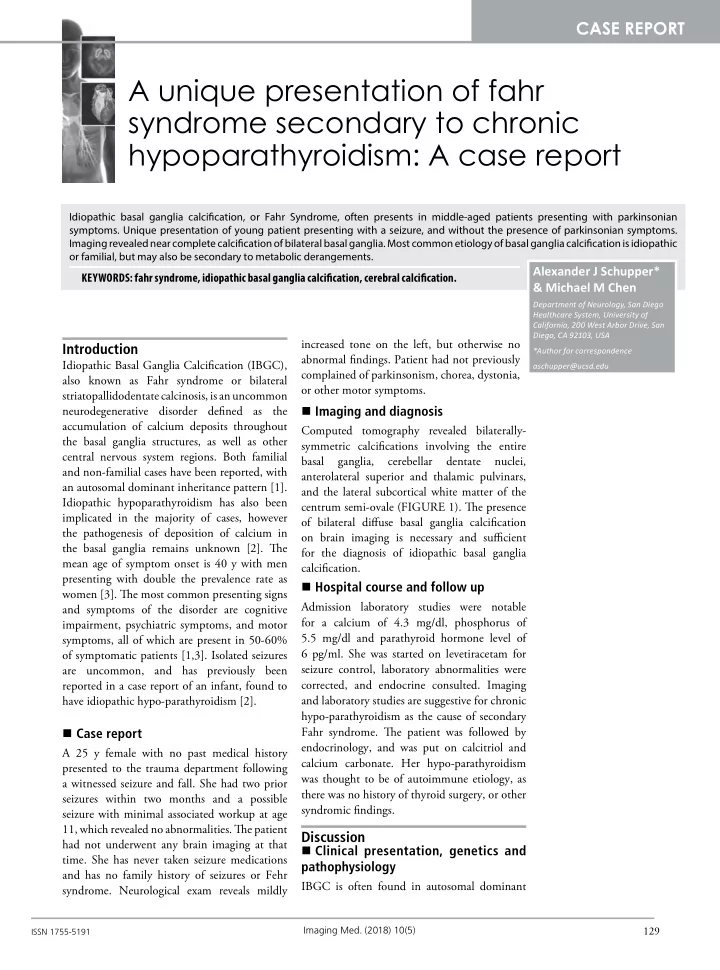
CASE REPORT A unique presentation of fahr syndrome secondary to chronic hypoparathyroidism: A case report Idiopathic basal ganglia calcifjcation, or Fahr Syndrome, often presents in middle-aged patients presenting with parkinsonian symptoms. Unique presentation of young patient presenting with a seizure, and without the presence of parkinsonian symptoms. Imaging revealed near complete calcifjcation of bilateral basal ganglia. Most common etiology of basal ganglia calcifjcation is idiopathic or familial, but may also be secondary to metabolic derangements. Alexander J Schupper* KEYWORDS: fahr syndrome, idiopathic basal ganglia calcifjcation, cerebral calcifjcation. & Michael M Chen Department of Neurology, San Diego Healthcare System, University of California, 200 West Arbor Drive, San Diego, CA 92103, USA increased tone on the left, but otherwise no Introduction *Author for correspondence abnormal fjndings. Patient had not previously Idiopathic Basal Ganglia Calcifjcation (IBGC), aschupper@ucsd.edu complained of parkinsonism, chorea, dystonia, also known as Fahr syndrome or bilateral or other motor symptoms. striatopallidodentate calcinosis, is an uncommon Imaging and diagnosis neurodegenerative disorder defjned as the accumulation of calcium deposits throughout Computed tomography revealed bilaterally- the basal ganglia structures, as well as other symmetric calcifjcations involving the entire central nervous system regions. Both familial basal ganglia, cerebellar dentate nuclei, and non-familial cases have been reported, with anterolateral superior and thalamic pulvinars, an autosomal dominant inheritance pattern [1]. and the lateral subcortical white matter of the Idiopathic hypoparathyroidism has also been centrum semi-ovale (FIGURE 1). Tie presence implicated in the majority of cases, however of bilateral difguse basal ganglia calcifjcation the pathogenesis of deposition of calcium in on brain imaging is necessary and suffjcient the basal ganglia remains unknown [2]. Tie for the diagnosis of idiopathic basal ganglia mean age of symptom onset is 40 y with men calcifjcation. presenting with double the prevalence rate as Hospital course and follow up women [3]. Tie most common presenting signs Admission laboratory studies were notable and symptoms of the disorder are cognitive for a calcium of 4.3 mg/dl, phosphorus of impairment, psychiatric symptoms, and motor 5.5 mg/dl and parathyroid hormone level of symptoms, all of which are present in 50-60% 6 pg/ml. She was started on levetiracetam for of symptomatic patients [1,3]. Isolated seizures are uncommon, and has previously been seizure control, laboratory abnormalities were corrected, and endocrine consulted. Imaging reported in a case report of an infant, found to have idiopathic hypo-parathyroidism [2]. and laboratory studies are suggestive for chronic hypo-parathyroidism as the cause of secondary Case report Fahr syndrome. Tie patient was followed by endocrinology, and was put on calcitriol and A 25 y female with no past medical history calcium carbonate. Her hypo-parathyroidism presented to the trauma department following was thought to be of autoimmune etiology, as a witnessed seizure and fall. She had two prior there was no history of thyroid surgery, or other seizures within two months and a possible syndromic fjndings. seizure with minimal associated workup at age 11, which revealed no abnormalities. Tie patient Discussion had not underwent any brain imaging at that Clinical presentation, genetics and time. She has never taken seizure medications pathophysiology and has no family history of seizures or Fehr IBGC is often found in autosomal dominant syndrome. Neurological exam reveals mildly Imaging Med. (2018) 10(5) 129 ISSN 1755-5191
CASE REPORT Schupper, Chen Figure 1. Axial CT images demonstrating dense, bilaterally-symmetric calcifjcations involving the entire basal ganglia, dentate nuclei in cerebellum, anterolateral superior thalami, thalamic pulvinars and the lateral subcortical white matter of the centra semi-ovale. families, but has also been reported in sporadic thought to be due to endocrine disorders, cases. Most patients are diagnosed in middle specifjcally disturbances in the regulation of age, and men are twice as likely to be diagnosed parathyroid hormone. Hypo-parathyroidism can lead to increased calcinosis, and it is believed as women [3]. Here we present a young woman that calcium deposition begins in the vessel with no afgected family members presenting wall, eventually extending to the neuron. Tiis with difguse basal ganglia calcifjcations. deposition of the basal ganglia leads to impaired Calcifjcations most commonly reported in local circulation, causing additional neuronal the globus pallidus, but may be present in the injury and subsequent increased calcium centrum semi-ovale and cortical white matter, deposition [5]. as seen in our patient. Tie presence of extra- basal ganglia calcifjcation may be the cause of Differential diagnosis this patient’s unique presentation of multiple seizures. Tie majority of patients present with In determining the diagnosis of IBGC, one symptoms of parkinsonism and movement must also consider the various causes of disorders, cognitive decline, and psychiatric intracranial calcifjcations. Often the clinical symptoms [1,3,4]. presentation and location of calcifjcation on brain imaging may be helpful in determining IBGC has a strong genetic link, with a familial the diagnosis. Basal ganglia calcifjcation must be autosomal dominant inheritance being found present for the IBGC diagnosis, and the globus most commonly. SLC20A2 on chromosome pallidus is almost universally afgected. Patients 8p11.2 and PDGFRB on chromosome 5q32 most common present with either cognitive, have been the most commonly implicated psychiatric or parkinsonian symptoms, however, genetic mutations, though other genes have led patients may present with seizures (as seen in to similar phenotypes [1]. our patient), headache, stroke, vertigo, paresis, Basal ganglia calcifjcation is most commonly or other neurological presentations. Imaging Med. (2018) 10(5) 130
A unique presentation of fahr syndrome secondary to chronic hypoparathyroidism: A CASE REPORT case report To diagnose IBGC, other causes must be antioxidants and calcium antagonists have ruled out. Tie many etiologies of intracranial been reported, however, these results have calcifjcations, including infectious, metabolic, not been confjrmed [6]. For the rare patient congenital and vascular, must be further presenting with seizure activity, antiepileptic explored in determining the cause of basal drug use with medications such as levetiracetam ganglia calcifjcations. For example, the TORCH are appropriate. In a young female patient of infections (toxoplasmosis, other, rubella, childbearing age, it is important to limit the use cytomegalovirus, herpes simplex virus) must of teratogenic medications including valproic be considered, as they may cause intracranial acid and carbamazepine. calcifjcations. Most commonly, metabolic Conclusion derangements causing problems with calcium homeostasis are a common cause of basal Fahr syndrome is a rare neurodegenerative ganglia calcifjcation. Serum levels of alkaline disease defjned by the presence of bilateral basal phosphatase, calcium, calcitonin, parathyroid ganglia calcifjcations. Most cases are familial, hormone, as well as infectious labs and heavy and there is a strong genetic component to the metal concentrations are recommended. disease, specifjcally an autosomal dominant inheritance. Patients commonly present with Management cognitive, motor and/or psychiatric symptoms, Currently there is no treatment for IBGC, but may present in a variety of phenotypes. and management is limited to supportive care Idiopathic basal ganglia calcifjcation may for presenting neurological and psychiatric present similarly to other infectious, metabolic, symptoms. If underlying metabolic disturbances congenital or vascular disorders afgecting the are found, as seen in this patient, correctly nervous system, and an exhaustive workup must underlying abnormalities may improve be conducted to rule out other causes. the presenting symptoms. Chelators with J. Pediatr. Neurosci . 10, 178-180 (2015). 5. Saleem S, Aslam HM, Anwar M et al . Fahr's REFERENCES syndrome: literature review of current evidence. 1. Nicolas G, Pottier C, Charbonnier C et 3. Manyam BV, Walters AS, Narla KR. Bilateral Orphanet. J. Rare. Dis . 8, 156 (2013). striopallidodentate calcinosis: clinical al . Phenotypic spectrum of probable and genetically-confjrmed idiopathic basal ganglia characteristics of patients seen in a registry. Mov. 6. Skvortsov IA, Rudenskaia GE, Karaseva AN et al . calcifjcation. Brain . 136, 3395-3407 (2013). Disord . 16, 258 (2001). Efgectiveness of therapeutic use of complexones in various diseases of the extrapyramidal system 2. Bhat MA, Laway BA, Mustafa F. Bilateral basal 4. Mufaddel AA, Al-Hassani GA. Familial in children. Zh. Nevropatol. Psikhiatr. Im. S. S. idiopathic basal ganglia calcifjcation (Fahr’s ganglia calcifjcation and recurrent Korsakova . 87, 1457-1462 (1987). generalized seizures as initial presentation disease). Neurosciences . 19, 171-177 (2014). of idiopathic hypoparathyroidism in an infant. 131 Imaging Med. (2018) 10(5)
Recommend
More recommend