • appendiceal mass • cecal mass • diverticulitis Thin walled, dilated appendix with fecalith, associated fluid and air within the lumen 1
Gangrenous appendicitis Perforated appendicitis • associated with • 15-28% of all cases increased complication • 50% in pts <10yrs, >50yrs rates • may have poor tissue • characterized by more severe quality at site of pain and higher fever appendiceal division – “ no touch ” technique • Tools: – margin of healthy tissue – partial cecectomy if needed (Yak et al, JACS 2007;205(1):60) (Sleem et al, Surgery 2009;146(4):731) Treatment of perforated Antibiotic treatment for perforated acute appendicitis or gangrenous appendicitis • Yes/No? • Antibiotics • open vs. lap Anderson BR et al, Cochrane Database Syst Rev 2005;20:(3) appendectomy -Antibiotic vs placebo for the prevention of postoperative • Irrigation vs suctioning complications after appendectomy • drains -RCT, CCT -outcome measures: wound infection, intra-abdominal abscess, length of stay, mortality -the efficacy of different Abx regimens was not evaluated -45 studies, 9576 patients The use of antibiotics is superior to placebo for preventing wound infection and intra-abdominal abscess 2
Antibiotic treatment for perforated Open vs. laparoscopic or gangrenous appendicitis appendectomy • Type? • Duration? • first described by • first described by Semm McBurney in 1894 in 1983 Baron et al, Clin Inf Dis, Oxford 1992 • safe • allows full exploration of -cultured peritoneal fluid in cases of non- the abdomen • expeditious • allows for “ no touch ” perforated and perforated appendicitis, • small incisions found 3 vs 9 types of bacteria, respectively technique Hoelzer et al, Pediatric Inf Dis J 1999;18:979 • appendix removed in a -assessed the safety of discontinuing Abx when bag device pts postoperatively have –started eating -afebrile -have a normal WBC (Semm et al, Endoscopy 1983;15:59) Cochraine review: Laparoscopic vs. laparoscopic vs. open appendectomy Open Appendectomy for perforated appendicitis • Small, retrospective studies – longer duration of surgery in open group, or no difference • decreased wound infection rate – variable rate of postoperative infections, postoperative ileus • increased intra-abdominal abscess risk – Increased conversion to open rate compared to non- perforated cases • shorter hospital stay – Laparoscopic appendectomy “ advantageous with regard to • Meta-analysis in WJS 2010 • shorter return to normal activity and work infections “ (Markides et al, WJS 2010;34(9):2026) surgical site infections, with no increased intra-abdominal • longer duration of surgery • increased hospital cost • decreased pain as reported by patients (Lim et al, J Korean Soc Coloprocol 2011;27:293) (Yak et al, JACS 2007;205(1):60) (Kirshtein et al, WJS 2007;31(4):744) (Cochraine Database of Systematic Review 2004;18(4):CD001546) (Ball et al, Surgical Endoscopy 2004; 18(6):969 ) 3
Surgical treatment for perforated Appendiceal abscess appendicitis with abscess Percutaneous drainage Early operation interval operation • shorter duration of • longer duration of illness illness • Lower hospital costs • decreased risk of bowel • more common in elderly patients • increased risk of bowel injury • seen in up to 47% of patients with perforated injury • additional work-up appendicitis • ?no further operation • controversy: timing of surgery (Wittmann et al, Principles of Surgery, 6th ed) Early vs Interval appendectomy for children with perforated appendicitis Appendiceal abscess/phlegmon • 131 children enrolled -64 early (<24hrs) -67 interval (6-8wks) • Early appendectomy significantly reduced time away from normal I. Immediate surgery is Abx/immed appy vs activities associated with a higher Abx/interval appy morbidity compared with • The overall adverse events rate after early appendectomy was nonsurgical treatment significantly lower (odds ratio, 3.3; CI: 1.9- 5.6; P < 0.001). II. After successful nonsurgical treatment, a malignant disease is detected in 1.2% (CI: 0.6-1.7) and an important benign disease in 0.7% (CI: 0.2-11.9) during follow-up. • The risk of recurrence is 7.4% (CI: 3.7-11.1) (up in 14% in other studies) (Blakely et al Arch Surg 2011;146(4):660) (Andersson et al, Ann Surg 2007) 4
Appendiceal Abscess Irrigation versus suction for perforated appendicitis CT Scan or Ultrasound Phlegmon + Abscess > 4-6cm • St. Peter et al. Ann Surgery 2012;256(4):581 Small Abscess Irrigation versus suction alone during Antibiotics Fever/ Sepsis Afebrile Drainage laparoscopic appendectomy for perforated appendicitis: a prospective randomized trial Children Adults Interval -220 patients treated laparoscopically and enrolled No Improvement Improvement Appendectomy -no difference in the abscess rate, which was 19.1% with Regular Diet, Antibiotics Operate Discharge suction only and 18.3% with irrigation Colonoscopy 2-4 weeks No Neoplasm Neoplasm (From Maa & Kirkwood, Consider Interval Staging/ Colectomy Sabiston 18th ed) Appendectomy The role of routine abdominal Tools/tips for perforated/gangrenous drainage appendicitis • Allemann P et al Langenbacks Arch Surg • Preoperative planning 2011;396:63 • Multiple scopes, endoloops vs staplers Prevention of infectious complications after • Pulse lavage, high -flow irrigation system laparoscopic appendectomy for complicated • Additional ports acute appendicitis- the role of routine abdominal • Alternate surgeon positions drainage • Alternate patient positions • Conversion vs delayed operation -case match study of 130 patients -uncomplicated appendicitis and diffuse peritonitis excluded -patients without drains had fewer complications, shorter LOS 5
Acute appendicitis in the Complicated acute appendicitis immunosuppressed Organ transplantation HIV/AIDS • pregnancy • immunosuppression Immunosuppressive tx for autoimmune or neoplastic pathology • morbid obesity • old age • physical findings may be mild • chronic illness • broad differential • enterocolitis/typhlitis not uncommon • do not delay operative tx • involve patient and Oncologist in the decision • outcomes may be poor (Chui et al, Pediatr Blood Cancer 2008;50(6):1282) Acute appendicitis in the Acute appendicitis in the immunosuppressed morbidly obese • Diagnosis can be difficult • Imaging restrictions based on weight • Laparoscopic appendectomy associated with shorter LOS and morbidity • Need to request bariatric equipment – bariatric OR, ward beds – pressure points padded – extra long trocars and instruments 39yo woman day 12 of tx for relapsing acute lymphoblastic leukemia, with WBC 0.1, PLT count 10k 6
Complicated acute appendicitis Appendiceal carcinoid • comprise 1-2% of • Most common neoplasms of appendectomies the appendix • appendectomy if small mass • Most often discovered in 4-5 th (<2cm), not involving the decade of life • appendiceal mass • Carcinoid base • 75% involve distal 1/3rd, less • cecal mass • consider cecectomy, than 10% involve base • cecal diverticulitis hemicolectomy • Most tumors are less than 1cm (Moertel et al, NEJM 1987) • 5 yr survival 94% local, 85% regional mets, 34% distal (Landry el al, Arch Surg 2008;143(7):664) (Landry el al, Arch Surg 2008;143(7):664) (Harada et al, Am J Surg 1993;166:666) (Harada et al, Am J Surg 1993;166:666) Adenocarcinoma of the Mucinous adenoacarcinoma of appendix the appendix • Comprise 0.1-0.8% of appendectomies • Rare tumors of the appendix • 29% nodal metastases • Propensity of peritoneal- based metastases, but low • Prognosis poor- 5 yr survival • adenocarcinoma • mucinous adenoca nodal metastasis (6-20%) about 20% with appendectomy alone, 63% • Hemicolectomy controversial. after right colectomy Historically accepted, good for staging, several studies • Appendectomy sufficient for showed no statistical mucosal lesions with negative difference in survival margins (Hesketh KT Gut 1963:4:158) (Turaga et al Ann Surg Oncol 2013;20:1063) 7
Laparoscopic tools for Cecal diverticulitis complicated acute appendicitis • Right sided diverticulitis first described by Potier in 1912 • 10 and 5-30 degree scopes • “true” diverticulea medically if dx ’ d on imaging, • High pressure pulse-lavage irrigation • cecal diverticulitis treated • cecal diverticulitis that dx ’ d intraoperatively system treatment is controversial for • Open Hasson technique for pregnant patients • Multi-disciplinary care as needed (OB, Cardiology, Bariatric, Heme-Onc, Surg Onc) (Issa et al Eur J Gastroenterol Hepatol 2012;24:1254) 8
Recommend
More recommend