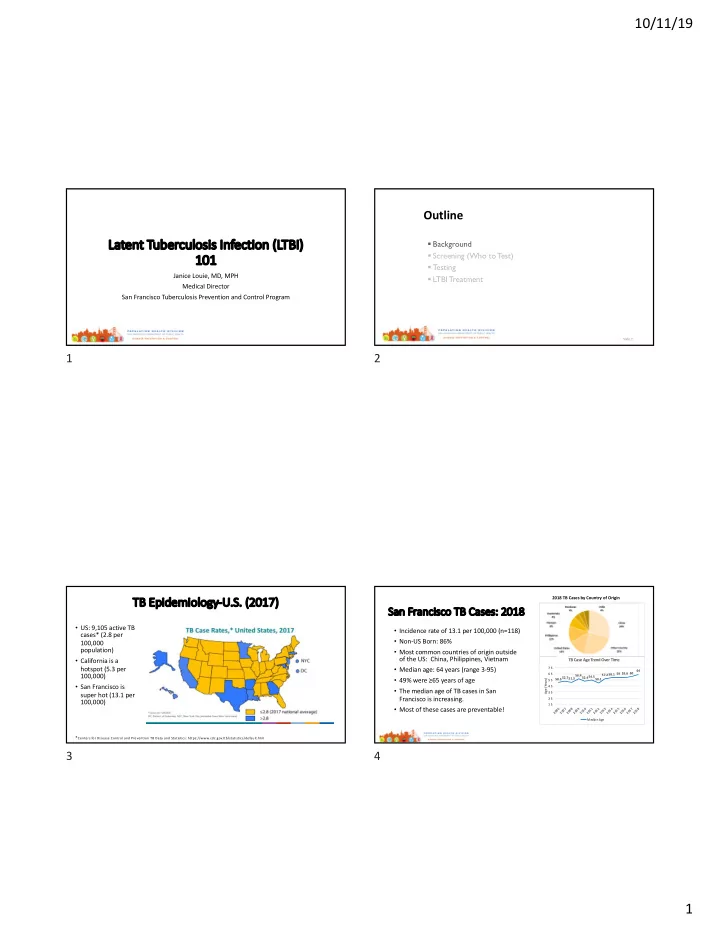
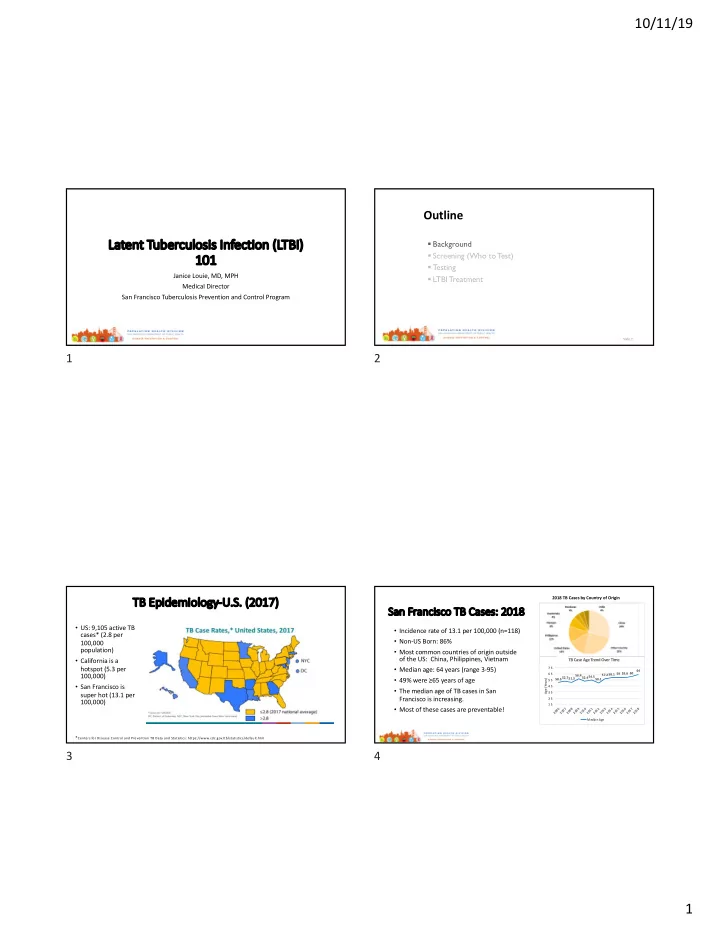
10/11/19 Outline La Laten ent t Tuber ubercul ulosis Infec ecti tion n (LTBI BI) § Background 101 101 § Screening (Who to T est) § T esting Janice Louie, MD, MPH § LTBI Treatment Medical Director San Francisco Tuberculosis Prevention and Control Program Slide 2 1 2 TB TB Epi Epidem demiology gy-U. U.S. (2017) 2018 TB Cases by Country of Origin Sa San Franci cisco o TB Cases: 2018 • US: 9,105 active TB • Incidence rate of 13.1 per 100,000 (n=118) cases* (2.8 per • Non-US Born: 86% 100,000 population) • Most common countries of origin outside of the US: China, Philippines, Vietnam • California is a TB Case Age Trend Over Time hotspot (5.3 per • Median age: 64 years (range 3-95) 7 5 64 100,000) 6 5 57.258.1 59 59.6 60 56.452.454.550.1 • 49% were ≥65 years of age 50.352.751.3 Age (Years) 5 5 • San Francisco is 4 5 • The median age of TB cases in San super hot (13.1 per 3 5 Francisco is increasing. 2 5 100,000) 1 5 • Most of these cases are preventable! 0 6 0 7 0 8 0 9 1 0 1 1 1 2 1 3 1 4 1 5 1 6 1 7 1 8 2 0 2 0 2 0 2 0 2 0 2 0 2 0 2 0 2 0 2 0 2 0 2 0 2 0 Me di a n Age * Centers for Disease Control and Prevention TB Data and Statistics: https://www.cdc.gov/tb/statistics/default.htm 3 4 1
10/11/19 ~2 ~2.4 m million C Californians w with th l latent T t TB i infecti tion- He Health h di dispa parity in n TB: API San n Franc nciscans ns most are unaware and untreated 2.5 U.S.-born 2.0 Foreign-born Millions of persons Estimated 65,111 1.5 San Franciscans with LTBI 1.0 1.8M (2017, CDPH TBCB Report) 0.5 20% 12% 0.0 LTBI preva lence Aware of LTBI Treat ed f or LTBI The TB case-rate in Asian-Americans is 10.8X that in Non-Hispanic White populations NHANES 2011-2012 applied to California population 6 5 6 TB TB Disease vs. (Latent) Tuberculosis Infection (LTB TBI) Natur Na ural History y of TB TB Active TB disease Latent TB infection Not infected 5-10% over lifetime, depending on risk factors Cough, fever, weight loss, No symptoms night sweats Active TB Exposure to Latent TB (LTBI) years infectious (Dormant or “sleeping”) disease Abnormal chest x-ray Normal chest x-ray TB Infectious Not infectious May progress to active TB Rapidly develop disease active TB disease (~1-5%) - Children <5 years - Immunocompromised/HIV - Recent converters Slide 7 8 7 8 2
10/11/19 Outline • Background • Screening (Who To Test) • Testing • LTBI Treatment 9 10 Risk of false positives is high in a low incidence population 11 12 3
10/11/19 Note: Age not considered in this assessment, however younger adults have more years of expected life. Some clinicians may choose to 86% of TB cases prioritize younger non-US in SF are non-US born persons born. Countries of origin for most cases outside of US include: China, Routine testing of Philippines and persons without HIV patients have Vietnam. risk factors is not exceptionally high rate recommended of reactivation (7-10% and may result in per year); screen unnecessary annually evaluation and treatment because of false positive results 13 14 Radiog Ra ographic c lesion ons “con onsistent t with th inacti ctive TB” TB • Risk of developing active TB is Watch out! Patients with up to 19-fold higher abnormal CXR and report that says “lesions • TST or IGRA may be negative consistent with old TB, no • Check sputa and await culture evidence of active TB” results before starting LTBI treatment • Data still unclear on what are best regimens o At SFDPH we use INH+ RIF x 4 months or INH x 9 months 15 16 4
10/11/19 Culture results LTBI with abnormal chest X-ray: 3 cases Å Yes, Active TB, pan-sensitive A A • Non- US born • Asymptomatic • QFT+ • CXR report: “BUL nodules, calcified, consistent with old granulomatous disease. No active disease.” B Å No, TB 4 (old granulomatous B What do you do? disease, LTBI treatment with INH and rifampin) Check sputa! Sputa preliminary results: • Smear neg x 3, geneXp neg x 1 C C • Await cultures (8 weeks) Å Yes, Active TB, pan-sensitive 17 18 Pathophysiology of TB lesions: a dynamic state A radiographic interpretation of “old” TB on chest X- ray does NOT rule out active disease 19 20 5
10/11/19 Ri Risk Fact ctor ors for or Develop oping Acti Active TB 21 22 Outline • Children <5 years at high risk of disseminated TB/TB meningitis • Active TB in children is usually pauci-bacillary: § Background - Asymptomatic or atypical § Screening (Who to T est) symptoms - CXR abnormalities non- § T esting specific: look for infiltrate in lower lobes, mediastinal § LTBI Treatment lymphadenopathy - Sputum typically non- diagnostic, need gastric aspirates x 3 (geneXp often not available) - Exposure history important - Infants and children <5 yrs are “sentinels of transmission” 23 24 6
10/11/19 Tu Tuberculin Skin Testing 25 26 Ca Califor ornia TST interpretati tion on guidelines > 5 mm of induration > 10 mm of induration* Considered positive in: Considered positive in all other persons • Persons with HIV or immunosuppression recommended for TB screening • Recent contacts to an active case of pulmonary or laryngeal TB • Persons with fibrotic changes on chest X-ray consistent with old TB 27 28 7
10/11/19 History of BCG vaccination ESAT-6, CFP-10, and proprietary CD8 antigens (absent from all BCG strains and from most nontuberculous mycobacteria with the exception of M. kansasii , M. szulgai , and M. marinum) 29 30 Repeat testing provided valid result (positive or negative) in 68% (Banach Int Jl TB Lung Dis 2011) 31 32 8
10/11/19 73% false positive rate 12% false positive rate 33 34 Outline § Background § Screening (Who to T est) § T esting § LTBI Treatment 35 36 9
10/11/19 LT LTBI Treatment Options Fi First Line: e: Rifam ampin Normal CXR Multi-center Phase 3 RCT: N= 3443 • Rifampin x 4 months Rifampin x 4 months vs INH x 9 months • INH + rifapentine x 3 months Study sites: Australia, Canada, Benin, Brazil, Ghana, Guinea, Indonesia, Korea, • INH x 6 months Saudi Arabia Findings: • INH x 9 months (gold standard)- immunocompromised/HIV • Rifampin x 4 months was non- inferior to INH x 9 months for the prevention of active TB at 28 months of follow-up TB-4 (Radiographic evidence of old TB disease) Higher rate of treatment completion • Lower rate of adverse events and • INH + Rifampin x 4 months* • hepatotoxicity *Jasmer et al. Twelve months of isoniazid compared with four months of isoniazid and rifampin for persons with radiographic evidence of previous tuberculosis: an outcome and cost- effectiveness analysis. Am J Respir Crit Care Med 2000 Nov;162(5):1648-52. 37 38 39 40 10
10/11/19 First Line: 3-HP by Directly Observed Therapy 41 42 Self Adm Sel dmini nister ered ed-3H 3HP Prevent TB Study Multi-center RCT (n=8053) • Recommended by CDC June 2018* • Based on study of 1000+ adults in Denver, median age 36 years 3HP DOT x 12 weeks vs INH x 9 • SFDPH protocol: months Inclusion criteria: o All adults, who upon mutual assessment by MD and nursing, can be compliant Study Sites: U.S., Canada, Brazil o Children <18 years who are able to swallow pills (without crushing) and can be monitored by and Spain a parent Exclusion criteria: 3HP was non-inferior to INH x • o Any patient who requires DOPT 9 months for the prevention of active TB at 33 months of o Any adult where noncompliance is a concern follow-up o Children who need crushed pills or liquid formulations Higher rate of treatment • o Children (including adolescents and teenagers) where parents do not agree or are unable to completion monitor compliance Lower rate of hepatotoxicity • * MMWR Weekly / June 29, 2018 / 67(25);723–726 43 44 11
10/11/19 Second line- Isoniazid x 6 months Second line- Isoniazid x 9 months (Use when rifamycin is not tolerated or contra-indicated) Recommended for immunocompromised/HIV *But increased hepatoxicity “52 weeks of INH prevented the most tuberculosis, but 24 weeks prevented the most as duration of INH increases tuberculosis per case of hepatitis caused.” 45 46 Monthly Mo Mo Monitoring Isonia Is iazid id Adverse Events • Adherence • Hepatitis • Symptoms: • Uncommon in age <20 years o Fatigue, anorexia, nausea/vomiting, abdominal pain • Increased risk with older age: ~2% in ages 50-64 years o Icterus, jaundice, dark urine • Increased risk with ETOH abuse or chronic liver disease o Rash, itchiness • Asymptomatic transaminitis (20%) o Peripheral numbness • LFTS: • Peripheral neuropathy (<0.2%); supplement with B6 50 mg o History of liver disease or ETOH use • Rash o HIV Hold medications if: • Mild CNS effects o Pregnancy/post-partum (<3 months) • Symptomatic and LFTS >3X ULN • Note drug interactions: increase Dilantin, carbamazepine and o Other hepatotoxic meds (e.g. statins) • Asymptomatic and LFTS >5X ULN o Age> 50 Antabuse levels ATS/CDC LTBI Guidelines 2000 47 48 12
Recommend
More recommend