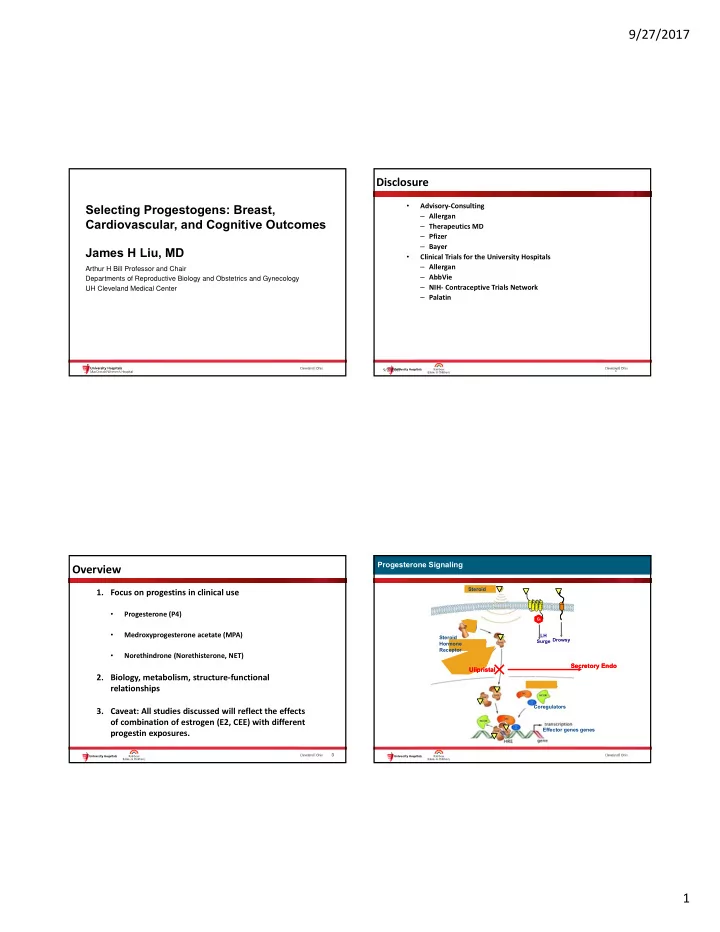
9/27/2017 Disclosure Selecting Progestogens: Breast, • Advisory ‐ Consulting – Allergan Cardiovascular, and Cognitive Outcomes – Therapeutics MD – Pfizer – Bayer James H Liu, MD • Clinical Trials for the University Hospitals – Allergan Arthur H Bill Professor and Chair – AbbVie Departments of Reproductive Biology and Obstetrics and Gynecology – NIH ‐ Contraceptive Trials Network UH Cleveland Medical Center – Palatin 9/27/2017 2 Progesterone Signaling Progesterone Signaling Overview Steroid 1. Focus on progestins in clinical use • Progesterone (P4) G i G i • Medroxyprogesterone acetate (MPA) LH Steroid Surge Drowsy Hormone Receptor • Norethindrone (Norethisterone, NET) Secretory Endo Secretory Endo Ulipristal Ulipristal 2. Biology, metabolism, structure ‐ functional relationships Coregulators 3. Caveat: All studies discussed will reflect the effects of combination of estrogen (E2, CEE) with different Effector genes genes progestin exposures. 3 1
9/27/2017 Structural Differences Among Progestins Oral Progesterone Intake and the First Pass Effect Progestins: Related But Distinct Agents CH 3 O CH 3 O C= O C= O OCCH 3 OCCH 3 C= CH O O O CH 3 Progesterone Norethindrone Medroxyprogesterone acetate acetate Oral progesterone metabolites i.e. 20- DHP4 results in drowsiness Deletion of the methyl group between rings A and B Addition of an ethinyl group at position 17 Bailey D G , Dresser G K CMAJ 2004;170:1531-1532 Oral Progesterone Metabolism: Off Target Effects Medroxyprogesterone acetate Metabolism O O O HO 3 HP 5 -reductase O O OH Progesterone H 5 P Breast MPA template structure is not broken by CYP3A4 during O 20 DHP Brain Sedation metabolism and binds as MP-acetate to progesterone receptors Zhang Drug Metabolism and Dispostion 2008;2292 2
9/27/2017 Minimal Dose of MPA Required for Endometrial Protection On Target Effects 200 D Cytosolic Estrogen Receptor Femtamoles/mg protein ± SEM ± SEM ENDOMETRIUM 100 200 * On Target Effects y=0.99 0.625 mg CEE † 100 FM/mgP B CEE +2.5 +5 +10 only MPA MPA MPA 0.3 mg 0.625 mg 1.25 mg CEE CEE CEE CEE = conjugated equine estrogen; MPA = medroxyprogesterone acetate. Gibbons WE et al. Am J Obstet Gynecol. 1986;154:456-461. 9 Suggested Progestin Doses Required For Secretory How Much Progestin is Sufficient? Changes in E-Primed Endometrium for 10-12 days A Simple Method for Determining the Optimal Dosage of Progestin Oral Progestin Dose Required in Post ‐ menopausal Women Receiving Estrogens Padwick ML, Pryse ‐ Medroxyprogesterone acetate 5-10 mg/d Davies J, Whitehead MI. NEJM 1986;315:930 ‐ 34 Micronized progesterone 200-300 mg/d “Regardless of the preparation and dosage of the ( cyclic ) estrogen Vaginal progesterone gel 45 mg/d* Drospirenone 0.25-1 mg/d* and progestin used, wholly or predominantly proliferative Norethindrone 0.35-1.0 mg/d endometrium was always associated with bleeding on or before day 75-150 g/d Norgestrel 10 after the addition of progestin; wholly or predominantly Dydrogesterone 10-20 mg/d secretory endometrium, or a lack of endometrial tissue was associated with bleeding on day 11 or later. “ King et al. Fertil Steril 1986;46(6):1062; Whitehead et al. Obstet Gynecol 1990;75(4):59S; * Other data 3
9/27/2017 Biology: Progesterone Effects on Gland Mitoses in Human Breast and Endometrium Are Different Endometrium BREAST On Target Effects Mitoses Off Target Effects Breast Off Target Effects 1 7 14 21 28 Cycle Days 14 T.A. Longacre et al. Am J. Surg Path, Vol.10 No. 6, 1986 WHI CEE+MPA: During Study and Follow-up Breast Cancer WHI CEE+MPA Trial: Mammography Results Increased Breast Density, Cysts % Abnormal* E+MPA Placebo Proportion Year 1 9.4 5.4 † Overall 31.5 21.2 † *Abnormal mammograms included those that were associated with recommendations for short-term follow-up, showed a suspicious abnormality, or were highly suggestive of malignancy † P < .001 vs E+P. Chlebowski RT, et al. JAMA . 2003;289:3243-53. Modified from Heiss et al. JAMA 2008;299:1036-45 16 9/27/2017 4
9/27/2017 WHI CEE+MPA Trial: Characteristics of No Increased Risk of Invasive Breast Invasive Breast Cancers Cancer in the WHI CEE-Alone Trial E+P Placebo (n = 199) (n = 150) P-Value Kaplan-Meier Estimate Tumor size, mean ± SD (cm) 1.7 ± 1.1 1.5 ± 0.9 .04 Positive lymph nodes, % 25.9 15.8 .03 0.05 Cumulative Proportion HR = 0.77 SEER stage, % 0.04 95% nCI = 0.59–1.01 Localized 74.6 82.7 Placebo Regional 24.4 14.0 .048 0.03 Metastatic 1.0 2.0 0.02 Morphology, grade, % CEE Well differentiated 25.0 20.3 0.01 Moderately differentiated 43.3 47.7 .61 0.00 Poorly 31.7 32.0 0 1 2 3 4 5 6 7 8 differentiated/anaplastic Time (years) SEER = Surveillance, Epidemiology, and End Results. Women ’ s Health Initiative Steering Committee. JAMA. 2004;291:1701-12. Chlebowski RT, et al. JAMA . 2003;289:3243-53. Summary: WHI Breast Cancer Results Summary: WHI Breast Cancer Results – CEE alone used for an average of 7 yrs did not increase – Breast cancers among women assigned to CEE+MPA breast cancer risk in women with prior hysterectomy 1 were somewhat larger and more likely to involve – CEE+MPA used for an average of 5 yrs was associated with regional lymph nodes a small increased risk of breast cancer in women without – Higher rate of abnormal mammograms prior hysterectomy 2 observed in women assigned to CEE+MPA • Increased risk was limited to those women with prior – Cannot make direct comparisons between the CEE ‐ HT use alone and CEE+MPA results – Absolute risk of breast cancer was low in both WHI trials, regardless of treatment assignment 1,2 • Study populations had important differences in baseline risk 1 Women's Health Initiative Steering Committee. JAMA. 2004;291:1701-12. 2 Chlebowski RT, et al. JAMA. 2003;289:3243-53. Chlebowski RT, et al. JAMA . 2003;289:3243-53. 5
9/27/2017 Breast Cancer Risk Among CEE+MPA Users in Randomized Controlled Trials Million Women Study – Investigators recruited 1,084,110 women in the UK, aged 50–64 years, between 1996 and 2001 WHI – Questionnaire about lifestyle, SES, medical history, and HT use sent in conjunction with invitation from NHSBSP for screening mammography HERS – Mean age, 56 years; 9364 cases of invasive breast cancer and 637 breast cancer deaths identified during follow-up HERS II – Analysis of HT and breast cancer risk restricted to postmenopausal women (n = 828,923) 0.5 1.0 2.0 10 – 50% were ever-users of HT; 33% were current users; mean duration of use was 5.8 years Relative Hazard (95% CI) Chlebowski RT, et al. JAMA . 2003;289:3243-53. SES = socioeconomic status; NHSBSP = National Health Service Breast Screening Programme. Hulley S, et al. JAMA . 2002;288:58-66. Million Women Study Collaborators. Lancet . 2003;362:419-27. Incident Invasive Breast Cancer in Current Users of E-only Preparations Incident Invasive Breast Cancer in Type of Estrogen? Relation to Recency and Type of HT Used Relative Risk E-only Formulation (95% CI)* All E-only formulations 1.30 (1.21–1.40) Relative Risk By constituent and dose HT Use at Baseline (95% FCI)* All equine estrogen 1.29 (1.16–1.43) All never-users 1.00 (0.96–1.04) ≤ 0.625 mg 1.25 (1.11–1.41) >0.625 mg 1.36 (1.14–1.61) All past users 1.01 (0.95–1.08) All 17 -estradiol 1.24 (1.12–1.37) Current users ≤ 1 mg 1.25 (1.12–1.40) >1 mg 1.19 (0.89–1.58) E-only 1.30 (1.22–1.38) By formulation E+P 2.00 (1.91–2.09) Oral 1.32 (1.21–1.45) Tibolone 1.45 (1.25–1.67) Transdermal 1.24 (1.11–1.39) Implanted 1.65 (1.26–2.16) Other/unknown types 1.44 (1.17–1.76) Dotted line represents overall relative risk for current users of estrogen-only preparations compared with 0.5 1.0 1.5 2.0 2.5 never-users at baseline. 0.5 1.0 1.5 2.0 FCI = floated CI. *Relative to never-users, stratified by age, time since menopause, parity and age at first birth, family history of breast *Relative to never-users, stratified by age, time since menopause, parity and age at first birth, family history of cancer, BMI, region, and deprivation index. breast cancer, body mass index, region, and deprivation index. Million Women Study Collaborators. Lancet . 2003;362:419-27. Million Women Study Collaborators. Lancet . 2003;362:419-27. 6
Recommend
More recommend