1 Reason Ischemic heart disease causes the greatest number of - PDF document
12 Lead Electrocardiogram (ECG) PFN: SOMACL17 JSOMTC, SWMG(A) Slide 1 Terminal Learning Objective Action: Communicate knowledge of 12 Lead Electrocardiogram (ECG) Condition: Given a lecture in a classroom environment Standard: Received
12 Lead Electrocardiogram (ECG) PFN: SOMACL17 JSOMTC, SWMG(A) Slide 1 Terminal Learning Objective Action: Communicate knowledge of 12 Lead Electrocardiogram (ECG) Condition: Given a lecture in a classroom environment Standard: Received a minimum score of 84% on the written exam IAW course AHA standards JSOMTC, SWMG(A) Slide 2 References Advanced Cardiovascular Life Support, Provider Manual 2010 The 12 lead ECG in Acute Myocardial Infarction 1996 The 12 lead ECG for Acute and Critical Care Providers 2005 JSOMTC, SWMG(A) Slide 3 1
Reason Ischemic heart disease causes the greatest number of deaths in the United States. 50% die before arriving at a hospital. If treatment is not received within 2 hours of onset of symptoms, chance of survival is 25%. By treating a heart attack within one hour of onset of symptoms, the chance of survival is 49%! JSOMTC, SWMG(A) Slide 4 Reason The keys to quick management of an acute myocardial infarction (AMI) patient are: Prompt recognition of the symptoms Rapid performance and interpretation of a 12 Lead ECG Provide pre ‐ arrival notification to the receiving facility JSOMTC, SWMG(A) Slide 5 Agenda Recall the pathophysiology of acute myocardial infarction (AMI) Identify the electrode placement for a 12 Lead ECG Identify the 12 Lead ECG physiology to assess an AMI Identify an AMI using a 12 Lead ECG JSOMTC, SWMG(A) Slide 6 2
Agenda Identify the limitations and complications of recognizing an AMI using a 12 Lead ECG Participate in a 12 Lead ECG interpretation practical exercise JSOMTC, SWMG(A) Slide 7 Pathophysiology of Acute Myocardial Infarction (AMI) JSOMTC, SWMG(A) Slide 8 Pathophysiology of AMI A heart attack occurs when a thrombus or blood clot forms in a coronary artery, cutting off the blood supply to a segment of the heart muscle. Prompt restoration of blood flow can stop and minimize (or even prevent) the heart damage. JSOMTC, SWMG(A) Slide 9 3
Pathophysiology of AMI The blood flow can be restored by: Percutaneous coronary intervention (PCI) Coronary artery bypass graft (CABG) Administration of a clot dissolving (thrombolytic) drug JSOMTC, SWMG(A) Slide 10 Pathophysiology of AMI ACS symptom review: Crushing chest pain lasting more than 15 minutes Chest Pain spreading to the shoulders, neck, arms or jaw Chest discomfort with lightheadedness, fainting, sweating or nausea Shortness of breath with or without chest discomfort JSOMTC, SWMG(A) Slide 11 Electrode Placement for a 12 Lead ECG JSOMTC, SWMG(A) Slide 12 4
ECG Leads Bipolar Leads I, II, and III Unipolar Leads aVR, aVL, and aVF Precordial V1, V2, V3, V4, V5, and V6 JSOMTC, SWMG(A) Slide 13 12 Lead ECG Preparation JSOMTC, SWMG(A) Slide 14 Bipolar and Unipolar Leads JSOMTC, SWMG(A) Slide 15 5
Precordial Leads JSOMTC, SWMG(A) Slide 16 V1 JSOMTC, SWMG(A) Slide 17 V2 JSOMTC, SWMG(A) Slide 18 6
V4 JSOMTC, SWMG(A) Slide 19 V3 JSOMTC, SWMG(A) Slide 20 V5 JSOMTC, SWMG(A) Slide 21 7
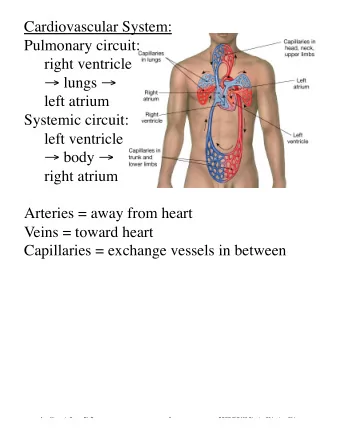
V6 JSOMTC, SWMG(A) Slide 22 12 Lead ECG Electrode Placement JSOMTC, SWMG(A) Slide 23 12 Lead ECG Physiology to Assess an AMI JSOMTC, SWMG(A) Slide 24 8
12 Lead ECG Relationship to Coronary Artery Anatomy Let’s look at the heart Page 28 in the ACLS Handbook The right coronary artery (RCA) supplies oxygen to the inferior (bottom) surface of the heart JSOMTC, SWMG(A) Slide 25 12 Lead ECG Relationship to Coronary Artery Anatomy The left coronary artery (LCA) splits in two: The left anterior descending coronary artery (LAD) The left circumflex coronary artery (LCX or Cx) JSOMTC, SWMG(A) Slide 26 12 Lead ECG Relationship to Coronary Artery Anatomy (cont) JSOMTC, SWMG(A) Slide 27 9
12 Lead ECG Relationship to Coronary Artery Anatomy The left anterior descending coronary artery (LAD) courses down the anterior (front) surface of the heart and supplies oxygen to the septal, anterior, and lateral sides of the heart. JSOMTC, SWMG(A) Slide 28 12 Lead ECG Relationship to Coronary Artery Anatomy (cont) JSOMTC, SWMG(A) Slide 29 12 Lead ECG Relationship to Coronary Artery Anatomy The left circumflex coronary artery (Cx) supplies oxygen to the left lateral (side) surface of the heart. JSOMTC, SWMG(A) Slide 30 10
12 Lead ECG Relationship to Coronary Artery Anatomy (cont) JSOMTC, SWMG(A) Slide 31 12 Lead ECG Relationship to Coronary Artery Anatomy JSOMTC, SWMG(A) Slide 32 12 Lead ECG Relationship to Coronary Artery Anatomy (cont) I lateral aVR V 1 septal V 4 anterior II inferior aVL lateral V 2 septal V 5 lateral III inferior aVF inferior V 3 anterior V 6 lateral JSOMTC, SWMG(A) Slide 33 11
12 Lead ECG Relationship to Coronary Artery Anatomy JSOMTC, SWMG(A) Slide 34 Identify an AMI Using a 12 Lead ECG JSOMTC, SWMG(A) Slide 35 Analyze the 12 Lead ECG JSOMTC, SWMG(A) Slide 36 12
Normal 12 Lead ECG JSOMTC, SWMG(A) Slide 37 12 Lead Versus 3 Lead ECG Differences 2.5 second views instead of a 6 second view Legend Views mimic anatomy of the heart JSOMTC, SWMG(A) Slide 38 Identify an AMI Baseline Ischemia—tall or inverted T wave (infarct), ST segment may be depressed (angina) Injury—elevated ST segment, T wave may invert Infarction (Acute)—abnormal Q wave, ST segment may be elevated and T wave may be inverted Infarction (Age Unknown)—abnormal Q wave, ST segment and T wave returned to normal JSOMTC, SWMG(A) Slide 39 13
ECG Recording JSOMTC, SWMG(A) Slide 40 Identify an AMI Know what to look for: Measure from J point J point plus ST elevation or 0.04 second depression > 1 mm 2 anatomical leads Pathologic Q wave greater than 40 ms or greater than 1/3 height of R wave PR baseline ST ‐ segment deviation = 4.5 mm JSOMTC, SWMG(A) Slide 41 ST Segment Elevation Myocardial Infarctions (STEMIs) Acute Anterior Wall Infarct Anterolateral Infarct Acute Inferior Wall Infarct JSOMTC, SWMG(A) Slide 42 14
Acute Anterior Wall Infarct JSOMTC, SWMG(A) Slide 43 Anterolateral Infarct JSOMTC, SWMG(A) Slide 44 Acute Inferior Wall Infarct JSOMTC, SWMG(A) Slide 45 15
Limitations and Complications of Recognizing an AMI Using a 12 Lead ECG JSOMTC, SWMG(A) Slide 46 Limitations of 12 Lead ECG 12 Lead ECG: Does not look at the right ventricle of the heart • Acute Right Ventricular Infarct Does not look at the posterior (rear) of the heart • Posterior Wall Infarct Patient can still be having an AMI even if ST elevation is not seen on a 12 lead ECG JSOMTC, SWMG(A) Slide 47 Right Ventricular Infarct JSOMTC, SWMG(A) Slide 48 16
Right Ventricular Infarct Looks just like an inferior infarct Take lead V4 and place it 5th ICS MCL on the right side of the chest RVI suspected if ST elevation is present in that lead Usually this patient is in cardiogenic shock due to a heavy reliance on preload Don’t administer Nitro or Morphine JSOMTC, SWMG(A) Slide 49 Posterior Wall Infarct JSOMTC, SWMG(A) Slide 50 Posterior Wall Infarct ST segment depression is reciprocal of ST segment elevation Taller R wave is reciprocal of pathological Q wave Usually noticed in leads V1, V2, and V3 JSOMTC, SWMG(A) Slide 51 17
Complications of 12 Lead ECG AMI can affect the conduction system of the heart New Left Bundle Branch Block Lethal Dysrhythmias Examples: VF or Pulseless VT Cardiogenic Shock JSOMTC, SWMG(A) Slide 52 Left Bundle Branch Block JSOMTC, SWMG(A) Slide 53 Left Bundle Branch Block JSOMTC, SWMG(A) Slide 54 18
Left Bundle Branch Block Look at the QS complex in V1 QRS > 0.12 seconds Pointing down indicates LBBB JSOMTC, SWMG(A) Slide 55 12 Lead ECG Interpretation Practical Exercise JSOMTC, SWMG(A) Slide 56 Practical Exercise JSOMTC, SWMG(A) Slide 57 19
Questions? JSOMTC, SWMG(A) Slide 58 Terminal Learning Objective Action: Communicate knowledge of 12 Lead Electrocardiogram (ECG) Condition: Given a lecture in a classroom environment Standard: Received a minimum score of 84% on the written exam IAW course AHA standards JSOMTC, SWMG(A) Slide 59 Agenda Recall the pathophysiology of acute myocardial infarction (AMI) Identify the electrode placement for a 12 Lead ECG Identify the 12 Lead ECG physiology to assess an AMI Identify an AMI using a 12 Lead ECG JSOMTC, SWMG(A) Slide 60 20
Agenda Identify the limitations and complications of recognizing an AMI using a 12 Lead ECG Participate in a 12 Lead ECG interpretation practical exercise JSOMTC, SWMG(A) Slide 61 Reason Ischemic heart disease causes the greatest number of deaths in the United States. 50% die before arriving at a hospital. If treatment is not received within 2 hours of onset of symptoms, chance of survival is 25%. By treating a heart attack within one hour of onset of symptoms, the chance of survival is 49%! JSOMTC, SWMG(A) Slide 62 Reason The keys to quick management of an acute myocardial infarction (AMI) patient are: Prompt recognition of the symptoms Rapid performance and interpretation of a 12 Lead ECG Provide pre ‐ arrival notification to the receiving facility JSOMTC, SWMG(A) Slide 63 21
Recommend
More recommend
Explore More Topics
Stay informed with curated content and fresh updates.