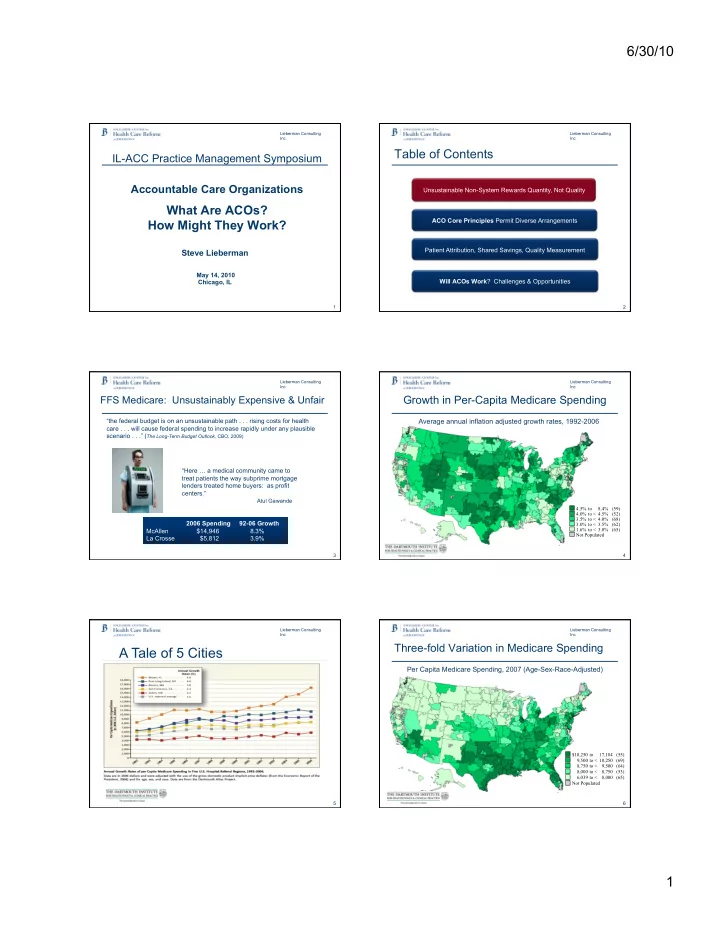
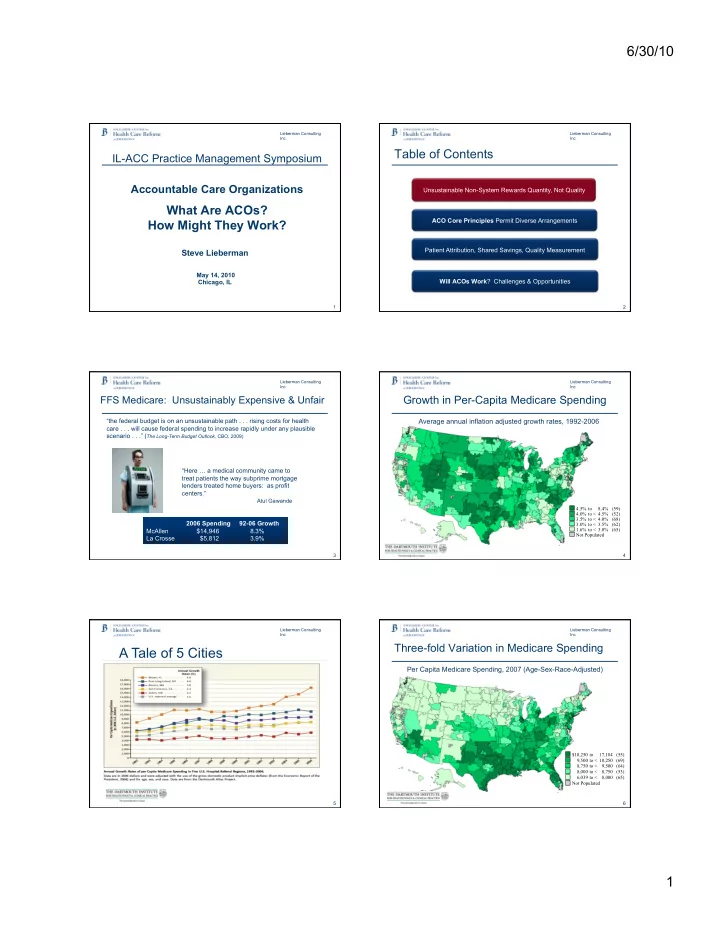
6/30/10 Lieberman Consulting Lieberman Consulting Inc Inc Table of Contents IL-ACC Practice Management Symposium Accountable Care Organizations Unsustainable Non-System Rewards Quantity, Not Quality What Are ACOs? ACO Core Principles Permit Diverse Arrangements How Might They Work? Patient Attribution, Shared Savings, Quality Measurement Steve Lieberman May 14, 2010 Chicago, IL Will ACOs Work ? Challenges & Opportunities 1 2 Lieberman Consulting Lieberman Consulting Inc Inc Growth in Per-Capita Medicare Spending FFS Medicare: Unsustainably Expensive & Unfair “the federal budget is on an unsustainable path . . . rising costs for health Average annual inflation adjusted growth rates, 1992-2006 care . . . will cause federal spending to increase rapidly under any plausible scenario . . .” ( The Long-Term Budget Outlook, CBO, 2009) “Here … a medical community came to treat patients the way subprime mortgage lenders treated home buyers: as profit centers.” Atul Gawande 4 .5% to 8 .4% (59) 4 .0% to < 4 .5% (52) 3 .5% to < 4 .0% (68) 2006 Spending 92-06 Growth 3 .0% to < 3 .5% (62) 1 .6% to < 3 .0% (65) McAllen $14,946 8.3% Not Populated La Crosse $5,812 3.9% 3 4 Gawande, Atul. The Cost Conundrum: What a Texas town can teach us about health care. The New Yorker, June 1, 2009 Lieberman Consulting Lieberman Consulting Inc Inc Three-fold Variation in Medicare Spending A Tale of 5 Cities Per Capita Medicare Spending, 2007 (Age-Sex-Race-Adjusted) $10,250 to 17,184 (55) 9,500 to < 10,250 (69) 8,750 to < 9,500 (64) 8,000 to < 8,750 (53) 6,039 to < 8,000 (65) Not Populated Source: Slowing the Growth of Health Care Spending: Lessons from Regional Variation Fisher, Skinner, Bynum, New England Journal of Medicine, February 26, 2009 5 6 1
6/30/10 Lieberman Consulting Lieberman Consulting Inc Inc What do higher spending regions get? What do higher spending regions get? Patient-Perceived Physician’s Health Outcomes Trends Over Time Perceptions Quality Worse communication Worse access to primary Greater growth in per Slightly higher mortality among physicians care capita resource use Greater difficulty ensuring continuity Lower overall rating of medical care Lower gains in survival following AMI Lower satisfaction with career Lower satisfaction with hospital care (1) ¡Fisher ¡et ¡al. ¡Ann ¡Intern ¡Med: ¡2003; ¡138: ¡273-‑298 ¡ ¡ (2) ¡Baicker ¡et ¡ ¡al. ¡Health ¡Affairs ¡web ¡exclusives, ¡October ¡ ¡7, ¡2004 ¡ (3) ¡Fisher ¡et ¡al. ¡Health ¡Affairs, ¡web ¡exclusives, ¡Nov ¡16, ¡2005 ¡ (4) ¡Skinner ¡et ¡al. ¡Health ¡Affairs ¡web ¡exclusives, ¡Feb ¡7, ¡2006 ¡ (5) ¡Sirovich ¡et ¡al ¡Ann ¡Intern ¡Med: ¡2006; ¡144: ¡641-‑649 ¡ (6) ¡Fowler ¡et ¡al. ¡JAMA: ¡299: ¡2406-‑2412 ¡ 7 8 Lieberman Consulting Lieberman Consulting Inc Inc Variations in Preference Sensitive Care Variations by Types of Care: Evidence-Based Care More Care in High More Care in High Spending Regions 2.0 Sending Regions 2.0 1.0 1.0 Preference Sensitive Care Evidence-Based Evidence-Based Less Care in High Less Care in High Quality Quality Spending Regions Spending Regions 0.5 0.5 Includes ¡Rates ¡of: ¡ ¡ Includes ¡rates ¡of: ¡ Mammogram, ¡Women ¡65-‑69 ¡ ¡Pap ¡Smear, ¡Women ¡65+ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ Total ¡Hip ¡Replacement ¡Total ¡Knee ¡Replacement ¡ Pneumococcal ¡ImmunizaYon ¡ ¡ ¡ ¡Aspirin ¡at ¡admission ¡(Heart ¡aZack) ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¡ Back ¡Surgery ¡ ¡CABG ¡Following ¡Heart ¡AZack ¡ 9 10 Lieberman Consulting Lieberman Consulting Inc Inc Variation in Supply Sensitive Care Preference Sensitive Care Varies in ALL Regions 14.0 Rate of Coronary Artery Bypass Each red dot Graft Surgery represents a Hospital More Care in High Age-sex-race adjusted, 2001 Referral Region 12.0 Spending Regions (HRR) 2.0 Rate per 1000 Enrollees 10.0 Each red dot represents a 8.0 Hospital 1.0 Referral Supply Preference Region (HRR) 6.0 Sensitive Care Sensitive Care Evidence-Based 4.0 Less Care in High Quality Spending Regions 0.5 2.0 Q1 Q2 Q3 Q4 Q5 Includes ¡rates ¡of: ¡ N.B. ¡Self-‑reported ¡health ¡ InpaYent ¡Days ¡ ¡InpaYent ¡Days ¡in ¡the ¡ICU ¡ status ¡& ¡income ¡explain ¡ HRRs by Spending Quintile Imaging ¡& ¡DiagnosYc ¡Tests ¡EvaluaYon ¡& ¡Management ¡Visits ¡ about ¡25% ¡of ¡variaYon ¡ 11 12 2
6/30/10 Lieberman Consulting Lieberman Consulting Inc Inc Comparison of Different Payment Models Table of Contents FFS Capitation ACO Payment Providers are revenue With fixed payments unrelated Moderating incentives, Unsustainable Non-System Rewards Quantity, Not Quality centers rewarded for to volume, providers are cost shared savings balances increased volume centers rewarded for “stinting” incentives of FFS & capitation ACO Core Principles Permit Diverse Arrangements Patients Neither assigned nor Enrolled with specific provider Assigned based on previous enrolled care patterns Patient Attribution, Shared Savings, Quality Measurement Primary care & Little reward for Supports primary care and care Support s primary care and care coordination primary care or care coordination care coordination coordination Will ACOs Work ? Challenges & Opportunities Accountability for Weak incentives to Strong accountability for per- Accountability for costs. per-capita costs & manage per-capita capita cost but no link to quality Links shared savings to quality costs or improve quality meeting quality measures 13 14 Lieberman Consulting Lieberman Consulting Inc Inc Accountability, “Systemness” & Incentives ACOs Differ But Share a Few, Key Elements Core Principles Key Design Elements 1 2 3 Achieve better health, better quality & Pay for better value: improve lower costs for patients and communities overall health & reduce costs Are of a Tools : timely feedback to providers Better information that engages Can provide or manage Are capable of sufficient size continuum of care as a internally physicians, supports improvement, and Reporting : require utilization and to support real or virtually distributing informs consumers quality data from providers comprehensive integrated delivery shared savings performance system payments measurement Establish robust HIT infrastructure New model: It’s the system - Establish organizations accountable for aims and Implement cost-saving and quality- capable of redesigning practice and improving medical interventions Important Caveats managing capacity Evaluate performance of systems • ACOs are not gatekeepers Restructure payment incentives to Realign incentives – both financial and • ACOs do not require changes to benefit structures avoid extremes of FFS “revenue clinical – to support accountability for • ACOs do not require patient enrollment centers” & capitation “cost centers” costs and quality across care settings 15 16 Lieberman Consulting Lieberman Consulting Inc Inc Quality Measures Will Evolve Over Time: Performance Payment Framework Beginning, Intermediate, & Advanced Stages ACOs offer a wide range of approaches Multiple priorities, outcome-oriented, and span the continuum of care Level 1 Level 2 Level 3 Asymmetric shared-savings Symmetric Model Partial Capitation Model Beginning Intermediate Advanced ACO receives mix of FFS and Continue operating under Payments can still be tied • ACOs have access to • ACOs use specific clinical • ACOs use more complete prospective fixed payment current insurance contracts/ to current payment system, medical, pharmacy, and data (e.g., electronic clinical data (e.g., coverage models (e.g., FFS) although ACO could receive If successful at meeting laboratory claims from laboratory results) and electronic records, revenue from payers and budget and performance No risk for losses if spending payers (claims-based limited survey data registries) and robust distribute funds to targets, greater financial exceeds targets members (depending on measures) patient-generated data benefits • More sophisticated HIT Most incremental approach ACO contracts) (e.g., Health Risk If ACO exceeds budget, more • Relatively limited health infrastructure in place with least barriers for entry Appraisals, functional At risk for losses if spending risk means greater financial infrastructure • Greater focus on full status) Attractive to new entities, exceeds targets downside • Limited to focusing on spectrum of care risk-adverse providers, or Increased incentive for • Well-established and Only appropriate for providers entities with limited primary care services providers to decrease costs with robust infrastructure, robust HIT infrastructure organizational capacity, range (starter set of measures) due to risk of losses demonstrated track record in of covered services, or • Focus on full spectrum of finances and quality and experience working with Attractive to providers with care and health system providing relatively full range other providers some infrastructure or care of services priorities coordination capability and demonstrated track record 17 18 3
Recommend
More recommend