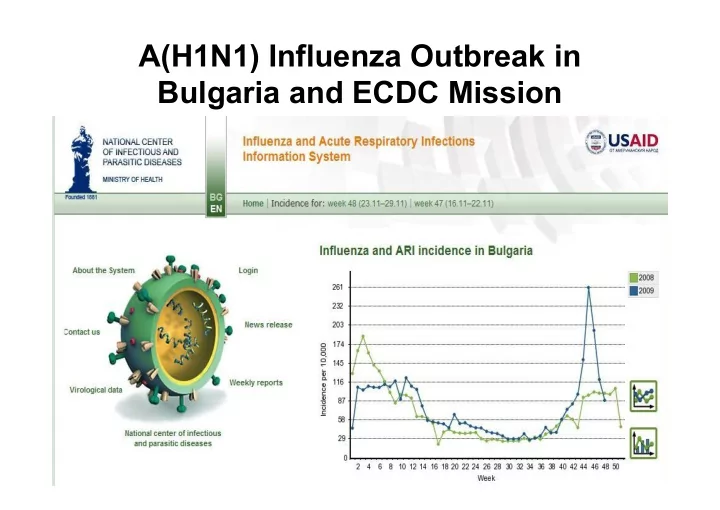
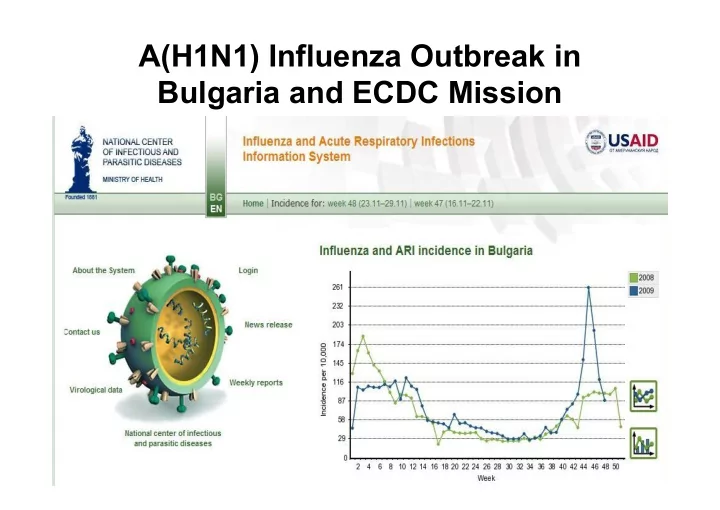
A(H1N1) Influenza Outbreak in Bulgaria and ECDC Mission
44, 45, 46 week (26.10-15.11.2009) 44 45 46
AH1N1 RT-PCR tests done in the National Reference Laboratory, May-November, 2009 748 Total number of samples - 2191 Positive for A(H1N1)pdm - 748 (34,1%)
Distribution of samples by age groups 1000 872 900 800 703 700 600 500 370 400 279 300 220 201 149 200 97 100 37 11 0 0- 4г . 5-14 г . 15-29 г . 30-64 г . 65+ Total number of samples Posititve for A(H1N1)pdm
Distribution of samples by week 40 – 48, 2009 . 450 400 350 300 250 200 150 100 50 0 40 41 42 43 44 45 46 47 48 Total number of samples Positive for A(H1N1)pdm
Distribution of deaths by age groups 66% 6% 34% 34% % 21 21 11 11 cases 15-29 15-29 30-64 0-64
Distribution of deat Distribution of deaths by sex hs by sex women men 44% 56%
Distribution of deaths by time of seeking medical help 72 2 % 60 28 % 28 % 40 23 23 20 % 9 cases 0 on n time ime late ate
Distribution of deaths by antiviral treatment Distribution of deaths by antiviral treatment starting time starting time no treatment 13% on time 31% late 56%
Distribution of deaths by presence of risk factors obesity; 12 no risk; 41 chronic illnesses; 38 pregnancy; 9
Fatal cases EU/EFTA countries Week 50
Fatal cases EU/EFTA countries Week 17
Fatal cases EU/EFTA countries Week 18
Fatal cases EU/EFTA countries Week 19
Fatal cases EU/EFTA countries Week 20
Fatal cases EU/EFTA countries Week 21
Fatal cases EU/EFTA countries Week 22
Fatal cases EU/EFTA countries Week 23
Fatal cases EU/EFTA countries Week 24
Fatal cases EU/EFTA countries Week 25
Fatal cases EU/EFTA countries Week 27
Fatal cases EU/EFTA countries Week 28
Fatal cases EU/EFTA countries Week 29
Fatal cases EU/EFTA countries Week 30
Fatal cases EU/EFTA countries Week 31
Fatal cases EU/EFTA countries Week 32
Fatal cases EU/EFTA countries Week 33
Fatal cases EU/EFTA countries Week 34
Fatal cases EU/EFTA countries Week 35
Fatal cases EU/EFTA countries Week 36
Fatal cases EU/EFTA countries Week 37
Fatal cases EU/EFTA countries Week 38
Fatal cases EU/EFTA countries Week 39
Fatal cases EU/EFTA countries Week 40
Fatal cases EU/EFTA countries Week 41
Fatal cases EU/EFTA countries Week 42
Fatal cases EU/EFTA countries Week 43
Fatal cases EU/EFTA countries Week 44
Fatal cases EU/EFTA countries Week 45
Fatal cases EU/EFTA countries Week 46
Fatal cases EU/EFTA countries Week 47
Fatal cases EU/EFTA countries Week 48
Fatal cases EU/EFTA countries Week 49
Fatal cases EU/EFTA countries Week 50
Purpose of the visit • to exchange experience regarding pandemic influenza, as Bulgaria was increasingly affected by the pandemic • to review and discussion of measures taken to control the epidemic of pandemic influenza – based on mission check list prepared by ECDC influenza team and • planning of further actions and cooperation points
ECDC experts’ conclusions • The threat to health posed by the A(H1N1) pandemic influenza virus in Bulgaria does not substantially differ from that in other EU Member States. • The clinical pattern of disease appeared to be similar to that in other EU countries, with most affected people only experiencing mild illness. However, a number of people have been very seriously ill. • Bulgaria is well placed to respond to the 2009 A(H1N1) pandemic, though the plan had to be adapted to respond to the rapidly developing epidemiological situation.
Immediate measures taken by public health authorities in Bulgaria – activation of national and regional pandemic emergency operational units (centres) – daily reporting from regional to the national level required on the bed capacity and utilization, incidence rates, morbidity pattern and deaths, utilization and availability of antiviral in hospitals. – authoritative information about the pandemic virus was communicated to the public and health professionals - meetings with: hospital directors; directors of regional public health centres, emergency health care units, journalists and other relevant stake holders – clear clinical guidance has been elaborated, adapted and disseminated to different levels of medical care – morning filter in schools and closure of schools for one week – distribution of antivirals to regional centres and hospitals – changes in the legislation to facilitate vaccine and antiviral purchase agreements
Identified strengths of preparedness • Dedication and high level of expert knowledge of staff of the Department of Public Health and the National Center of Infectious and Parasitic Diseases working to address the rapidly developing epidemiological situation. • Availability of comprehensive pandemic plan and rapid adaptation of the plan to changing epidemiological situation. • Efforts to increase the AV availability and plans to distribute to Emergency Care centres. • Regional communicators were all trained in media relations prior to the pandemic. • Combined actions with the ministry of education – introduction of daily (morning) health checks and closure of schools. • Intensive discussions on vaccination policy and plans • Communication with international organizations (WHO, ECDC, European commission)
The main suggestions and advice of ECDC team for further actions: • monitoring epidemiological situation in the country for early signs of possible resurgence and / or possible second wave, • observing the number of influenza-related hospitalizations and deaths which may still be increasing for some period of time while ILI incidence may be going down, • planning and preparing vaccination campaigns, GPs can be used to help in identifying persons in risk groups. • reinforcing the communication to clinicians, especially GPs, and the public, about the need for early AV treatment (especially for those with underlying conditions predisposing to severe course of infection), • performing an overall evaluation of the impact of measures applied for the control of the pandemic may be considered by the Bulgarian PH authorities.
Further actions • Sharing experiences (ECDC advisory forum – 8 Dec; meeting in Bucharest – 15 Dec) • Elaboration and adaptation of vaccination plans – Pandemic vaccination – Seasonal influenza vaccination § Prepare and review plans for resource availability during holidays (X-mas and new year) – staff at central and local levels, primary and specialized health system preparedness – based on planning assumptions of international and local planning assumption § Continuous monitoring of the epidemiological situation
Observations and notes • The great importance of preliminary information from affected countries – risk groups, clinical manifestation, incidence rate and need for hospitalization, managing severe cases. • Massive panic among the population, despite the maximum transparency and openness or namely because of them. The borderline between good information awareness and psychosis is rather thin and easy to cross. • Need for external expert support – benefit from the reputation of the specialised international institutions. Nobody can be a prophet in his own land! • Emergency situations require emergency decisions! This also refers to the legislation, most of the procedures envisaged are slow and cumbersome and not apt for emergencies. • No matter how prepared you may be, there will always be things you have not prepared for. But, there is a positive touch, too – proposals which have been discussed for years are resolved very quickly in a time of crisis. Both the public and the politicians are much more open to health related issues.
Discussion issues • Unbalanced contracts for supply of pandemic vaccine. The current provisions assign plenty of responsibilities to the national authorities and only one right, i.e., the right to pay no matter what. I, personally, would not sign, nor would I advise the minister to sign under such a contract. • Long-term consequences of a pandemic. The public has only a certain amount of threats it can absorb and we are on the verge of exhausting it. This will inevitably cause problems with the future actions to improve the seasonal influenza vaccine coverage, for example, or with the preparedness to face other challenges related to public health. • Lack of a quick, reliable and effective mechanism for mutual support among EU member states. Practically, the only real support we received in response to our request for assistance with the supply of antivirals came from Austria and the WHO. Regardless of the long discussions, it has proved impossible to establish a virtual let alone a real community- wide stockpile of antivirals and vaccines. The common European procedure to deliver vaccines to several member states which was being drafted failed as well.
Recommend
More recommend