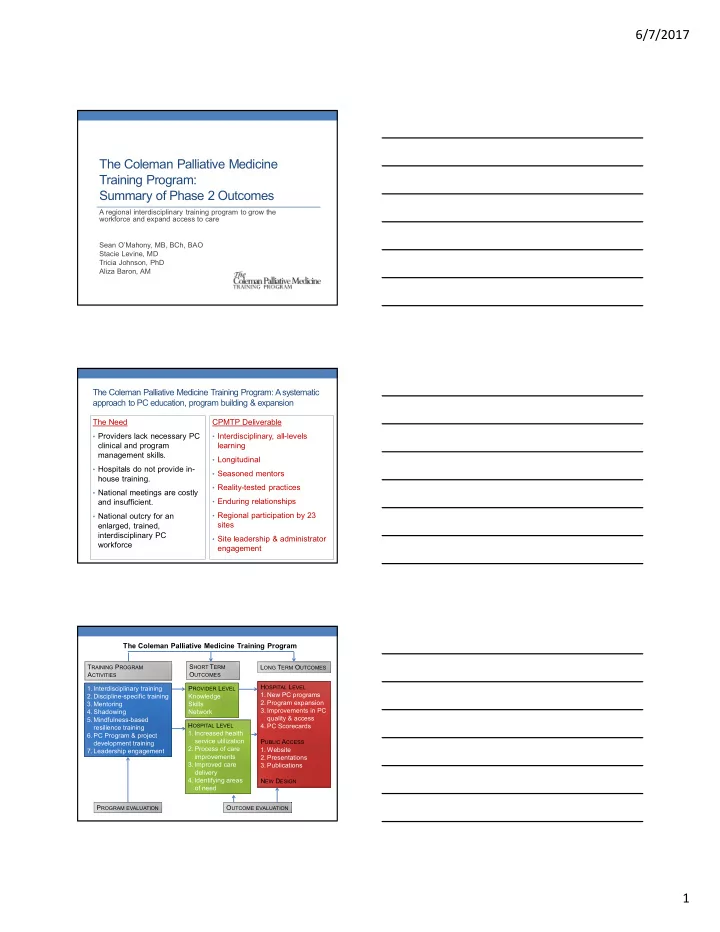
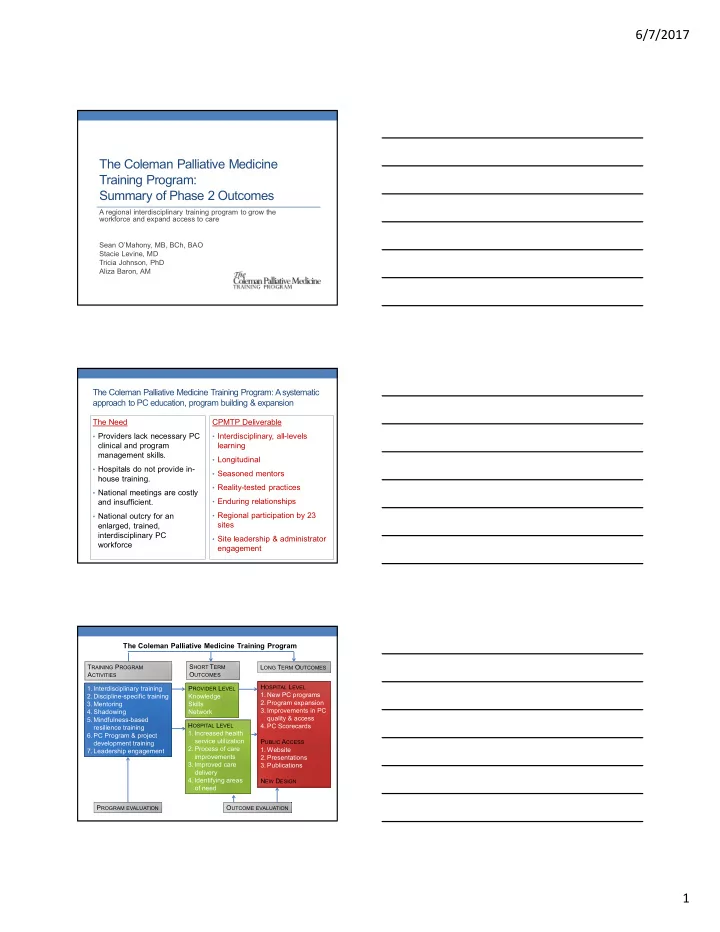
6/7/2017 The Coleman Palliative Medicine Training Program: Summary of Phase 2 Outcomes A regional interdisciplinary training program to grow the workforce and expand access to care Sean O’Mahony, MB, BCh, BAO Stacie Levine, MD Tricia Johnson, PhD Aliza Baron, AM 2 The Coleman Palliative Medicine Training Program: A systematic approach to PC education, program building & expansion The Need CPMTP Deliverable • Providers lack necessary PC • Interdisciplinary, all-levels clinical and program learning management skills. • Longitudinal • Hospitals do not provide in- • Seasoned mentors house training. • Reality-tested practices • National meetings are costly • Enduring relationships and insufficient. • National outcry for an • Regional participation by 23 sites enlarged, trained, interdisciplinary PC • Site leadership & administrator workforce engagement 3 The Coleman Palliative Medicine Training Program T RAINING P ROGRAM S HORT T ERM L ONG T ERM O UTCOMES A CTIVITIES O UTCOMES H OSPITAL L EVEL 1. Interdisciplinary training P ROVIDER L EVEL 1. New PC programs 2. Discipline-specific training Knowledge 2. Program expansion 3. Mentoring Skills 3. Improvements in PC 4. Shadowing Network quality & access 5. Mindfulness-based H OSPITAL L EVEL 4. PC Scorecards resilience training 1. Increased health 6. PC Program & project service utilization P UBLIC A CCESS development training 2. Process of care 1. Website 7. Leadership engagement improvements 2. Presentations 3. Improved care 3. Publications delivery 4. Identifying areas N EW D ESIGN of need P ROGRAM EVALUATION O UTCOME EVALUATION 1
6/7/2017 Overarching objectives Report system-level palliative medicine I. outcomes for organizations participating in the Coleman Palliative Medicine Training Program Products and dissemination II. Propose an updated program design , III incorporating 360 0 feedback from administrators, trainees, PC program directors and mentors 4 I. System-level palliative care outcomes 1. Enlarge the PC workforce with trained interdisciplinary providers 2. Increase patient and family access to palliative care services 3. Increase hospice utilization 4. Quantify the value of palliative care 5 6 1 Expand the trained workforce in PC “ As a new NP in “ This program PC, the program developed our was very front line team supportive and members to helped me see this as part grow … and also of their role... ” helped to facilitate Hiring at sites growth at my institution. ” Doubled guest 26 Fellows attendance at conferences 10 Junior Mentors 19 Nurses, ~ 30 administrators and PC 7 Chaplains team members attend each 5 Social Workers, conference 4 Physicians ~ 85 total per conference 1 Physician Assistant 2
6/7/2017 7 1 29 Core skills for nurses & physicians Skill Domains Differential diagnosis, pain management with opioids, non- Provide PC, dose opioids, opioids, adjuvant analgesics, & assess pain, assess non pharmacologics P AIN decisional capacity, give ASSESSMENT & bad news P EDIATRICS MANAGEMENT Nausea/vomiting, dyspnea, symptoms in actively dying N ON PAIN patients SYMPTOM E THICAL , MANAGEMENT LEGAL ISSUES Anxiety and Teach PC, team M ENTAL HEALTH depression leadership, delirium, spiritual P ROGRAM stakeholders ‘ buy-in, distress leverage resources, LEADERSHIP PC needs assessment, Support family of dying monitor benchmarks C OMMUNICATION patients, discuss prognosis, communicate bad news, SKILLS advance care planning, hospice care, explain PC 8 1 22 Core skills for PC social workers and chaplains Domains 5% 5% C OMMUNICATION 4% D IRECT PRACTICE 27% M ENTAL HEALTH 14% T EAM CARE L EADERSHIP / EXPERTISE 18% P ALLIATIVE BASICS 27% S PIRITUAL Program leadership & team-based skills improved significantly 1 in self-ratings, pre and post training Skills Confidence Performance ALL ALL Deliver teaching sessions in PC Lead or communicate effectively on an ALL ALL interdisciplinary team Describe to stakeholders how palliative care can enhance the mission and financial bottom line of an MED MED organization Leverage new and existing resources to build a MED palliative care program MED MED Conduct a needs assessment for PC Monitor performance improvement benchmarks MED Articulate role & function of chaplain or social worker SW & CH 9 3
6/7/2017 1 Significant improvements in leadership, program development and team skills in PC S OCIAL W ORKERS & N URSES , P HYSICIANS , C HAPLAINS PA • T EACH PC • T EACH PC • T EACH PC • T EACH PC • L EAD AN INTERDISCIPLINARY • L EAD AN INTERDISCIPLINARY • L EAD AN INTERDISCIPLINARY • L EAD AN INTERDISCIPLINARY TEAM TEAM TEAM TEAM • A RTICULATE ROLE AND • A RTICULATE ROLE AND • D ESCRIBE FINANCIAL BENEFITS • D ESCRIBE FINANCIAL BENEFITS FUNCTION OF SW AND FUNCTION OF SW AND OF PC TO STAKEHOLDERS OF PC TO STAKEHOLDERS CHAPLAIN CHAPLAIN • L EVERAGE RESOURCES TO • L EVERAGE RESOURCES TO BUILD A PC PROGRAM BUILD A PC PROGRAM • C ONDUCT A PC NEEDS • C ONDUCT A PC NEEDS ASSESSMENT ASSESSMENT • M ONITOR PERFORMANCE • M ONITOR PERFORMANCE BENCHMARKS BENCHMARKS 10 1 Metrics that matter: Extensive outreach & education to administrators • Multi-pronged: Conference sessions, 1-on-1 site teleconferences • Continuous from 2014 - present • Palliative Care Registry • Palliative Outcomes Study • Stated training program requirement • Carrot = stipend • Challenges and limitations included • staff turnover • mergers, new leadership • Variability in data tracking • Access to data 11 Palliative medicine team size increased or remained 1 stable over time for all but 1 community hospital 8 7 6 5 FTEs 4 3 2 1 0 2012 2014 2015 2016 Hospital 8 Hospital 20 Hospital 10 Hospital 21 Hospital 18 Hospital 25 Hospital 2 Hospital 11 4
6/7/2017 Palliative medicine team size increased or remained 1 stable over time for all but 1 teaching hospital 20 15 FTEs 10 5 0 2012 2014 2015 2016 Hospital 24 Hospital 22 Hospital 3 Hospital 27 Hospital 6 Hospital 9 Hospital 4 Hospital 5 Hospital 1 Hospital 14 In aggregate, the number of trained palliative medicine 1 clinicians increased substantially For the 19 organizations reporting For the 6 organizations reporting 2012 – staffing data for 2012 to 2015: 2016 staffing data: +92% +94% +12% 98 94 30.39 27.11 26.37 51 15.65 2012 2014 2015 2012 2014 2015 2016 14 Palliative medicine team teams were highly 1 interprofessional (2015) 12 10 Chaplain SW Nurse APN 8 Physician FTEs 6 4 2 0 5
6/7/2017 Programs grew substantially during the fellowship 1 program 350% Overall FTE Growth During the Coleman Program 300% 250% 200% 150% 100% 50% 0% -50% Programs grew substantially during the fellowship 1 program 100% Annualized FTE Growth During the Coleman Fellowship Program 80% 60% 40% 20% 0% 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 -20% 17 7 programs met the CAPC guidelines for an 1 interdisciplinary palliative care team 10 Chaplain 9 SW 8 Nurse 7 APN 6 Physician 5 4 3 2 1 0 Hospital 5 Hospital 9 Hospital 7 Hospital 25 Hospital 6 Hospital 10 Hospital 23 Of the programs that didn’t meet team criteria, 31% were missing a physician, 13% missing an APRN or RN, 63% missing a SW, and 88% missing a chaplain. 6
6/7/2017 INCREASE PATIENT AND FAMILY ACCESS TO PALLIATIVE CARE SERVICES Practice Improvement Projects Growth in Staffing Growth Patient Volume 19 20 Practice improvement projects aimed to improve 2 quality and access to palliative care Multi-modal training prepared trainees to create and implement effective O NE - ON - ONE projects MENTORING D ISCIPLINE - SPECIFIC PROJECT CONSULTATION I NTERDISCIPLINARY GROUP CONSULTATION C ONFERENCE EDUCATION – QUALITY STANDARDS , METRICS THAT MATTER , INTENT TO CHANGE CONTRACTS 2 Regional reach of the training program P HASE 1 20 SITES 2013 - 2015 29 SITES TOTAL 14 - C ONTINUOUS PARTICIPATION P HASE 2 2013 – 2017 22 SITES 2015 – 2017 (8 NEW ) 21 7
6/7/2017 22 23 participating sites and 36 interdisciplinary 2 PC champions 18 16 16 14 12 12 Participating Sites 10 10 9 Fellows & Jr. Mentors 8 6 4 4 4 2 2 2 0 T EACHING C OMMUNITY O UTPATIENT S AFETY N ET H OSPITALS H OSPITALS C LINICS H OSPITALS 23 2 30 Projects implemented at 35 practice settings P ROJECT REQUIREMENTS : 18 17 MEETS A NEED INSTITUTIONAL SUPPORT 16 14 MEASURABLE OUTCOMES 14 2- YR . TIMELINE COMPATIBLE WITH JOB 12 RESPONSIBILITIES 10 8 6 4 2 2 1 1 0 I NPATIENT O UTPATIENT H OME PC N URSING H OME HOME HOSPICE 24 2 Multiple, diverse project outcomes I NCREASED PATIENT ACCESS TO CARE 13 PROJECTS I MPROVED I DENTIFYING HEALTH SERVICE AREAS OF NEED UTILIZATION 13 PROJECTS 3 PROJECTS P ROCESS OF C ARE DELIVERY CARE IMPROVEMENTS IMPROVEMENTS 11 PROJECTS 8 PROJECTS 8
Recommend
More recommend