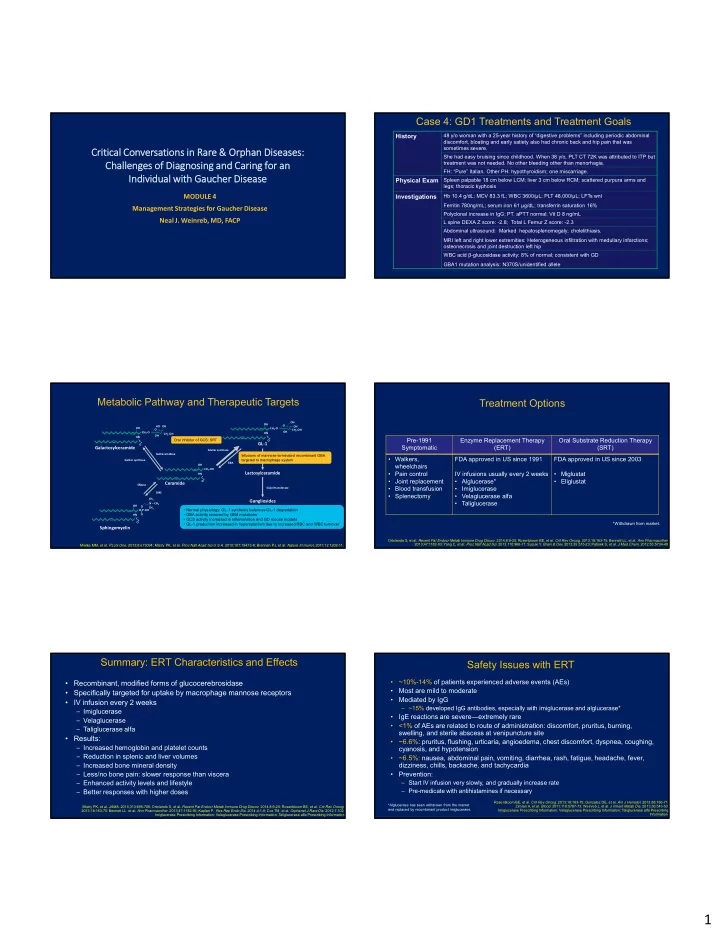
Case 4: GD1 Treatments and Treatment Goals History 48 y/o woman with a 25-year history of “digestive problems” including periodic abdominal discomfort, bloating and early satiety also had chronic back and hip pain that was sometimes severe. Critical Conversations in Rare & Orphan Diseases: She had easy bruising since childhood. When 38 y/o, PLT CT 72K was attributed to ITP but treatment was not needed. No other bleeding other than menorhagia. Challenges of Diagnosing and Caring for an FH: “Pure” Italian. Other PH: hypothyroidism; one miscarriage. Individual with Gaucher Disease Physical Exam Spleen palpable 18 cm below LCM; liver 3 cm below RCM; scattered purpura arms and legs; thoracic kyphosis MODULE 4 Investigations Hb 10.4 g/dL; MCV 83.3 fL; WBC 3600/µL; PLT 48,000/µL; LFTs wnl Ferritin 780ng/mL; serum iron 61 µg/dL; transferrin saturation 16% Management Strategies for Gaucher Disease Polyclonal increase in IgG; PT, aPTT normal; Vit D 8 ng/mL Neal J. Weinreb, MD, FACP L spine DEXA Z score: -2.8; Total L Femur Z score: -2.3 Abdominal ultrasound : Marked hepatosplenomegaly; cholelithiasis. MRI left and right lower extremities: Heterogeneous infiltration with medullary infarctions; osteonecrosis and joint destruction left hip WBC acid β-glucosidase activity: 8% of normal; consistent with GD GBA1 mutation analysis: N370S/unidentified allele Metabolic Pathway and Therapeutic Targets Treatment Options OH OH O HO OH OH OH CH 2 ‐O O CH 2 ‐OH OH CH 2 ‐O CH 2 ‐OH HN OH HN C Pre-1991 Enzyme Replacement Therapy Oral Substrate Reduction Therapy Oral inhibitor of GCS: SRT C O GL‐1 O Symptomatic (ERT) (SRT) Galactosylceramide GluCer synthase GalCeramidase Infusions of mannose-terminated recombinant GBA • Walkers, FDA approved in US since 1991 FDA approved in US since 2003 LacCer synthase GalCer synthase targeted to macrophage system GBA OH wheelchairs CH 2 ‐OH • Pain control IV infusions usually every 2 weeks • Miglustat Lactosylceramide HN C • Joint replacement • Alglucerase* • Eliglustat O Ceramide SMase • Blood transfusion • Imiglucerase Sialyl transferase SMS • Splenectomy • Velaglucerase alfa CH 3 Gangliosides • Taliglucerase N – CH 3 OH O CH 3 • Normal physiology: GL-1 synthesis balances GL-1 degradation O‐P‐OH = • GBA activity reduced by GBA mutations HN O C • GCS activity increased in inflammation and GD mouse models O *Withdrawn from market. • GL-1 production increased in hypersplenism due to increased RBC and WBC turnover Sphingomyelin Ortolando S, et al. Recent Pat Endocr Metab Immune Drug Discov . 2014;8:9-25; Rosenbloom BE, et al. Crit Rev Oncog . 2013;18:163-75; Bennett LL, et al. Ann Pharmacother . 2013;47:1182-93; Yang C, et al. Proc Natl Acad Sci . 2013;110:966-71; Suzuki Y. Brain & Dev. 2013;35:515-23; Patnaik S, et al. J Med Chem . 2012;55:5734-48 . Mielke MM, et al. PLoS One . 2013;8:e73094; Mistry PK, et al. Proc Natl Acad Sci U S A . 2010;107:19473-8; Brennan PJ, et al. Nature Immunol , 2011;12:1202-11. Summary: ERT Characteristics and Effects Safety Issues with ERT • ~10%-14% of patients experienced adverse events (AEs) • Recombinant, modified forms of glucocerebrosidase • Most are mild to moderate • Specifically targeted for uptake by macrophage mannose receptors • Mediated by IgG • IV infusion every 2 weeks – ~15% developed IgG antibodies, especially with imiglucerase and alglucerase* – Imiglucerase • IgE reactions are severe—extremely rare – Velaglucerase • <1% of AEs are related to route of administration: discomfort, pruritus, burning, – Taliglucerase alfa swelling, and sterile abscess at venipuncture site • Results: • ~6.6%: pruritus, flushing, urticaria, angioedema, chest discomfort, dyspnea, coughing, – Increased hemoglobin and platelet counts cyanosis, and hypotension – Reduction in splenic and liver volumes • ~6.5%: nausea, abdominal pain, vomiting, diarrhea, rash, fatigue, headache, fever, – Increased bone mineral density dizziness, chills, backache, and tachycardia – Less/no bone pain: slower response than viscera • Prevention: – Enhanced activity levels and lifestyle – Start IV infusion very slowly, and gradually increase rate – Better responses with higher doses – Pre-medicate with antihistamines if necessary Rosenbloom BE, et al. Crit Rev Oncog. 2013;18:163-75; Gonzalez DE, et al. Am J Hematol . 2013;88:166-71; *Alglucerase has been withdrawn from the market Mistry PK, et al. JAMA . 2015;313:695-706; Ortolando S, et al. Recent Pat Endocr Metab Immune Drug Discov . 2014;8:9-25; Rosenbloom BE, et al. Crit Rev Oncog . Zimran A, et al. Blood . 2011;118:5767-73; Weinreb J, et al. J Inherit Metab Dis. 2013;36:543-53; and replaced by recombinant product imiglucerase. Imiglucerase Prescribing Information; Velaglucerase Prescribing Information; Taliglucerase alfa Prescribing 2013;18:163-75; Bennett LL, et al. Ann Pharmacother . 2013;47:1182-93; Kaplan P. Res Rep Endo Dis . 2014;4:1-8; Cox TM, et al. Orphanet J Rare Dis. 2012;7:102; Imiglucerase Prescribing Information; Velaglucerase Prescribing Information; Taliglucerase alfa Prescribing Information Information. 1
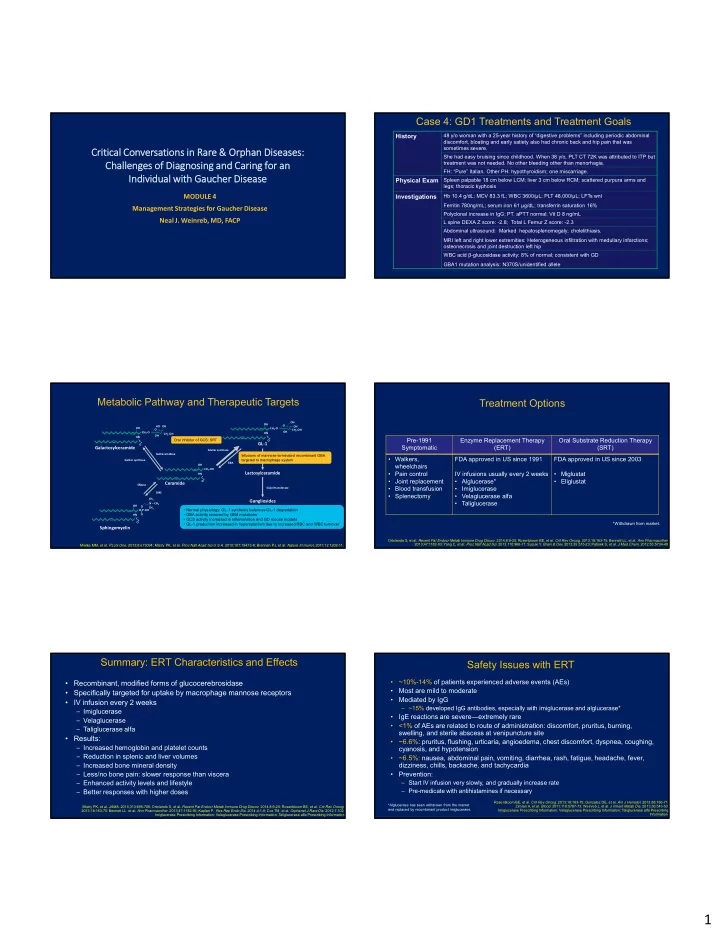
Limitations of ERT Oral GL-1 Synthase Inhibitor Therapy (SRT) Miglustat • Invasive and sometimes inconvenient or unavailable • Ineffective for neuronopathic GD • Iminosugar that resembles glucose moiety of GL-1 • Not proven to prevent GD-associated Parkinsonism or malignancies • Incomplete control of macrophage activation effects: • Efficacy: demonstrated non-inferiority in maintaining liver volume; also • Cytokines maintained spleen volume, hemoglobin concentration, and platelet count in • T and B cell stimulation patients stable on ERT switching to miglustat • Inflammatory manifestations including coagulation activation • Incomplete control of skeletal manifestations: • FDA approved for patients with mild/moderate GD1 for whom ERT is not an • Marrow infiltration option • Bone mineral loss (osteopenia/osteoporosis) • Osteonecrosis and fractures • Common AEs: GI issues, tremors, and weight loss • Requires low-carbohydrate diet to minimize GI side effects Probabilities of living free without a new episode of avascular necrosis, fracture, or lytic bone lesion with enzyme replacement treatment 1.0 0.8 Probability Survival 0.6 0.4 DS3 > 6 DS3 3-6 0.2 DS3 < 3 0.0 0 5 10 15 20 Year Weinreb NJ, et al. Orphanet J Rare Dis . 2015;10:64. Weinreb NJ, et al. Am J Hematol . 2005;80:223-9; Cox T, et al. Lancet. 2000;355:1481-5; Miglustat Prescribing Information.. ENGAGE: Long-Term Hematologic and Visceral Improvements at Eliglustat Clinical Trials 4.5 Years in Previously Untreated Individuals with GD1 • The largest clinical trial program ever in GD 2.5 100 Platelets + 87% Mean ± SEM • Conducted over 14 years 2 80 Change in Hemoglobin, g/dL Hemoglobin +1.4 g/dL % Change from Baseline • Included 395 patients in 34 countries 1.5 60 1 • Represents 1,400 patient-years of eliglustat exposure 40 0.5 20 • First to include a placebo-controlled phase 3 trial 0 0 Liver volume ‐23% ‐0.5 ‐20 ‐1 ‐40 Spleen volume ‐67% ‐1.5 ‐60 ‐2 ‐80 0 0.5 1 1.5 2 2.5 3 3.5 4 4.5 5 (N = 40) (n = 39) (n = 38‐39) (n = 32‐35) (n = 21‐28) (n = 12‐13) Time on Eliglustat, years Lukina E, et al. Blood . 2010;116:893-9; Lukina E et al. Blood . 2010;116:4095-8; Lukina E, et al. Blood Cells Mol Dis . 2014;53:274-6; Clinicaltrials.gov (NCT00358150). Peterschmitt MJ, et al. ICIEM 2017. Poster 689; Mistry PK, et al. WORLD Symposium 2017. Points to Remember About GD Treatment Eliglustat ENGAGE Trial: Changes in BMD and BMB After 4.5 Years in Treatment-Naïve Patients • ERT effectively ameliorates most symptom-causing manifestations of GD1 in adults and children, including splenomegaly, hepatomegaly, thrombocytopenia, anemia, bone crises, and chronic bone pain caused by GD1. 11 0 10.5 Mean Total BMB Score ‐0.2 • Imiglucerase, velaglucerase, and taliglucerase appear to be similar in efficacy and safety. 10 There is no evidence for either superiority or inferiority to support a decision about which ‐0.4 9.5 ‐0.5 ERT to recommend. However, there are molecular differences, especially in glycosylation, 9 ‐0.6 8.5 that might impact efficiency of cellular uptake, transcriptome response in tissues and ‐0.8 8 ‐1 antigenicity. 1 7.5 ‐1 7 Total BMB Score ‐1.2 • Of the 2 oral SRTs (miglustat, eliglustat), eliglustat appears to have efficacy that is more 6.5 Spine T‐Score ‐1.5 similar to that of the ERTs and can be prescribed for some treatment-naïve adult patients 6 ‐1.4 I I I I I I 0 0.75 1.5 2.5 3.5 4.5 and for some patients currently or previously treated with ERT. 2 (n = 40) (n = 34, 39) (n = 33, 38) (n = 27, 31) (n = 18, 19) (n = 9, 10) Time on Eliglustat, years • Eliglustat has a more favorable GI side-effect profile than miglustat. 2 • Study design: Phase 3, placebo-controlled, randomized • Population: adults with GD1 (N=40); duration: 9 months 1. Brumshtein B, et al. Glycobiology. 2010;20:24-32; Tekoah Y, et al. Biosci Rep. 2013;33:pii:e00071; Dasgupta N, et al. PLoS One . 2013;8:e74912; 2. Mistry PK, et al. Blood Cells Mol Dis. 2018;71:71-4 Mistry PK, et al. JAMA . 2015;313:695-706; Mistry PK, et al. WORLD Symposium 2017; Mistry PK, et al . Mol Genet Metab. 2016:120:s97. 2
Recommend
More recommend