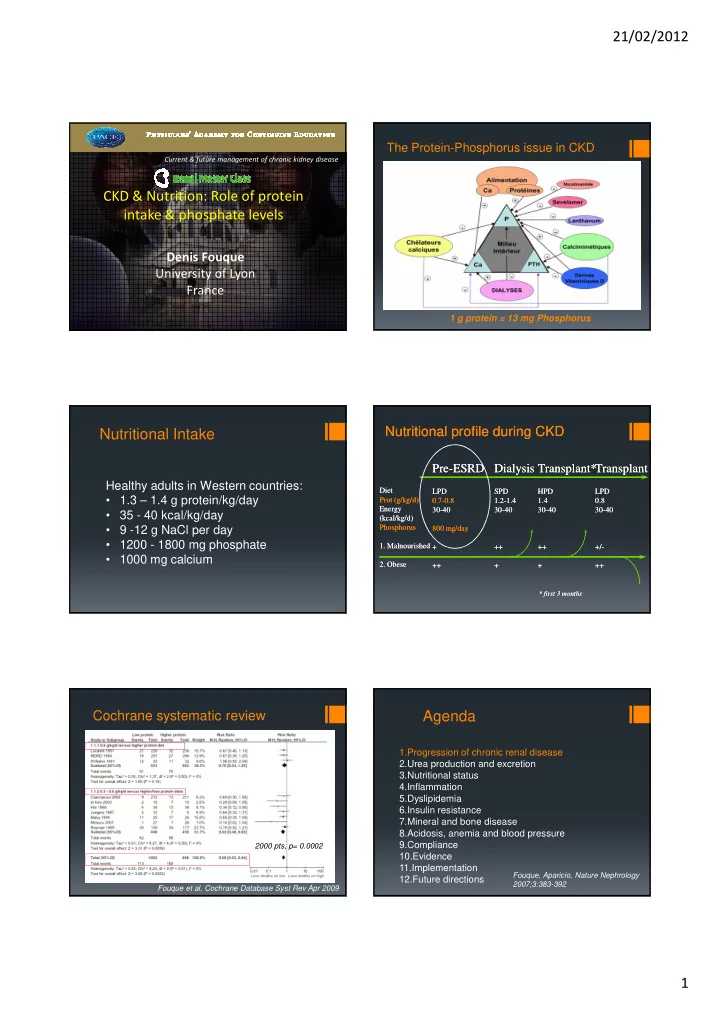
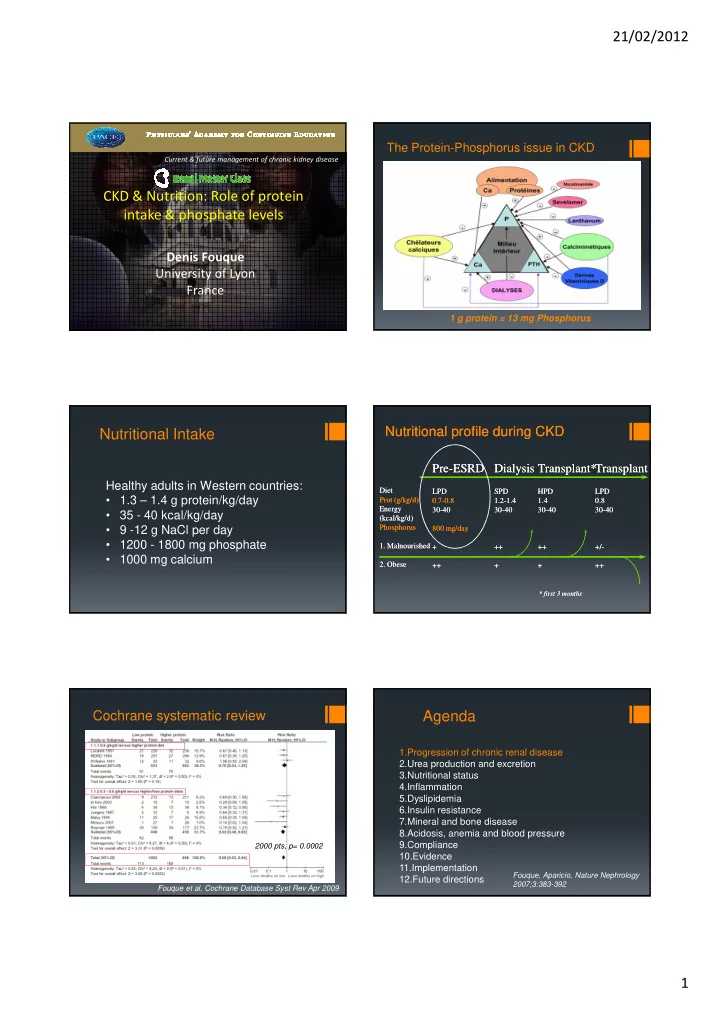
21/02/2012 The Protein-Phosphorus issue in CKD Current & future management of chronic kidney disease CKD & Nutrition: Role of protein intake & phosphate levels Denis Fouque University of Lyon France 1 g protein = 13 mg Phosphorus Nutritional profile during CKD Nutritional profile during CKD Nutritional Intake Pre-ESRD Pre ESRD Dialysis Dialysis Transplant* Transplant* Transplant Transplant Healthy adults in Western countries: Diet Diet LPD LPD SPD SPD HPD HPD LPD LPD • 1.3 – 1.4 g protein/kg/day Prot Prot (g/kg/d) (g/kg/d) 0.7- 0.7 -0.8 0.8 1.2- 1.2 -1.4 1.4 1.4 1.4 0.8 0.8 Energy Energy 30- 30 -40 40 30- 30 -40 40 30- 30 -40 40 30- 30 -40 40 • 35 - 40 kcal/kg/day (kcal/kg/d) (kcal/kg/d ) • 9 -12 g NaCl per day Phosphorus Phosphorus 800 mg/day 800 mg/day • 1200 - 1800 mg phosphate 1. Malnourished 1. Malnourished + ++ ++ ++ ++ +/ +/- - • 1000 mg calcium 2. Obese 2. Obese ++ ++ + + + + ++ ++ * first 3 months * first 3 months Cochrane systematic review Agenda 1.Progression of chronic renal disease 2.Urea production and excretion 3.Nutritional status 4.Inflammation 5.Dyslipidemia 6.Insulin resistance 7.Mineral and bone disease 8.Acidosis, anemia and blood pressure 2000 pts, p= 0.0002 9.Compliance 10.Evidence 11.Implementation Fouque, Aparicio, Nature Nephrology 12.Future directions 2007;3:383-392 Fouque et al, Cochrane Database Syst Rev Apr 2009 1
21/02/2012 Reducing Protein intake Nephroprotection � Fundamental experimental work of Brenner, Hostetter 0.3 g prot/kg + ceto-analogs Proteinuria and colleagues � More difficult to be confirmed in humans: Serum albumin � Men are not rats � Multifactorial disease � Less protein gradient � Clinical trials caveats (eg, duration, speed of progression, various renal disease, interference with outcome measures, compliance) � Surrogate: proteinuria ++ Aparicio et al, Nephron 1988 Proportionate reduction in protein intake VLPD reduces Proteinuria better than LPD and proteinuria • VLPD + KA (0.3 g/kg/d) / LPD (0.6 g/kg/d) / Free Diet • Parallel reduction in Protein intake and Sodium intake Proteinuria (g/d) Baseline protein intake ≥ 1 g/kg/day Gansevoort et al, NDT 1992 Bellizzi et al, Kidney Int 2007 Protein intake induces renal inflammation Protein intake induces renal pathology Rats fed 2 different sources and 3 different levels of protein for 2 months casein 45% 30% 20% Proteinuria 186 ±23 248 ±32 141 ±42 * Urine H 2 O 2 (mg/day) S insulin 14.6 ±1.9 12.0 ±1.4 11.7 ±1.9 * Renal expression Lipids casein 45% 30% 20% SREBP1 2.2 ±0.2 2.2 ±0.2 1.0 ±0.2 * TNF-alpha 3.5 ±0.6 2.7 ±0.4 1.1 ±0.3 * inflam IL-6 2.1 ±0.3 2.0 ±0.2 1.0 ±0.1 * mation IV collagen 1.65 ±0.2 2.0 ±0.3 1.0 ±0.2 * Oxidant stress Mesangial cell proliferation TGF-beta 1.9 ±0.2 1.4 ±0.2 1.0 ±0.1 * Tovar-Palacio et al, Am J Physiol fibrosis Tovar-Palacio et al, Am J Physiol 2011 300:F263 Matrix expansion 2011 300:F263 2
21/02/2012 LPD reduces renal inflammation Ketoacids reduces renal fibrosis 5/6 Nx rats followed for 8 months Protein intake: 22% - 6% - 5% +1%KA Fibronectin staining Kruppel-like factor 15 (KLF15): antifibrotic transcription factor Gao X et al, Kidney Int 2011 79:987 Gao X et al, Kidney Int 2011 79:987 LPD – KA reduce renal matrix accumualation Overexpression of KLF15 and renal inflammation Renal TGF beta and collagen expression Gao X et al, Kidney Int 2011 79:987 Gao X et al, Kidney Int 2011 79:987 Transfected mesangial cells LPD restores renal KLF15 expression The role of Klotho on vascular calcifications WT Kl-/- Kl-/- +LPD Kl-/- + sevel Gao X et al, Kidney Int 2011 79:987 Ohkido et al. ASN 2011 3
21/02/2012 Agenda 1.Progression of chronic renal disease Reduction in serum urea nitrogen 2.Urea production and excretion 3.Nutritional status 4.Inflammation 5.Dyslipidemia 6.Insulin resistance 7.Mineral and bone disease 8.Acidosis, anemia and blood pressure 9.Compliance 10.Evidence 11.Implementation 12.Future directions Agenda After 3 months at 0.3 g/kg/d + ketoanalogues 1.Progression of chronic renal disease 2.Urea production and excretion 3.Nutritional status and safety 4.Inflammation 5.Dyslipidemia 6.Insulin resistance 7.Mineral and bone disease 8.Acidosis, anemia and blood pressure 9.Compliance 10.Evidence 11.Implementation 12.Future directions Rigalleau et al. Am J Clin Nutr 1997 Optimal Protein Intake Aminoacid oxidation after reducing protein intake From 1.1 to 0.7 g/kg/day during three months Minimal intake 0.46 g/kg/d (FAO/WHO, RDA) +30% for mixed protein = 0.60 +30% for safety (at population level ) = 0.80 in CKD patients: 0.6-0.7 0.6-0.7 • Nitrogen balances (Kopple) g/kg/d g/kg/d • Leucine fluxes (Maroni, Fouque) • Metabolic analyses (Aparicio) (bone, CV risk, acidosis, proteinuria, insulinoresistance…) Bernhard et al, J Am Soc Nephrol 2001 4
21/02/2012 Urinary urea excretion (mmol/d) Serum albumin in the MDRD study MDRD study A Mild CKD from 1.1 to 0.7 g prot/kg/d MDRD study B Severe CKD Fouque et al. J Am Soc Nephrol 1995 Kopple et al, Kidney Int 1997 Nutritional intake after the start of Dialysis Nutritional status after the start of dialysis DEXA FM Protein intake No difference No difference whatever the whatever the predialysis diet predialysis diet LBM Energy intake Vendrely et al. Kidney Int 2003 Vendrely et al. Kidney Int 2003 Agenda Low protein diet and inflammation 1.Progression of chronic renal disease • 17 males, non diabetic, mild proteinuria and CKD 2.Urea production and excretion st III (39 ml/min) 3.Nutritional status • 4 month at 0.68 g prot/kg/day (free protein intake 4.Inflammation before) 5.Dyslipidemia • 3 day diet records - same dietician 6.Insulin resistance 7.Mineral and bone disease No weight change - no change in BMI or body fat 8.Acidosis, anemia and blood pressure 9.Compliance S urea to drop from 14.5 to 10.6 mmol/l (- 27 %, 10.Evidence 11.Implementation <0.001) 12.Future directions Kozlowska et al, Nephrology 2004 5
21/02/2012 Agenda Low protein diet and inflammation Leptin TNF alpha 1.Progression of chronic renal disease 2.Urea production and excretion 3.Nutritional status 4.Inflammation 5.Dyslipidemia 6.Insulin resistance 7.Mineral and bone disease From 1.05 to 0.68 g protein /kg/d 8.Acidosis, anemia and blood pressure 9.Compliance 10.Evidence 11.Implementation 12.Future directions Kozlowska et al, Nephrology 2004 Improvement in insulin resistance OGT Protein intake After 3 months at 0.3 g/kg/d + ketoanalogues decreased from 1 g/kg/d to 0.3 g + Insulin clamp ketoacids during 4 Serum glucose months insulinemia Improvement in serum glucose and insulinemia (after OGT) Adipocyte ? Gin et al. Metabolism 1987 Rigalleau et al. Am J Clin Nutr 1997 Agenda Phosphate and bone 1.Progression of chronic renal disease • Hyperphosphatemia is independently 2.Urea production and excretion associated with mortality even before dialysis 3.Nutritional status 4.Inflammation • Hyperparathyroidism starts around 60 ml/min 5.Dyslipidemia • Phosphate is strongly bound to protein: 6.Insulin resistance 100 g protein = 1300 mg phosphate 7.Mineral and bone disease 8.Acidosis, anemia and blood pressure • FGF 23 is « the new player » 9.Compliance 10.Evidence 11.Implementation 12.Future directions 6
21/02/2012 Reduction in oral phosphate load Fibroblast Growth Factor 23 From 15 to 8 mg/kg/d (a regular intake is 1500 mg/d) � Hormone synthezised by the bone (osteocyte) � Strong modulator of renal phosphate excretion � Strongly reduces 1-25 Vit D � Increases with CKD worsening (x10 to 1000) � Associated with increased mortality in dialysis Rigalleau et al. Am J Clin Nutr 1997 FGF 23 and renal function FGF 23, mortality and renal death HOST study 1099 stage IV CKD mortality Mean Fup 3 yr renal death Isakova et al. Kidney Int 2011;79:1370 Kendrick et al. JASN, on line Sept 2011 FGF 23: modulated by nutrients FGF 23: modulated by phosphate/protein intake Phosphate intake, 800 mg/d, either from meat or vegetarian 29 healthy volunteers (randomized cross over) 3 different phosphate intakes: • Normal • Oral binder • Supplement of 1500 mg/d Ferrari et al. J Clin Endocrinol Metab 2005 Moe et al. C JASN 2011;6:257 7
21/02/2012 Modulating phosphate/FGF23 by binders Artery stifness / FGF23 / binders 8-wk RCT in 100 CKD patients Ca acetate vs sevelamer Am J Kidney Dis 2012;59:177 J Renal Nutr 2011:21:285-294 Agenda Warning: Risk of low energy intake Warning: Risk of low energy intake Results from large CKD trials kcal/kg/d kcal/kg/d 1.Progression of chronic renal disease 2.Urea production and excretion 3.Nutritional status 4.Inflammation 5.Dyslipidemia 6.Insulin resistance 7.Mineral and bone disease 8.Acidosis, anemia and blood pressure 9.Compliance 1988 1988 1993 1993 1996 1996 10.Evidence MDRD start MDRD end HEMO start 11.Implementation 12.Future directions 8
Recommend
More recommend