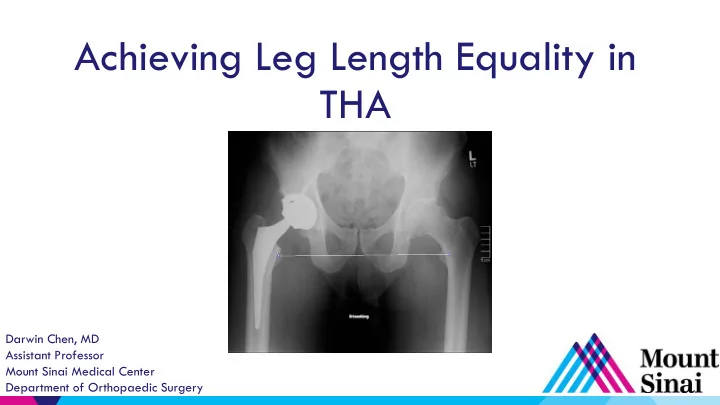
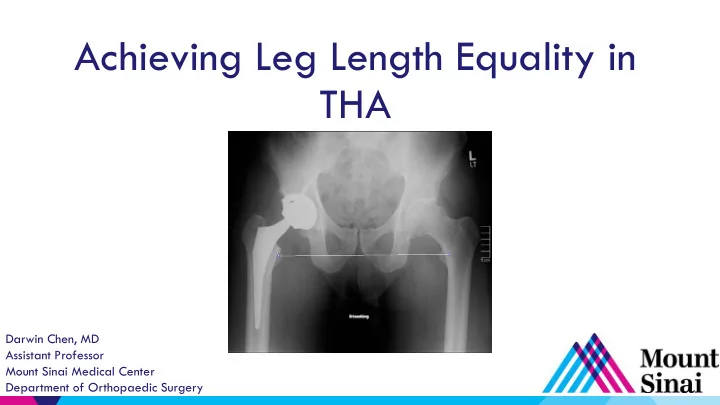
Achieving Leg Length Equality in THA Darwin Chen, MD Assistant Professor Mount Sinai Medical Center Department of Orthopaedic Surgery
Disclosures ▶ Monogram Orthopedics Consultant – ▶ Conformis Medical advisory board, consultant –
Leg Length Inequality ▶ One of the most vexing problems in THA ▶ Hard to define – Less than 1mm, 5mm,10mm? – Patient perception? ▶ Prevalence unknown ▶ 32-44% patients perceive LLD postop – Shortening < 10mm Ranawat, J Arthroplasty 2001 Woolson, J Arthroplasty 1999 – Lengthening > 6mm Hoffman, Orthpedics 2000 McGrory, JBJS 1995
Why is Leg Length Inequality Important? ▶ Abnormal gait ▶ LBP , knee pain ▶ Nerve palsy ▶ Shoe wear ▶ Dissatisfaction ▶ Most common reason for litigation after THA! Clark, JAAOS 2006
Today’s Routine, Primary THA Should Be “Perfect” ▶ “…patients very soon become adjusted to 1cm of over- lengthening.” Sir John Charnley 1979 ▶ A pain free THA isn’t good enough anymore ▶ Happy patient = – No pain - Well fixed implants – Good function - Stability – Equal leg lengths
Preoperative History and Physical Exam ▶ Do your legs feel equal? ▶ PMHx – Spinal deformity/fusion – Prior trauma – Neuromuscular disorder – DDH ▶ Exam – Pelvic obliquity – Flexion contracture – Shoe modification
Preoperative History and Physical Exam ▶ True leg length – ASIS to medial malleolus ▶ Apparent leg length – umbilicus to medial malleolus *Postop* *Preop*
Templating is the Key to THA Success ▶ Goal – restore hip center of rotation, recreate offset, correct LLD ▶ Determine – Neck cut level – Acetabular position – Stem size and offset
Templating is the Key to THA Success ▶ Proper AP femur – 15º IR ▶ Proper marker ball placement “Ball on ball” sign Improper marker ball placement 15º IR
Templating is the Key to THA Success
Intraoperative Instability ▶ Don’t let intraoperative instability make you lengthen the leg…look for other sources!
Posterior Approach – LLD Assessment ▶ Knee/heel assessment – Subjective, dependent on leg shape, pelvic position – Feel before neck cut, compare with template – Compare with trials ▶ “Shuck” test – Unreliable – Dependent on relaxation, soft tissue quality/contractures
Posterior Approach – LLD Assessment ▶ “L to C” - lesser trochanter to center of femoral head
Posterior Approach – LLD Assessment ▶ Bent Steinmann pin Mcgee, Scott, CORR 1985
Posterior Approach – LLD Assessment ▶ Calipers/tools
Direct Anterior Approach – Improved Leg Lengths? ▶ Trans-ischial or trans-teardrop line
Direct Anterior Approach – Improved Leg Lengths? ▶ Off-table, direct assessment K Berend
Direct Anterior Approach – Improved Leg Lengths? ▶ Overlay method J Matta
Does Advanced Technology Help? $$$
Does Advanced Technology Help? June 2015 “Robot-assisted posterior THA, fluoroscopy-guided anterior THA, and conventional posterior THA did not differ in obtaining minimal LLD. All three techniques are effective in achieving accuracy in LLD.”
Conclusions ▶ Preoperative templating is critical to restoring leg length and offset ▶ Posterior – lesser to center, calipers, pins, knee/heel ▶ Anterior – fluoroscopy, overlay, direct supine assessment ▶ A robotic/navigation system can help but is unnecessary and adds excessive cost
Thank You Darwin Chen, MD Assistant Professor Mount Sinai Medical Center Department of Orthopaedic Surgery
Recommend
More recommend