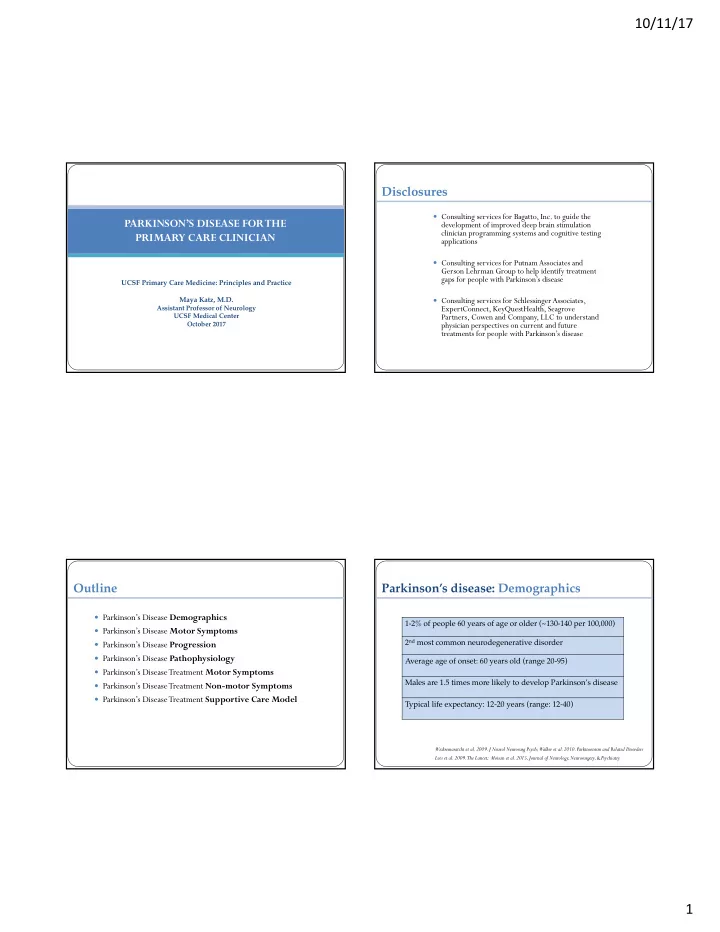
10/11/17 Disclosures Consulting services for Bagatto, Inc. to guide the PARKINSON’S DISEASE FOR THE development of improved deep brain stimulation clinician programming systems and cognitive testing PRIMARY CARE CLINICIAN applications Consulting services for Putnam Associates and Gerson Lehrman Group to help identify treatment gaps for people with Parkinson’s disease UCSF Primary Care Medicine: Principles and Practice Maya Katz, M.D. Consulting services for SchlessingerAssociates, Assistant Professor of Neurology ExpertConnect, KeyQuestHealth, Seagrove UCSF Medical Center Partners, Cowen and Company, LLC to understand October 2017 physician perspectives on current and future treatments for people with Parkinson’s disease Outline Parkinson’s disease: Demographics Parkinson’s Disease Demographics 1-2% of people 60 years of age or older (~130-140 per 100,000) Parkinson’s Disease Motor Symptoms 2 nd most common neurodegenerative disorder Parkinson’s Disease Progression Parkinson’s Disease Pathophysiology Average age of onset: 60 years old (range 20-95) Parkinson’s Disease Treatment Motor Symptoms Males are 1.5 times more likely to develop Parkinson’s disease Parkinson’s Disease Treatment Non-motor Symptoms Parkinson’s Disease Treatment Supportive Care Model Typical life expectancy: 12-20 years (range: 12-40) Wickremaratchi et al. 2009. J Neurol Neurosurg Psych; Walker et al. 2010. Parkinsonism and Related Disorders Lees et al. 2009. The Lancet; Moisan et al. 2015, Journal of Neurology, Neurosurgery, & Psychiatry 1
10/11/17 Cardinal motor symptoms: Tremor Cardinal motor symptoms: Bradykinesia Parkinson’s disease progression: Motor Fluctuations Cardinal motor symptoms: Gait Impairment OFF MEDICATIONS ON MEDICATIONS 2
10/11/17 Parkinson’s disease progression: Parkinson’s disease progression: Dyskinesias Motor Fluctuations Cenci, 2014, Frontiers Neurology Parkinson’s disease progression: Parkinson’s pathology: Hoehn & Yahr staging Substantia nigra pars compacta degeneration Stage 1: ~2 years Stage 3: ~2 years Unilateral involvement Mild to moderate bilateral involvement, Postural instability, Stage 2: ~7 years Still independent Mild bilateral involvement Parkinson’s disease Normal Scarr et al., 2013, Front. Cell. Neurosci. UCSF Department of Pathology Stage 4: ~2 years Stage 5: ~2 years Severe disability, Wheelchair bound or bedridden Needs an assistive device to Can only ambulate with another person assisting walk or stand Zhao et al. 2010, Mov Disord 3
10/11/17 Parkinson’s pathology: Lewy body Parkinson’s pathology: prion-like disease Olanow and Brundin, 2013, Movement Disorders Parkinson’s pathology: DaTSCAN Parkinson’s pathology: Rate model The basal ganglia has 2 major pathways: Direct and Indirect The direct pathway facilitates movement. • The indirect pathway inhibits movement • Striatal dopamine excites the direct pathway • DaTSCANs detect presynaptic dopaminergic § (increasing movement), and suppresses the neuronal loss using SPECT imaging indirect pathway (increasing movement) § Measures Ioflupane ( 123 I), which is a DAT ligand that binds to presynaptic dopamine transporters in the striatum de la Feunte-Fernandez 2012. Neurology Calabresi et al. 2014, NatureNeuroscience Ba and Martin, 2015, Parkinsonism and Related Disorders 4
10/11/17 Parkinson’s etiology: Parkinson’s pathology: Brain arrhythmia gene-environment interaction • Complex interplay between Phase amplitude coupling genetics (ingredients) • Increased bursting of environment (recipe) • neuronal activity Increased synchronization in neuronal activity Increased oscillatory activity de Hemptinne et al. 2013, PNAS Tanner et al. 2011, Envi Health Perspectives Treatment for Parkinson’s Disease Motor Symptoms: Treatment for Parkinson’s Disease Motor Symptoms: Medications Medications Carbidopa/Levodopa: Carbidopa/Levodopa: Effects Formulations Short half-life (45-90 minutes) Sinemet IR Orally disintegrating tablets, The most effective and generally well-tolerated medicine for PD not sublingually absorbed, similar time to Parcopa peak concentration compared to sinemet IR Short half-life (~45 to 90 minutes), needs to be taken frequently as PD progresses ~60 minutes increased sustained concentration compared to sinemet IR, Sinemet CR Ideally should be taken 1 hour before or 2 hours after a protein-rich meal impaired bioavilability, lower peak dose, time to peak concentration can be up to 120 minutes longer than sinemet IR Main side effects: nausea, lightheadedness, hallucinations, and dyskinesias Rytary ~2 to 2.5 hours increased sustained concentration compared to sinemet IR 5
10/11/17 PD Treatment: Medications PD Treatment: Medications Carbidopa/Levodopa: Carbidopa/Levodopa ER: Dosing Guidelines (Rytary) Start with sinemet 25/100mg IR: ½ tab three times per day Dosing Guidelines Increase to sinemet 25/100mg IR: 1 tab three times per day after 2 weeks Increase to sinemet 25/100mg IR: 1.5 tabs three times per day after 2 weeks Increase to sinemet 25/100mg IR: 2 tabs three times per day after 2 weeks Instruct patients to increase the dose of sinemet only if motor symptoms are not well controlled on the lower dose Can ultimately increase the dose up to 3.5 tabs per dose, if needed No maximum total daily dose, based on need and tolerance Advanced PD patients may take sinemet every 90 minutes Treatment for Parkinson’s Disease Motor Symptoms: Treatment for Parkinson’s Disease Motor Symptoms: Medications Medications Carbidopa/Levodopa Extenders: Dopamine Agonist: Effects Effects 1 hour increased on-time Compared to carbidopa/levodopa Rasagaline (Azilect) Side effects: drug interactions Lasts longer, half-life: ~6 hours Lower risk of causing dyskinesias 1 hour increased on-time Selegiline (Eldepryl) More mild benefit Side effects: drug interactions, HTN, insomnia, delirium 1 hour increased on-time Main side effects: sleep attacks, ICDs, sedation, confusion, hallucinations, Entacapone (Comtan) Side effects: diarrhea, orange urine cognitive deficits, dry mouth, lightheadedness 2-3 hours increased on-time Tolcapone (Tasmar) Usually not prescribed to people over 70 years of age Side effects: Liver failure 6
10/11/17 Treatment for Parkinson’s Disease Motor Symptoms: Treatment for Parkinson’s Disease Motor Symptoms: Medications Medications Levodopa sparing therapy: Levodopa sparing therapy: Effects Effects Mild-moderate reduction in parkinsonism Side effects: ICD, sleep attacks, Dopamine agonists MAO-B inhibitors Very mild reduction in parkinsonism, if any hallucinations, cognitive deficits Side effects: drug interactions, depends on whether rasagaline or selegiline are used Reduces tremor, mild benefit Side effects: nephrolithiasis, somnolence, Zonisamide ataxia, confusion, cognitive deficits Mild reduction in parkinsonism, Reduces tremor and dystonia Amantadine Reduces dyskinesias Side effects: sedation, delirium, Trihexyphenidyl Side effects: confusion, hallucinations, hallucinations, increased risk of dementia, dry mouth, constipation, dry mouth, constipation Treatment for Parkinson’s Disease Motor Symptoms: Treatment for Parkinson’s Disease Motor Symptoms: Risk of developing dyskinesias Medication Tips § Prochlorperazine (Compazine) § CALM-PD Clinical Trial Dosing Percentage developing Improvement in § Promethazine (Phenergan) strategy dyskinesia after 2 years movement and function scale (UPDRS) § Metoclopramide (Reglan) Pramipexole 10% 4.5 points § Most anticholinergics (e.g. benadryl or oxybutynin) Levodopa 30% 9.2 points § Most antipsychotics (only quetiapine, clozaril and pimavanserin are safe) CALM-PD PSG Study Group, 2000, JAMA 7
10/11/17 Treatment for Parkinson’s Disease Motor Symptoms: Treatment for Parkinson’s Disease Motor Symptoms: REHABILITATION REHABILITATION OUTPATIENT PHYSICAL THERAPY HOME SAFETY EVALUATION • Parkinson Wellness Recovery (PWR!) • skilled nursing • Lee Silverman Voice Training (LSVT) • physical therapy • Balance vest • occupational therapy • custodial non-skilled care Treatment for Parkinson’s Disease Motor Symptoms: Treatment for Parkinson’s Disease Motor Symptoms: REHABILITATION FREEZING OF GAIT NON-PHARMACOLOGICAL TREATMENTS MEDICARE COVERS 'SKILLED MAINTENANCE’ • Reduce multi-tasking to reduce freezing episodes Medicare covers rehab services to maintain or manage a patient’s current condition • • During a freezing episode: come to a complete stop (to abort the malfunctioning when no functional improvement is possible automatic gait program causing the freezing episode) • Then try any of the following techniques: • Therapy services to maintain a patient’s current condition or slow decline are covered • Count to 3 and take a large high step with one foot. • Try another movement (e.g. raise an arm, touch your head) and then restart walking • Turn in a U-shape • Change direction: step sideways and then go forward • Weight-shifting from side to side • Step over a target (e.g. a laser pointer using U-step walker/cane) • Metronome or musical cueing • Stress-reduction techniques to minimize emotional triggers of freezing episodes 8
Recommend
More recommend