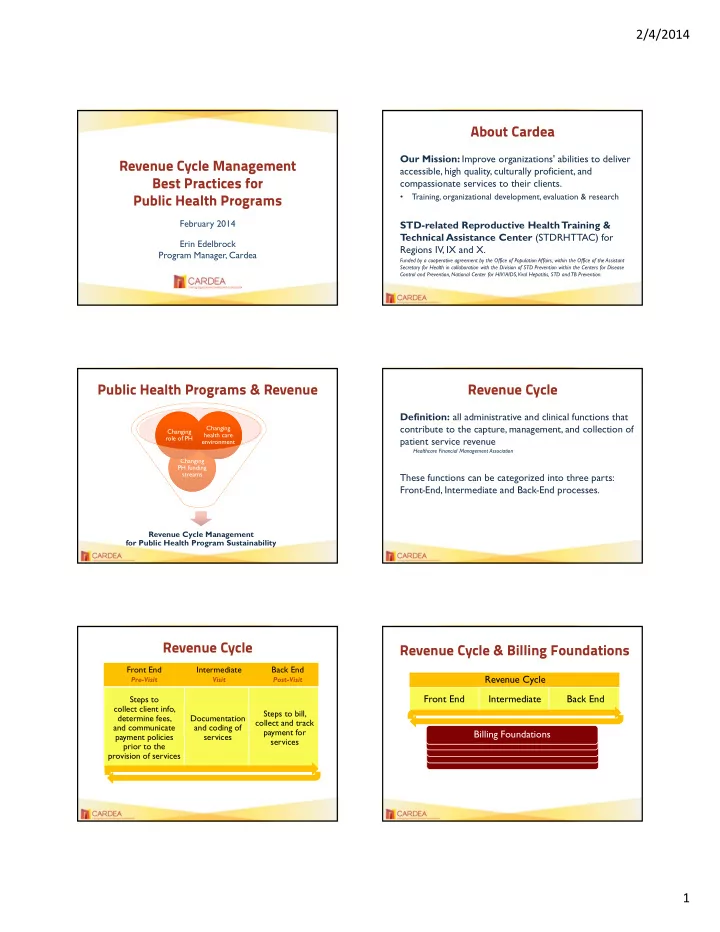
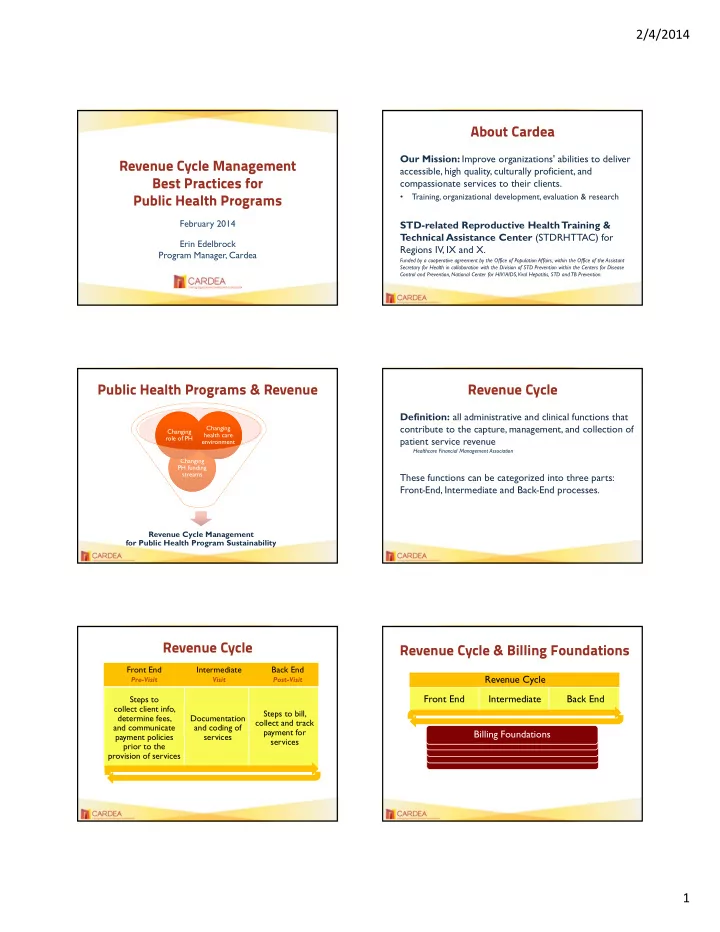
2/4/2014 About Cardea Our Mission: Improve organizations' abilities to deliver Revenue Cycle Management accessible, high quality, culturally proficient, and Best Practices for compassionate services to their clients. Training, organizational development, evaluation & research Public Health Programs • February 2014 STD-related Reproductive Health Training & T echnical Assistance Center (STDRHTTAC) for Erin Edelbrock Regions IV, IX and X. Program Manager, Cardea Funded by a cooperative agreement by the Office of Population Affairs, within the Office of the Assistant Secretary for Health in collaboration with the Division of STD Prevention within the Centers for Disease Control and Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD and TB Prevention. Public Health Programs & Revenue Revenue Cycle Definition: all administrative and clinical functions that contribute to the capture, management, and collection of Changing Changing Changing Changing health care health care role of PH role of PH patient service revenue environment environment Healthcare Financial Management Association Changing Changing PH funding PH funding streams streams These functions can be categorized into three parts: Front - End, Intermediate and Back - End processes. Revenue Cycle Management for Public Health Program Sustainability Revenue Cycle Revenue Cycle & Billing Foundations Front End Intermediate Back End Revenue Cycle Pre-Visit Visit Post-Visit Front End Intermediate Back End Steps to collect client info, Steps to bill, determine fees, Documentation collect and track and communicate and coding of payment for Billing Foundations payment policies services services prior to the provision of services 1
2/4/2014 Billing Foundation Revenue Cycle Management IS NOT… Third Party Payer Relationships Only related to billing insurance; it includes collecting Leadership & Staff Buy-in patient fees, managing program funds, etc. Information System Capacity IS… Workforce Capacity the management of revenue cycle processes to allow for a steady stream of revenue Legislative/Policy Landscape Revenue cycle management reflects an important truth— your services have value! Adapted from Elements for Successful Immunization Billing Practice, New York State Dept of Health, June 2012 Best Practices: Front End Processes Scheduling GOALS COLLECT from the patient: • Collect complete and accurate information • Contact and demographic info • Communicate financial policies to clients • Insurance info • Collect first-party payments, as appropriate • Reason for visit COMMUNICATE to the patient: • Agency financial policies and payment options • Required documents for visit Eligibility/Pre-Authorization Reminders & Registration Using the information captured at scheduling… Three opportunities to collect info from and communicate info to the patient: • Contact insurance carrier to determine eligibility and seek pre-authorization, if applicable • Initial scheduling • Reminder call Reduces denials due to incorrect/missing information or • Registration/Check-in insufficient coverage Reduces time at check-in 2
2/4/2014 Registration/Check-in Front End – Final Steps COMMUNICATE to the patient: • Verify insurance eligibility • Agency financial policies and payment options • Pre-populate encounter form/superbill COLLECT from the patient: • Any updated contact, demographic, insurance info • Copy of insurance card, as applicable • Signed release forms (address confidentiality) • Co-pays or other fees? Best Practices: Intermediate Processes Documentation & Coding GOALS • Correctly and completely document all clinical care / Paper Electronic Clinical Care capture all billable services Encounter Encounter Documentation • Capture corresponding charges and codes Form/Superbill Form/Superbill + Charge Capture (EHR, Manual Charge Practice Coding Services Entry Management) Documentation & Coding Best Practices: Back End Processes Paper or electronic, either way… GOALS • Documentation, charge capture and coding is a • Submit claims/send bills in an accurate and timely fashion partnership between providers and billing staff • Pursue all available avenues for reimbursement • Charges and codes must be supported by medical • Minimize errors documentation 3
2/4/2014 Check Out Claims Submission COMMUNICATE to the patient: Review and correct claims • Charges and account details, including the patient’s • Codes and charges, patient and provider info obligation • In-house v. Clearinghouse COLLECT from the patient: Timely submission (know your payer’s guidelines) • Payment, as appropriate (enter immediately) • Commitment to a payment plan, as appropriate Remittance Advice and Payment Posting Denials Management Remittance advice: information sent to a provider explaining • Denials for claim errors; often easily corrected how payments, adjustments or denials were applied modify and resubmit • Denials due to payer error appeal Paid? Congratulations! Post payment to the appropriate • Denials due to lack of coverage for the patient or the account as soon as possible service, unpaid deductible/co-ins, etc. bill secondary payers or patient, as appropriate Partially paid or denied? Don’t give up – follow-up! Quality Improvement Patient Billing Check payer and program rules (including Medicare, Quality Improvement Quality Assurance Medicaid, Title X) around balance billing to patients • A philosophy/approach • A specific activity If balance billing allowed… • Driven by staff & clients • Driven by management • Have written policies and procedures and train staff on • Focuses on systems and • Focus on policies & processes; builds on procedures; tasks & how to discuss charges and balances strengths compliance checks • Send initial statement as close to visit as possible; follow up • Assumes that the system, • Includes performance with regular, detailed statements NOT the individual is the evaluations • Provide multiple payment options root cause of most • Seeks to identify problems problems and make corrections 4
2/4/2014 What are your agency’s strengths A Quality Improvement Plan and areas for improvement? • Leadership Involvement — Mission, Goals, Resources Front End Intermediate Back End • T eam Empowerment—Responsibilities, Timeline Scheduling Clinical Care Claims Submission • Customer Focus Documentation Registration Claims Follow-up • Data Collection—tools; defined indicators, Charge Capture Eligibility Verification Denials management benchmarks Coding Services Fee Determination Payment posting • Process—Plan, Do, Check, Act; continuous Patient communication Balance billing • Celebrate success! Quality Improvement William J. Riley, et al. Realizing Transformational Change Through Quality Improvement in Public Health. J Public Health Management Practice, 2010. Resources from Cardea Contact Information • Case studies of public health programs that are currently billing • Webinars and other online learning tools • An online learning community to help you connect with peers and access resources • Customized training and technical assistance Erin Edelbrock Program Manager erin@cardeaservices.org 206.447.9538 www.cardeaservices.org @CardeaServices 5
Recommend
More recommend