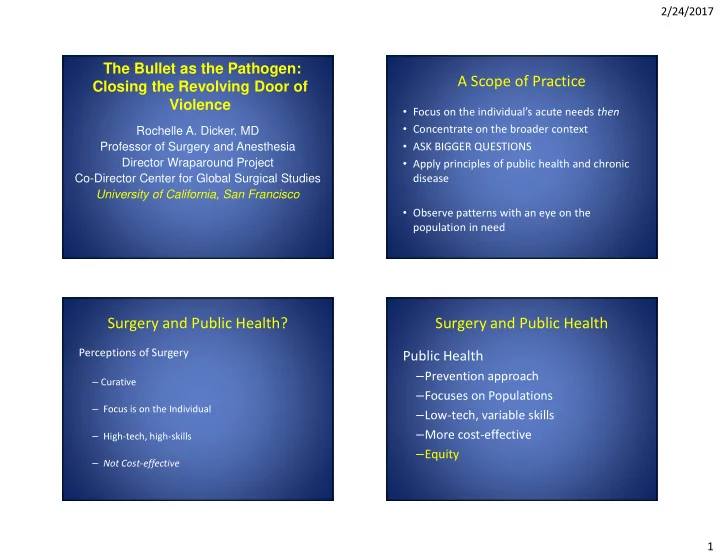
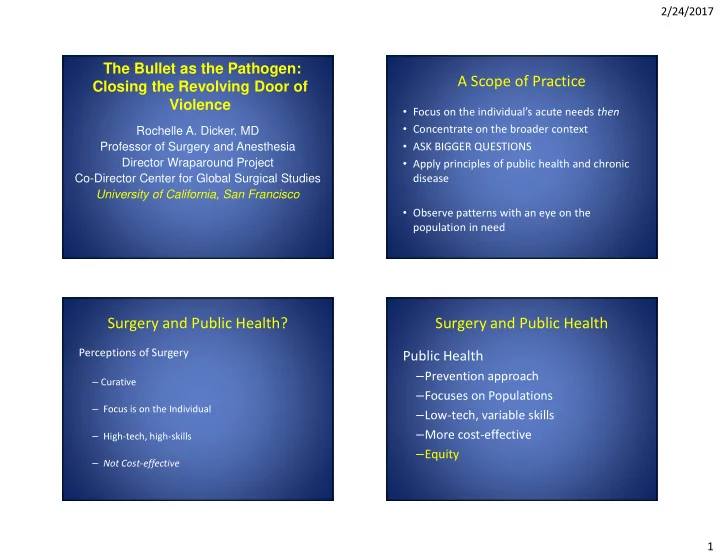
2/24/2017 The Bullet as the Pathogen: Closing the Revolving Door of A Scope of Practice Violence • Focus on the individual’s acute needs then • Concentrate on the broader context Rochelle A. Dicker, MD Professor of Surgery and Anesthesia • ASK BIGGER QUESTIONS Director Wraparound Project • Apply principles of public health and chronic Co-Director Center for Global Surgical Studies disease University of California, San Francisco • Observe patterns with an eye on the population in need Surgery and Public Health? Surgery and Public Health Perceptions of Surgery Public Health – Prevention approach – Curative – Focuses on Populations – Focus is on the Individual – Low-tech, variable skills – More cost-effective – High-tech, high-skills – Equity – Not Cost-effective 1
2/24/2017 NEARLY 6 MILLIONS LIVES Injury is a Public Health Problem Public Health Injury Surveillance Advocacy Research Services Policy Prevention & Control Evaluation Severity and Disparity of Homicide The San Francisco Story in Youth and Young Adults The Urban America Story #1 cause of death in young African Americans, 15-34 years old #2 in Latinos, 15-34 years old 53 per 100,000 African Americans 20 per 100,000 in Latinos 2
2/24/2017 Who Owns It? “ “ Violence is a public “ “ health issue ” ” ” ” Public Health C. Everett Koop , US Surgeon Injury Surveillance Advocacy General, 1984 Services Research Policy Prevention & Control Evaluation Surveillance 76% of homicide and assault victims had criminal histories African American men are 13 times more likely to be injured (15-34) 2 per 1000 AA men are injured from violence 4% of population and 60% of gunshot victims 3
2/24/2017 Social Determinants of Health • Complex interplay of social and economic systems – Social and structural systems in which people exist – Systems designed to address people’s health issues – Shaped by income, power, and resources • Globally, nationally, locally • What this means for PREVENTION • Health and Wealth: Population Health in 2050 and implications for the US Risk Factors for Violence: SOCIAL DETERMINANTS OF Protective Factors HEALTH • Adult mentorship • Poverty • Substance abuse • Interpersonal skills • Family dysfunction • Lack of role models • Commitment to school • Access to Guns • Educational deficiencies • Access to resources • Mental Illness • Hopelessness • Community morés: • RECIDIVISM • Joblessness – Social cohesion + willingness to intervene for the common good = reduction in violence • Intergenerational • Environment - Science RJ Sampson, SW Raudenbush, F Earls. • Normalization Health and Chronic Vol 277; 15 August 1997 Disease 4
2/24/2017 APPROACHES TO PREVENTION Public Health Injury Surveillance Advocacy Services Research Policy Prevention & Control Evaluation Purtle J, Cheney R, Wiebe DJ, Dicker RA Injury Prevention 2015;21:140-141 The Trauma Center’s Role in Public Health and Prevention The Teachable Moment: Precedent for it Risk reduction strategies – Public Health Model – Culturally Competent Case Management – Community and City partnerships 5
2/24/2017 THE WRAPAROUND PROJECT: The Wraparound Project A HOSPITAL BASED VIOLENCE INTERVENTION PROGRAM Cornerstones The Public Health Model for Injury Prevention Seizing the Teachable Moment AIMS – Provide intervention to reduce Long-term Culturally Competent Case Management recidivism and incarceration Providing Links to Risk Reduction Resources – Reestablish standard of care for violent injury in trauma centers serving communities affected by violence The Wraparound Project Target Population Cultural relevance Willingness to accept Sustainability Community “ “ “ ownership ” “ ” ” ” Permission to Seize the Teachable Moment Collaboration with Organizational collect data community Climate Access to… Willingness to accept Renewable $$$ “ “ Buy-in ” “ “ ” ” from leaders ” Fit with existing Leadership programs Positive image Strong host organization and staff Strong program advocates The Case Manager FEASIBILITY Resources • Working knowledge of urban violence Costs Training Space Evaluability Access to Available baseline data • Experience overcoming violence equipment and Access to clients over time Community Climate materials Simple program design Willingness to accept Incentives Access to statistical skills • Crisis management Fit with existing and funding Collaborative programs partners Permission to collect data • Positive force in the community Access to referral networks 6
2/24/2017 Key Partnerships Intervention Program Design • Community morés: – Social cohesion + willingness to intervene for the INJURY Initial Trauma Care common good = reduction in violence • Community Response Networks • Glide Memorial Church Teachable Assessment by Case HOSPITAL • Carecen tattoo removal Moment Managers at Bedside CARE • Family Mosaic of Bayview Low Risk High Risk • Arriba Juntos • Community GED Programs • Instituto Familia de la Raza RECOVERY Referral to Appropriate • Healthright 360 The Resources • Trauma Recovery Center Wraparound Project Vocational Training Program with AT and T Advocacy Center Friends of the Urban Forest • Teaches victims of violence skills and • Tutorial Services knowledge to be arborists • Partnership with School District • Life skills • GREAT job opportunities • Success Center Job Readiness • Project Rebound at SFSU • Funded by Metta, Bank of America, Hearts • Men’s Group 7
2/24/2017 Public Health Injury Surveillance Advocacy Services Research Policy Prevention & Control Evaluation COMPONENTS OF PROGRAM EVALUATION F ORMATIVE EVALUATION INDEPENDENT P ROCESS PREDICTORS EVALUATION OF SUCCESS I MPACT EVALUATION Journal of Trauma and Acute Care Surgery 2013; 74:976-982 O UTCOME EVALUATION 8
2/24/2017 Specific Aims Need Success Rate 1. PROCESS EVALUATION: To determine the screening, Mental Health 86% approached and enrollment rates of clients Employment 86% 2. IMPACT EVALUATION: To determine capacity at Housing 75% meeting individual risk reduction needs 3. OUTCOME EVALUATION: To determine the overall Education 72% injury recidivism rate and compare it to our Family Counseling 80% historical institutional control Court Advocacy 76% Driver ’ s License 4. To determine which risk reduction resources are Vocational Training 70% independent predictors of program completion and success 89% Other 66% Need Success Rate Odds Ratio Case Manager Dose Mental Health 86% 5.97 SUCCESS Employment 86% 4.41 Housing 75% 1.12 Education 72% 0.63 Family 80% 2.26 Counseling Court Advocacy 76% 1.29 Driver ’ s License Vocational 70% 0.69 Training 89% 3.53 Other 66% 1.48 9
2/24/2017 Conclusion • Providing mental health care and employment opportunities Is predictive of success. • The value of early “ high dose ” intensive case management is essential. • 466 clients enrolled • Most common needs: Mental health, housing, employment • Recidivism rate: 50% less than historical controls • Meeting education needs was associated with success • Housing: A risk factor? 10
2/24/2017 • Hospital Care • Skilled Nursing $282 Billion Physical Physical • Rehabilitation • Functional Each Year Impairment JOURNAL OF TRAUMA AND ACUTE CARE SURGERY The The VOLUME 78, NUMBER 2 Costs of Costs of Economic Economic Emotional Emotional Violence Violence • Hospital • PTSD • Depression Costs • Lost Wages • Anxiety • Fear Societal Societal • Unsafe Neighborhoods Specific Aims Markov Analysis 1. To determine the mean cost of trauma per individual at our institution Injured Victim 2. To determine the mean cost of our hospital- centered violence intervention program per individual No Intervention Intervention Program 3. To compare the cost-utility of hospital-based Program violence intervention programs to no intervention in young adults victims of interpersonal violence Reinjured Rehabilitated Reinjured Rehabilitated 11
2/24/2017 WHO FUNDS THIS? What do they want to see? • Hospital-centered • Mayors and Supervisors • Departments of Public Health violence intervention programs cost money • Foundations but cost less than caring • Federal government for patients after re- • Private donors injury. • …POLICY CHANGE National Network of Hospital-Based Violence Intervention Programs Public Health Injury Surveillance Advocacy Services Research Policy Prevention & Control Evaluation 12
Recommend
More recommend