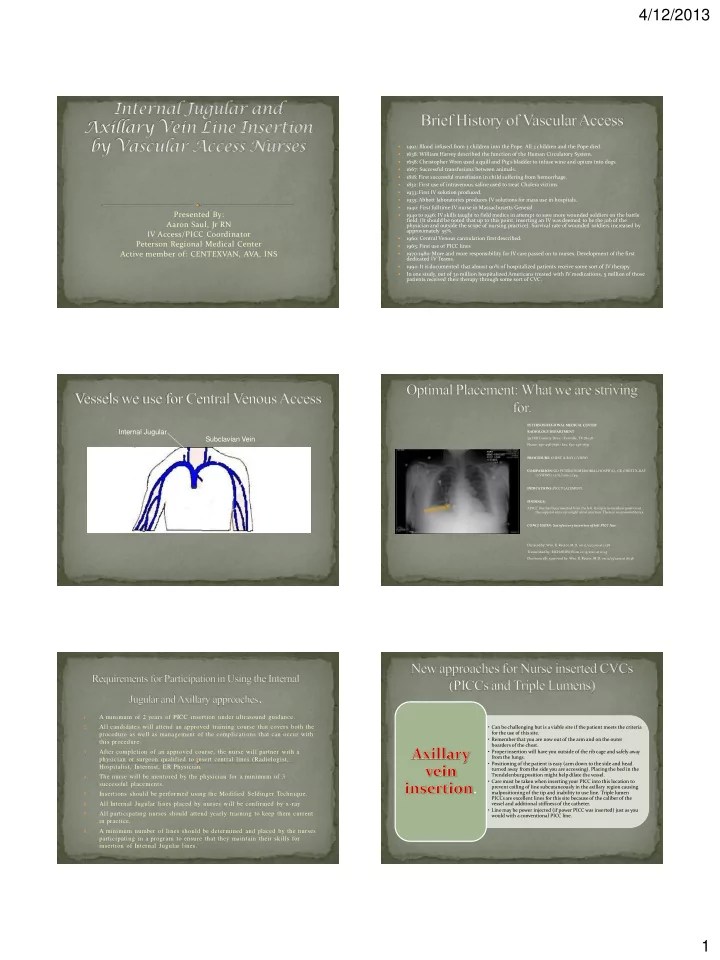
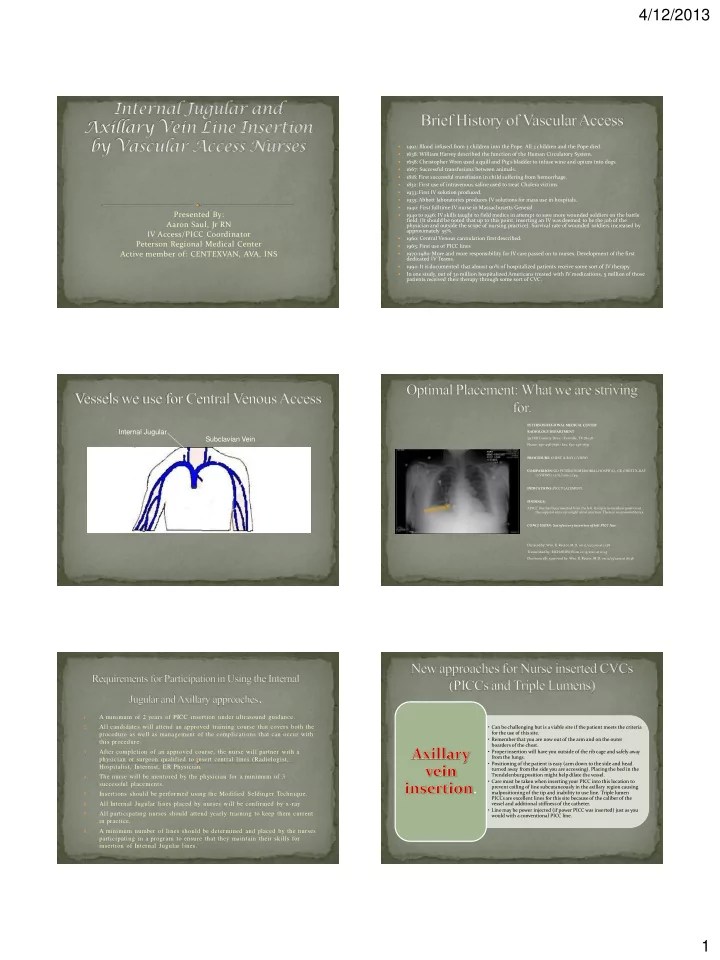
4/12/2013 1492: Blood infused from 3 children into the Pope. All 3 children and the Pope died. 1638: William Harvey described the function of the Human Circulatory System. 1658: Christopher Wren used a quill and Pig’s bladder to infuse wine and opium into dogs. 1667: Successful transfusions between animals. 1818: First successful transfusion in child suffering from hemorrhage. 1832: First use of intravenous saline used to treat Cholera victims 1933: First IV solution produced. 1935: Abbott laboratories produces IV solutions for mass use in hospitals. 1940: First fulltime IV nurse in Massachusetts General. Presented By: 1940 to 1946: IV skills taught to field medics in attempt to save more wounded soldiers on the battle field. (It should be noted that up to this point, inserting an IV was deemed to be the job of the Aaron Saul, Jr RN physician and outside the scope of nursing practice). Survival rate of wounded soldiers increased by approximately 55%. IV Access/PICC Coordinator 1960: Central Venous cannulation first described. Peterson Regional Medical Center 1965: First use of PICC lines Active member of: CENTEXVAN, AVA, INS 1970-1980: More and more responsibility for IV care passed on to nurses. Development of the first dedicated IV Teams. 1990: It is documented that almost 90% of hospitalized patients receive some sort of IV therapy. In one study, out of 30 million hospitalized Americans treated with IV medications, 5 million of those patients received their therapy through some sort of CVC. PETERSON REGIONAL MEDICAL CENTER Internal Jugular RADIOLOGY DEPARTMENT Subclavian Vein 551 Hill Country Drive • Kerrville, TX 78028 Phone: 830-258- 7636 • Fax: 830 -258-7657 Axillary Vein External Jugular PROCEDURE: CHEST X-RAY (1 VIEW) Cephalic Vein COMPARISON: SID PETERSON MEMORIAL HOSPITAL, CR, CHEST X-RAY (2 VIEWS), 12/12/2010, 11:49. INDICATIONS: PICC PLACEMENT Basilic Vein FINDINGS: A PICC line has been inserted from the left. Its tip is in excellent position at Brachial Vein the superior vena cava/right atrial junction. There is no pneumothorax. CONCLUSION: Satisfactory insertion of left PICC line. Dictated by: Wm. R. Rector, M.D. on 12/13/2010 at 11:58 Transcribed by: RICHARDSON on 12/13/2010 at 12:43 Electronically approved by: Wm. R. Rector, M.D. on 12/13/2010 at 16:36 A minimum of 2 years of PICC insertion under ultrasound guidance. 1. 2. All candidates will attend an approved training course that covers both the • Can be challenging but is a viable site if the patient meets the criteria for the use of this site. procedure as well as management of the complications that can occur with • Remember that you are now out of the arm and on the outer this procedure. boarders of the chest. After completion of an approved course, the nurse will partner with a 3. • Proper insertion will have you outside of the rib cage and safely away from the lungs. physician or surgeon qualified to insert central lines (Radiologist, • Positioning of the patient is easy (arm down to the side and head Hospitalist, Internist, ER Physician. turned away from the side you are accessing). Placing the bed in the Trendelenburg position might help dilate the vessel. 4. The nurse will be mentored by the physician for a minimum of 3 • Care must be taken when inserting your PICC into this location to successful placements. . prevent coiling of line subcutaneously in the axillary region causing malpositioning of the tip and inability to use line. Triple lumen Insertions should be performed using the Modified Seldinger Technique. 5. PICCs are excellent lines for this site because of the caliber of the All Internal Jugular lines placed by nurses will be confirmed by x-ray. 6. vessel and additional stiffness of the catheter. • Line may be power injected (if power PICC was inserted) just as you 7. All participating nurses should attend yearly training to keep them current would with a conventional PICC line. in practice. 8. A minimum number of lines should be determined and placed by the nurses participating in a program to ensure that they maintain their skills for insertion of Internal Jugular lines. 1
4/12/2013 Axillary Vein Insertion Candidates: 1. Thorough venous assessment with ultrasound of the patient should be performed on bilateral extremities to indeed identify that there are no usable vessels for traditional PICC Patients with a long history of numerous PICC insertions in insertion. both upper extremities and require venous access for Thorough history of any vascular access is very important as this will dictate which vessel 2. (right or left) will be attempted. treatment in a non-emergent situation. The patient’s chest mass must be taken into account. For example patient of my mass 3. would not be a very viable candidate for an axillary PICC (without a harpoon). Patients that are unable to position their arm for PICC 4. As with PICC lines, the presence of medical devices (i.e. pacemakers or history of a insertion. (Patients that have severe arthritis, rotator cuff pacemaker) again should be considered because of the stenosis caused by insertion of the wires into the subclavian vein. problems, shoulder replacements, other conditions). It should be noted that this should not be your first stop if at all possible and your 5. Patients that require venous access but have no vessels in the assessment of the patient should dictate how to best proceed. 6. Once you have selected your site, vessel entry should be performed again using the upper extremities of suitable size for cannulation until Modified Seldinger Technique with a micorpuncture kit (this consists of using a 21 ga reaching the level of the axillary vein. needle to access the vessel and wiring the vessel for purchase with a 0.018 wire). Obtain a chest xray to both confirm placement and ensure that there is no pneumothorax. 7. Left Clavicle Right Clavicle =Brachial Artery =Axillary Vein =Axillary Vein =Brachial Artery Approximate boarder of the rib cage Axillary fold Lower boarder of the clavicle General area of axillary vein 2
4/12/2013 Pectoral Muscle 1. Again, thorough venous assessment with ultrasound is of the utmost importance to identify the underlying structures at your proposed site of insertion. If separation of the Internal Jugular and Carotid is difficult or problematic, move to the other side to avoid inadvertently accessing the Carotid artery. The right Internal Jugular vein should be your first choice because it is a “straight shot” 2. • This is a big jump in practice. Remember, it’s not if you have a into the SVC to the Cavoatrial junction. The left Internal Jugular can be used but me complication; IT’S WHEN. mindful of the abrupt angle it takes when it joins the brachiocephalic vein crossing the chest. (Accidental perforation can occur when dilating up to insert your catheter). • Very intricate yet very simple site for insertion. • Again patient positioning is straight forward (head away from 3. Proper insertion should be as close to the base of the neck to ensure, in most cases, safe positioning of the Internal Jugular from the Carotid artery. side being accessed and Trendelenburg the bed). • With this site, air embolism is a VERY real danger, remember 4. Access is best achieved, if not emergent, by again using a micropuncture kit and the Modified Seldinger Technique so that if the Carotid artery is hit, you are not dealing with a what you need to do if this occurs (besides the expletive that 14 ga hole but instead with a 21 ga hole. will creep out under your breath and behind the mask). If emergent, use great care with the 14 ga needle and perform the procedure as you would • These lines are excellent for the patient that requires CVP 5. normally (MST). monitoring in the ICU. 6. To help avoid the development of a hematoma, take the patient out of Trendelenberg as • This is not a suitable site for the insertion of PICC lines. soon as you have the catheter in place. (External jugular insertion of PICC lines is still being If possible, suture the catheter down to the collar bone ensuring that you have a gentle considered at this time and is actually being performed in some 7. curve in the catheter. facilities across the country). Again obtain a chest xray to both confirm placement and ensure that there is no 8. pneumothorax. 3
4/12/2013 Approximate region of where the IJ and Carotid run The patient has limited selections for venous access. Upper extremity co- Upper boarder of the Clavicle 1. morbidities preclude PICC placement. The patient needs access in a more emergent situation. 2. 3. Patients that need the most accurate CVP monitoring possible. 4. Patients that will require large volumes of fluid and/or blood products Boarder of the Sternocleidomastoid muscle (e.g. septic patients, GI bleeds, patients in cardiogenic shock (s/p cardiac arrest)). 5. Patients with CKD. Patients with known coagulopathies may not be candidates for this 6. procedure. (Platelet count of less that 50,000 or an elevated INR). Any other patient that you think would benefit from have a large bore 7. central line for treatment of their condition. 6.3% of time 4.2% of time 75.5% of time 71.4% of time 12 o’clock 12 o’clock 10 o’clock 2 o’clock 16.4% of time 9% of time 9% of time 9% of time 9 o’clock 1 o’clock 11 o’clock 3 o’clock =Carotid Artery =Internal Jugular Vein =Carotid Artery =Internal Jugular Vein 4
Recommend
More recommend